Case report | DOI: https://doi.org/10.31579/2834-796X/025
Takayasu’s Arteritis - An Unusual Cause of Stroke in a Male Young Patient
1,2 Internist, Department of Internal Medicine, Hospital Universitario del Valle, Cali, Colombia.
3 Third-year Internal Medicine Resident, Department of Internal Medicine, Universidad del Valle, Cali, Colombia.
4 Internist, Cardiologist, Department of Internal Medicine, Hospital Universitario del Valle, Cali, Colombia.
*Corresponding Author: Mónica Fernandes-Pineda, Hospital Universitario del Valle, Santiago de Cali - Colombia.
Citation: Mónica F, Pineda, Luis Fernando M, Quintero, (2023), Takayasu’s Arteritis - An Unusual Cause of Stroke in a Male Young Patient, International Journal of Cardiovascular Medicine, 2(3); DOI:10.31579/2834-796X/025
Copyright: © 2023, Mónica Fernandes-Pineda. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 22 May 2023 | Accepted: 07 June 2023 | Published: 12 June 2023
Keywords: takayasu arteritits ; young onset stroke ; large vessel vasculitis ; pulseless disease
Abstract
Takayasu arteritis (TA) is a chronic vasculitis and inflammatory disease that involves the aorta and its major branch arteries. Strokes are a common complication of Takayasu’s arteritis, but they rarely occur as the first manifestation, and there are few case reports in the literature. In this article, we describe a case of a 44-year-old female who presented with right-sided hemiparesis and non-fluent aphasia, without any significant past medical history.
Imaging studies revealed a left middle cerebral artery territory infarct with occlusion of the left common carotid artery and left subclavian artery. The patient was diagnosed with Takayasu's arteritis and was prescribed steroids, on which they partially recovered and were discharged. In conclusion, young patients who present with stroke should be investigated for Takayasu’s arteritis and started on early treatment to avoid futher complications.
Introduction
Takayasu arteritis (TA) is a chronic vasculitis and inflammatory disease that involves the aorta and its major branch arteries, resulting in a reduction in blood flow and subsequent affectation. [1]This leads to a pulseless disease with claudication, compromised peripheral pulses, and frequent ischemia.[2]
TA has an estimated annual incidence rate of 1 case per 1 million persons and tends to be more common in women, with the onset of symptoms typically occurring between the ages of 15 and 25 years. [3]
Neurological involvement can occur in half of the patients, and strokes are a common complication of Takayasu’s arteritis. However, as the first manifestation, strokes are rare, and few case reports exist in the literature. [4]
In this article, we describe the case of a patient with Takayasu arteritis who had an ischemic stroke as the first presentation.
Case Report
We report a 44-year-old male with a history of generalized myalgias and arthralgias, with headaches and cervical pain, worsening over the previous month. Who presented to a emergency department with acute onset of a dense right hemiplegia and aphasia. While driving a motorcycle the patient had her wife witnessed the neurological onset.
No other systemic symptoms predated the patient’s presentation. There was a family history of a sister with antiphospholipid syndrome. Not other cardiac, cerebrovascular or autoimmune disease.
On examination, the patient was acutely ill appearing. There were no visible signs of trauma. He had a blood pressure of 72/55 mmHg in the right upper extremity. His heart rate was 80 beats-per-minute and his respiratory rate was 21 breaths per minute with an oxygen saturation of 97% without suppot. He was non-verbal, following simple commands, and with right hemiplegia.
The patient was taken emergently for a non-contrast brain computed tomography (CT) that revealed a dense middle cerebral artery (MCA) sign on the left corresponding to a thrombus without acute hemorrhage, infarct or mass effect. The patient was administered alteplase within a 4.5 hour window without any immediate change in his clinical status.
Then a neck and brain CT angiogram was performed, which showed stenosis involving the origin of the left common carotid artery and left subclavian artery, with extensive collaterals of the vertebral arteries and basilar artery (Figure 1). No dissection of the aorta or its branches was visualized. A brain magnetic resonance image (MRI) was performed demonstrating an evolving infarct involving the area of the middle cerebral artery (MCA) (Figure 2).
