Case Report | DOI: https://doi.org/10.31579/2835-785X/006
Treatment of Surgical Gastric Outlet Obstruction from A Large Gastroduodenal Trichobezoar: A Case Report
- Mohammad Aslam *
- Mohd Atif Ansari
- Nafees Ahamad
- Sadiq Husain
- Maikal Kujur
1 Department of General Surgery Jawaharlal Nehru Medical College and Hospital, Aligarh Muslim University, Aligarh, Uttar Pradesh, India 202002
*Corresponding Author: Mohammad Aslam. Department of General Surgery Jawaharlal Nehru Medical College and Hospital, Aligarh Muslim University, Aligarh, Uttar Pradesh, India 202002.
Citation: Mohammad Aslam, Mohd Atif Ansari, Md Nafees Ahamad, Sadiq Husain, Maikal Kujur. (2022). Treatment of Surgical Gastric Outlet Obstruction from A Large Gastroduodenal Trichobezoar: A Case Report. International Journal of Clinical Research and Reports.1(2); DOI:10.31579/2835-785X/006
Copyright: © 2022 Mohammad Aslam, This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 23 September 2022 | Accepted: 20 October 2022 | Published: 01 November 2022
Keywords: left hypochondrium; psychiatric treatment; pharmacobezoar
Abstract
Bezoars are collection of foreign indigestible material accumulating in the gastrointestinal tract leading to intraluminal mass formation that impairs the gastrointestinal motility and can lead to obstruction of the small or the large bowel. These include phytobezoar, lactobezoar, pharmacobezoar, trichobezoar, and polybezoar. A trichobezoar is a mass of undigested hair within the gastrointestinal tract.
Introduction
Bezoars are collection of foreign indigestible material accumulating in the gastrointestinal tract leading to intraluminal mass formation that impairs the gastrointestinal motility and can lead to obstruction of the small or the large bowel. These include phytobezoar, lactobezoar, pharmacobezoar, trichobezoar, and polybezoar. A trichobezoar is a mass of undigested hair within the gastrointestinal tract. Trichobezoars are seen in psychiatric young female with known to be trichophagic [1].Most common site of trichobezoar is the stomach. If trichophagia is not detected earlier then it can develop into Rapunzel Syndrome. Recurrence is overwhelming without psychiatric treatment after the surgery.
Case Presentation
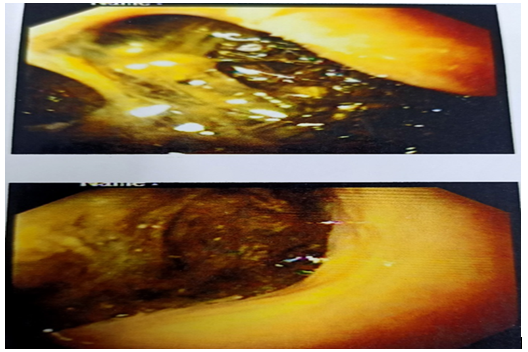
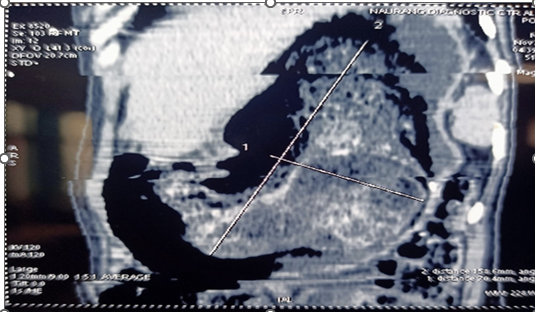
A21-year-old female patient known to be plucking and swallowing hairs for 1 year was admitted to the emergency department for nausea, vomiting, and history of weight loss. On physical examination, patient was having tachycardia and pallor. Per abdominal examination a large, hard mass in the epigastric and left hypochondrium. Complete blood count, electrolytes, kidney function tests, liver function tests, amylase and lipase were normal. Consequently, esophagogastroduodenoscopy (EGD) was done, revealing a collection of a huge hard hairball occupying the entire lumen of the stomach from the fundus through the pylorus reaching the duodenum. (Figure.1) On CECT a large mass measuring 30× 13× 12cm, well defined, multi-layered, inhomogenous, well circumscribed, solid appearing with pockets of air enmeshed within it, non-enhancing mass in the gastric lumen, extending upto proximal jejunum. The lesion was separated from the gastric walls by gastric fluid. No evidence of abnormal gastric mural thickening was noted (Figure. 1).
