Case Report | DOI: https://doi.org/10.31579/2834-5177/010
Transcatheter Embolization of Systemic-to-Pulmonary Artery Fistulas: a Case Report
- Zhang Shen
- Qian Jun *
Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China.
*Corresponding Author: Qian Jun, Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China.
Citation: Zhang Shen, Qian Jun, (2023), Transcatheter Embolization of Systemic-to-Pulmonary Artery Fistulas: a Case Report. International Journal of Clinical Infectious Diseases, 2(1); DOI:10.31579/2834-5177/010
Copyright: © 2023, Qian Jun. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 27 December 2022 | Accepted: 13 January 2023 | Published: 23 January 2023
Keywords: transcatheter embolization; systemic-to-pulmonary artery fistulas; computed tomography scan
Abstract
Background
The systemic artery to pulmonary vessel fistula (SAPVF) is an uncommon vascular abnormal communication. Previous studies usually adopt surgical treatments and the effectiveness of transcatheter arterial embolization for SAPVF is still unknown. Here we present a case of congenital right inferior phrenic artery to pulmonary artery fistula.
Case presentation
A 32-year-old man was admitted to the hospital with recurrent hemoptysis and then confirmed with SAPVF by computed tomography scan. After transcatheter embolization, the patient recovered well and were satisfied for treatment effect.
Conclusion
This is a rare reported case describing the clinic features and management of a youth congenital SAPVF patient.
Introduction
The systemic artery to pulmonary vessel fistula (SAPVF) is an uncommon vascular abnormal communication between systemic arteries (except bronchial arteries) and the lung parenchyma [1]. It can be divided into congenital and acquired causes. Congenital SAPVF is often accompanied by cardiac or pulmonary artery hypoplasia, and acquired are usually caused by pleural adhesions after pleurisy, empyema, trauma, or surgery [2]. Here we report a case of the congenital right inferior phrenic artery to pulmonary artery fistula which is rarely reported before.
Case Presentation
A 32-year-old man was admitted to the hospital with recurrent hemoptysis. He was previously healthy and did not have any family history of hemoptysis. He had repeated hemoptysis without obvious causes for more than a week and condition aggravation in the morning and evening, but no cough, expectoration, fever, nor dyspnea. Upon examination, there was no obvious abnormality. A preoperative nonenhanced computed tomography (CT) scan of the chest showed that a soft tissue density stripe abutting on the oblique fissure in the left lower lobe (Figure 1A). And the contrast-enhanced CT scan revealed about a 1.3 cm-sized well-enhanced vascular mass and an abnormally connection between the thickened right inferior phrenic artery and the branch of the pulmonary artery of the left lower lobe (Figure 1B). A systemic (right inferior phrenic artery)-pulmonary artery (branch of the pulmonary artery in the anteromedial basal segment of the left lower lobe) fistula was diagnosed.