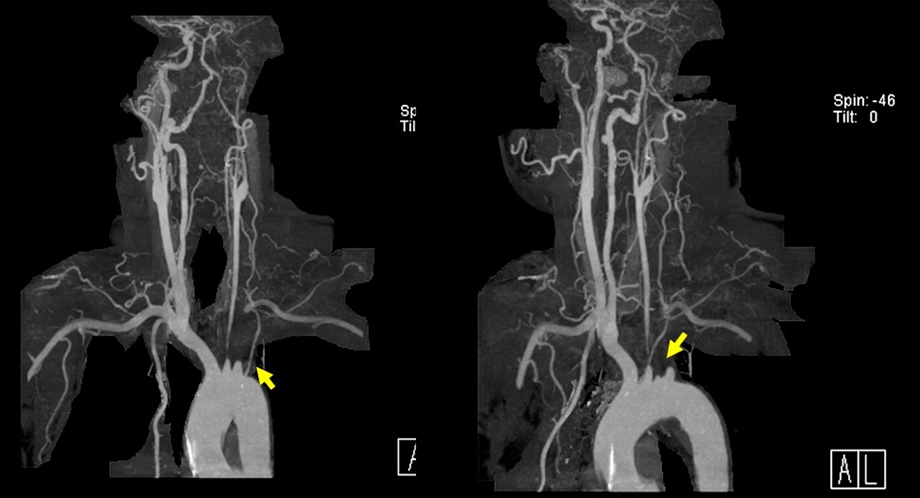
Figure 1 : Neck and brain CT angiogram. Stenosis involving the origin of the left common carotid artery and left subclavian artery, with extensive collaterals of the vertebral arteries and basilar artery
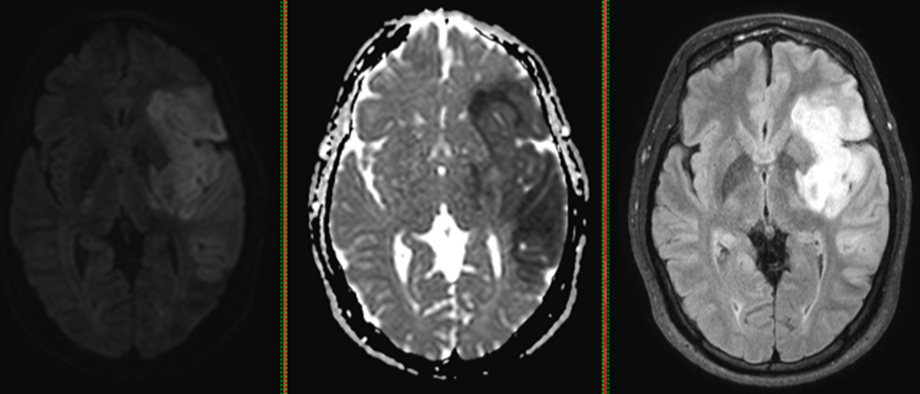
Figure 2 : Brain magnetic resonance image (MRI). Evolving infarct involving the area of the middle cerebral artery (MCA)
This pattern was highly suggestive of Takayasu's arteritis. Subsequently, a repeat vascular examination was made with reveal a wide pulse deficit, blood pressure discrepancies between two arms, without vascular bruits.
The subclavian vessel occlusion has a pathognomonic sign that is not frequently described, where the ulnar artery cannot be palpated and normal or immediate capillary refill is evident as a result of collateral circulation. This sign was present in the physical evaluation of our patient.
Laboratory testing revealed an erythrocyte sedimentation rate (ESR) of 40 mm/hour (normal 0–15 mm/hr). The patient’s complete blood count, chemistries, coagulation profiles, electrocardiogram, and chest radiograph were normal. An auto-immune screen was also negative for rheumatoid factor, anti-nuclear antibodies (ANA), extractable nuclear antigen (ENA), double-stranded DNA (dsDNA), anti-neutrophil cytoplasmic antibodies (ANCA) and antiphospholipid antibodies.
Given the clinical exam, laboratory results and the findings on the CT angiogram, the presumptive diagnosis of Takayasu’s arteritis was made. The patient was started on high dose steroids and cyclophosphamide. [5] He subsequently had normalization of his ESR and had partial clinical improvement by time of discharge.