Case Presentation
Subsequently, midline laparotomy was planned. A 10 cm longitudinal gastrotomy was done on the anterior gastric wall, 8 cm from the pylorus. A large trichobezoar, filling the entire stomach and the duodenum and proximal part of jejunum was extracted (Figure 3).

Discussion:
Trichobezoar is a rare disorder commonly occur in young adult females, with psychiatric problem. The site of hair pulling is most commonly from the scalp, but can occur other hairy areas of body area. [2,3] Trichobezoars in humans were first described from a post mortem by Swain in 1854. Formation in the stomach is that hair is undigestable and due to its smooth nature cannot be propulsed with peristalsis. It leads to the accumulation of hair together with mucus and food, causing the formation of a trichobezoar [4,5]. In most cases, confined within the stomach. However, in some cases, it extends through the pylorus into the jejunum, ileum or even colon. This condition is called Rapunzel syndrome [6]. Affected patients remain asymptomatic for many years. Symptoms develop as the bezoar increases in size .The complications that have been reported over the years include gastric mucosal erosion, ulceration, and gastric outlet obstruction and perforation of the stomach or the small intestine, protein-losing enteropathy , and death . On clinical examination large mobile epigastric mass that may be indentable, the so-called Lamerton’s sign. The most common diagnostic tool used in the is a CT scan, with a typical image showing a well-defined intraluminal ovoid heterogeneous mass with interspersed gas . Management options include endoscopic removal, laparoscopic removal [7], or via laparotomy. Conventional laparotomy is still the treatment of choice depending on the size and site of trichobezoar.
Conclusion
Trichobezoars should be considered as a differential diagnosis in young females with abdominal pain and presence of an upper abdominal mass. Endoscopic or surgical removal can be performed safely and effectively. Psychiatric evaluation and therapy is required to prevent recurrence .
References
- S.Q. Falah, A. (2016) Amanullah, Huge trichobezoar in the stomach of a young female patient, Gomal J. Med. Sci. 14 118–119.
View at Publisher | View at Google Scholar - S.M. Kinoo, B. Singh, (2012) Gastric trichobezoar: an enduring intrigue. Case reports in gastrointestinal, Medicine 1.
View at Publisher | View at Google Scholar - I.S. Al-Janabi, M.A. Al-Sharbaty, M.M. Al-Sharbati, L.A. Al-Sharifi, A. Ouhtit, (2004) Unusual trichobezoar of the stomach and the intestine: a case report, J. Med. Case Rep. 8 79.
View at Publisher | View at Google Scholar - S. Khattak, A. Kamal, Trichobezoar gomal, J. Med. Sci. S. Mewa Kinoo, B. Singh, (2012) Gastric trichobezoar: an enduring intrigue, Case Rep. Gastrointest. Med.
View at Publisher | View at Google Scholar - Obinna Obinwa, David Cooper, Faraz Khan, James M. O’Riordan, (2017) Rapunzel syndrome is not just a mere surgical problem: a case report and review of current management, World J. Clin. Cases 5 (February (2)) 50–55,
View at Publisher | View at Google Scholar - R.R. Gorter, C.M.F. Kneepkens, E.C.J.L. Mattens, D.C. (2010) Aronson, H.A. Heij, Management of trichobezoar: case report and literature review, Pediatr. Surg. Int. 26 457–463,
View at Publisher | View at Google Scholar

 Clinic
Clinic