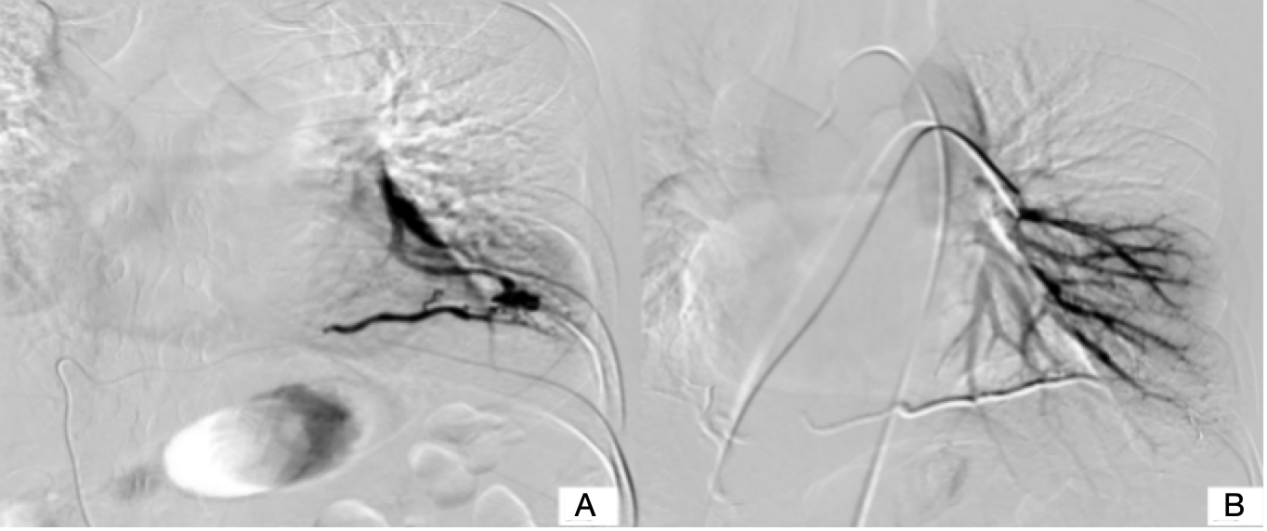
The patient refused the operation and had received embolization treatment. Two days later, we started the treatment course. Prior to embolization, vascular malformation was confirmed by selective angiography. The views have tortuous and thickened right inferior phrenic artery (Figure 1 C) and malformed anastomosis at the end of left inferior pulmonary artery display (Figure 1 D) but without obvious pulmonary vein (Figure 2 A). During the diagnostic angiography, 1.5 ml of iodized oil and 0.5 ml of tissue glue embolization were performed with a Super selective microcatheter. After embolism, there was no blood flow or a little blood flow (Figure 2 B) and soon the patient's symptom disappeared. He had simple misery in operation areas the first postoperative day, and the pain gradually ease. We consider this discomfort may related to surgical trauma. Then he was discharged from hospital after four days. No vascular abnormality was visible three and one half months later when a plain and enhanced CT were done. The patient reported minimal pain when pressure to the wound but no other symptoms.
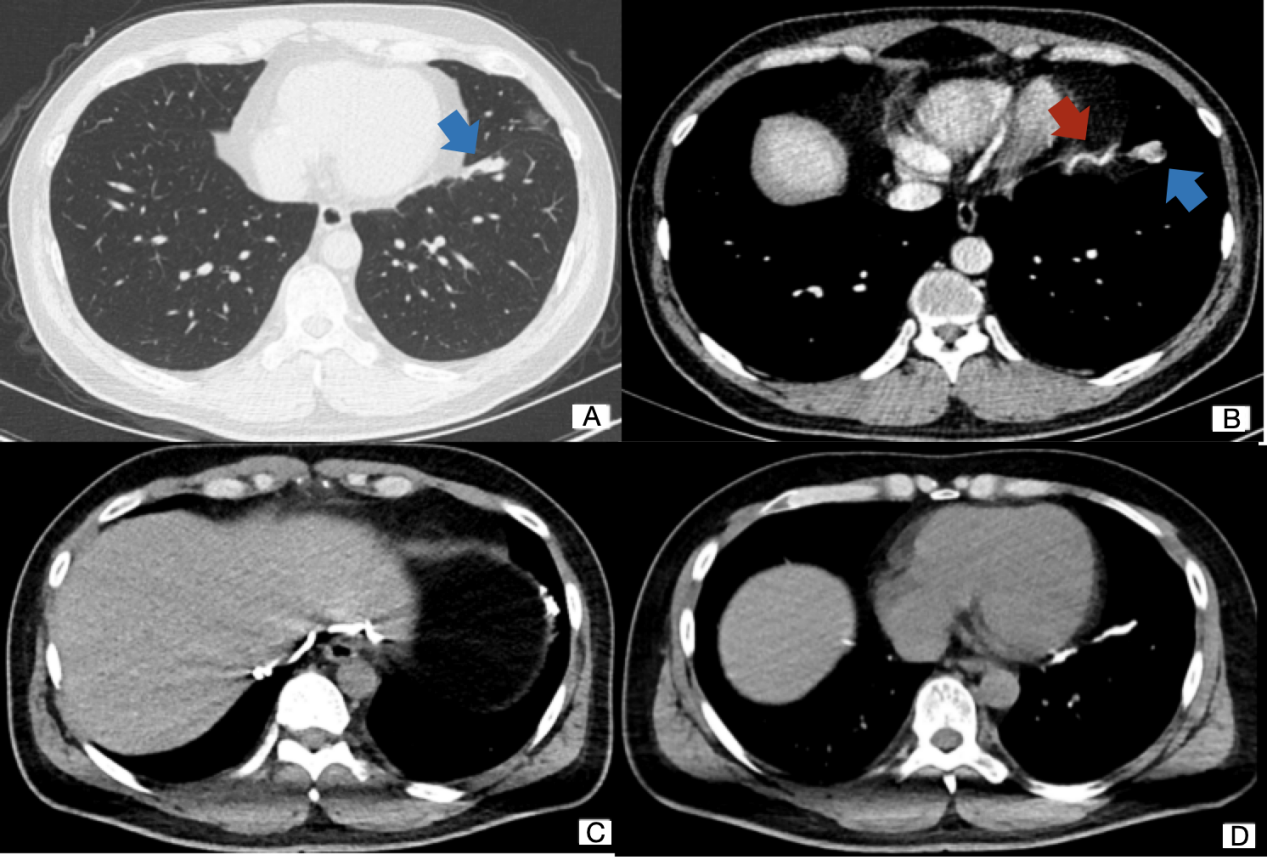
Figure 1 (A) : CT pulmonary window showed a soft tissue density strip abutting on the oblique fissure in the left lower lobe. (B) A contrast-enhanced CT scan showed a malformed vascular mass and significantly thickened right phrenic artery. (C) Selective angiography of the right inferior phrenic artery. (D) Selective angiography of the left pulmonary artery.
Discussion
SAPVF can be divided into congenital SAPVF and acquired SAPVF. About 50% of SAPVF are congenital and are more common in patients with cardiopathy or pulmonary artery hypoplasia [1]. Acquired SAPVF is mostly caused by tumors of the pleura or lung, inflammation, or iatrogenic chest injury, which obstructs the downstream obstruction of the involved vessels and creates collateral circulation in the chest wall or mediastinum.
These vascular fistulas are usually supplied by the internal thoracic and intercostal arteries, but also from the internal mammary and abnormal aortic branches, subclavian, axillary, phrenic, mediastinal, and coronary arteries [3,4]. Afferent arteries can be single or multiple and multiple systemic arteries to pulmonary artery fistulas without any other underlying diseases are extremely rare [5].
Most patients had no particular symptoms and the clinical features were continuous murmurs on chest auscultation or abnormal X-ray findings found in the patients in physical examination. Serious cases may have breathlessness, congestive heart failure, or hemoptysis [1]. When the systemic branch is the coronary artery, symptoms such as chest pain, exertional dyspnea, palpitations, angina pectoris, and acute inferior myocardial infarction may occur [6]. And if there are multiple systemic to pulmonary artery fistulas, there could be severe pulmonary hypertension [7].
Selective angiography is the reference standard for diagnosing SAPVF. It can make the complete appearance of the anatomic structure of the lesion more obvious and depict the extent and location of lung involvement. The contrast-enhanced CT also plays an important role in finding the causes of SAPVF and SAPVF related complications;therefore, it should be routinely reserved for SAPVF.
Treatment indications remain debated because the natural history of SAPVF is not well known. In patients who are unexpectedly found to have asymptomatic SAPVF, some authors believe that intervention is necessary because of the risk of bacterial infection, bleeding (dilation and rupture), and heart disease (pulmonary hypertension or congestive heart failure) [4,5].
The main treatment methods of SAPVF are including embolization, surgical treatment, or observation. Recently, embolization has become the preferred method because it causes minor trauma, minimal loss of lung parenchyma, and does not require general anesthesia [5]. It was reported that when SAPVF has few inflow arteries, surgical treatment has a better effect than embolization. However, surgical is controversial in SAPVF with multiple arterial infusions, because of the high risk for bleeding complications [1]. And comprehensive surgical treatment should be fully evaluated, particularly patients combined with other complex cardiovascular diseases [8].
Conclusions
In conclusion, we described our experience with a case of transcatheter arterial embolization for the treatment of congenital SAPVF. This treatment is a safe, less invasive, and a reasonable therapeutic option to control bleeding complications.
List of abbreviations
SAPVF: systemic artery to pulmonary vessel fistula
CT: computed tomography
Declarations
Ethics approval and consent to participate: Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Consent for publication: Consent informed consent was taken from the patient for publication of the clinical details without revealing the identity.
Availability of data and materials: The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Competing interests: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding: This study was not supported by any funding.
Authors' contributions: All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Acknowledgements: None.
References
- Riehl G, Chaffanjon P, Frey G, Sessa C, Brichon PY. (2003 )Postoperative systemic artery to pulmonary vessel fistula: analysis of three cases. Ann Thorac Surg.;76(6):1873-7. Epub 2003/12/12. doi: 10.1016/s0003-4975(03)01056-7.
View at Publisher | View at Google Scholar - Shimmyo T, Omori T, Hirano A, Masuda M. (2018 )Secondary systemic artery to pulmonary artery and pulmonary vein fistulas following the video-assisted thoracic surgery for pneumothorax: a case report. Surg Case Rep;4(1):1. Epub 2018/01/03. doi: 10.1186/s40792-017-0407-y.
View at Publisher | View at Google Scholar - Brundage BH, Gomez AC, Cheitlin MD, Gmelich JT. (1972) Systemic artery to pulmonary vessel fistulas: report of two cases and a review of the literature. Chest;62(1):19-23.
View at Publisher | View at Google Scholar - Yamada Y, Imamura H, Amamoto Y, Ochi M, Nagano K, Ito M. (1987)Congenital internal mammary artery-to-pulmonary artery fistulas: a case report. Heart Vessels;3(1):47-9.
View at Publisher | View at Google Scholar - Lee J-K, Park J-H, Kim J, Kim SJ, Lee A-R, Lee CH, et al.( 2013) Embolization of multiple systemic artery to pulmonary artery fistula with recurrent hemoptysis. Tuberc Respir Dis (Seoul);75(3):120-4. doi: 10.4046/trd.2013.75.3.120.
View at Publisher | View at Google Scholar - Said SAM, Nijhuis RLG, Akker JWOd, Takechi M, Slart RHJA, Bos JS, et al. (2014);Unilateral and multilateral congenital coronary-pulmonary fistulas in adults: clinical presentation, diagnostic modalities, and management with a brief review of the literature. Clin Cardiol;37(9):536-45. doi: 10.1002/clc.22297.
View at Publisher | View at Google Scholar - Jacheć W, Tomasik A, Kurzyna M, Pietura R, Torbicki A, Głowacki J, et al. (2019);The multiple systemic artery to pulmonary artery fistulas resulting in severe irreversible pulmonary arterial hypertension in patient with previous history of pneumothorax. BMC Pulm Med. 19(1):80. doi: 10.1186/s12890-019-0832-8.
View at Publisher | View at Google Scholar - Bito Y, Hattori K, Kato Y, Motoki M, Shibata T. Mitral (2012);valve surgery in a patient with systemic artery-to-pulmonary artery fistulas. Ann Thorac Surg. 94(4):1348-Epub 2012/09/26. doi: 10.1016/j.athoracsur.2012.02.022.
View at Publisher | View at Google Scholar

 Clinic
Clinic