Discussion
Takayasu's arteritis, also known as pulseless disease, was first described in 1908 by Mikito Takayasu as "a case of peculiar changes in the central retinal vessels." In this condition, the pulse is altered due to chronic inflammatory vasculitis that compromises the aorta and its major branches. [6]The pathophysiology of Takayasu's arteritis is still idiopathic. [7]
The clinical manifestations of Takayasu arteritis (TA) can vary widely, ranging from asymptomatic to severe neurological complications. There are also differences in presentation between younger and older patients (those over 40 years of age), with diagnosis often being delayed in the latter group.[1] Therefore, it is important to investigate for generalized inflammation syndrome in patients with TA who present with symptoms such as fever, night sweats, malaise, anorexia, weight loss, and diffuse myalgias, as this condition can often be misdiagnosed as an infection. [7] In the case of our patient, frequent cervical pain and headaches were the presenting symptoms.
It is important to emphasize the triphasic pattern of the disease, as patients often present during the pre-pulse inflammatory phase with non-specific systemic complaints such as fever, arthralgia, and weight loss, and are initially diagnosed with prolonged viral syndrome.(8) However, in the case of our patient, systemic symptoms were not considered until neurological complications developed.
Approximately 50% of Takayasu's arteritis patients can experience neurological symptoms, with visual symptoms being the most prevalent. The neurological presentation is so forgotten that there are Neuro-rheumatology books where it is not described. Strokes can affect 10% of the patients. The potential mechanisms that can cause stroke in Takayasu's arteritis include embolism from stenotic or occlusive lesions in the aorta and its branches, hypertension, cardioembolism, and cerebral hypoflow. [4]
Acute ischemic stroke was the initial clinical presentation in our patient. She met five of the six criteria defined by the American College of Rheumatology in 1990 and was thus diagnosed with Takayasu's arteritis. Standard treatment with high-dose steroids and cyclophosphamide as additional immunomodulators was initiated.(9) However, it is important to emphasize the need to withdraw corticosteroids as soon as possible to avoid side effects and to focus on new biological therapies, especially Tocilizumab, an IL-6 inhibitor, to improve the course of the disease. [10]
This case highlights the fact that in patients with a disease such as Takayasu arteritis, a clinical diagnosis may be possible at an early stage only with an exhaustive physical exam. [2]
TA is a variable vasculitis in both its manifestations and its coexistence with systemic inflammatory diseases, which can be evidenced in up to 19% of cases with pathologies such as inflammatory bowel disease, ankylosing spondylitis, and Behcet's disease. The association of several systemic diseases with TA is of great interest, as a wide variety of immunological mechanisms have been proposed. [1]
It is common in these coexistences to find that different types of vasculitis occur in patients with inflammatory bowel disease, including, in descending frequency, large vessel vasculitis, mainly Takayasu arteritis, and ANCA-associated vasculitis (mainly granulomatosis with polyangiitis).(12) Therefore, it is important to look for the presence of these types of diseases during the clinical course of these patients. Since these entities also lack antibodies, they could be included in the classification of autoinflammatory diseases.
Autoinflammatory diseases share phenotypic manifestations with recurrent fever attacks (not always present), lymphadenopathy, skin manifestations, vasculopathy, chest/abdominal pain, and musculoskeletal manifestations. The diagnosis is generally confirmed with pathogenic monogenic mutations, but it is mainly based on clinical findings for diagnosis.(13) We would consider that given the wide nosology of Takayasu arteritis, it should be included in the autoinflammatory syndromes, since it also lacks a demonstrated antibody.
References
- Mason JC. Takayasu arteritis—advances in diagnosis and management. Nat Rev Rheumatol. 2010 Jul;6(7):406–15.
View at Publisher | View at Google Scholar - Quinn KA, Gribbons KB, Carette S, Cuthbertson D, Khalidi NA, Koening CL, et al. Patterns of clinical presentation in Takayasu’s arteritis. Semin Arthritis Rheum. 2020 Aug;50(4):576–81.
View at Publisher | View at Google Scholar - Onen F, Akkoc N. Epidemiology of Takayasu arteritis. Presse Med. 2017 Jul;46(7–8):e197–203.
View at Publisher | View at Google Scholar - Hwang J, Kim SJ, Bang OY, Chung CS, Lee KH, Kim DK, et al. Ischemic Stroke in Takayasu’s Arteritis: Lesion Patterns and Possible Mechanisms. Journal of Clinical Neurology. 2012;8(2):109.
View at Publisher | View at Google Scholar - Saadoun D, Bura-Riviere A, Comarmond C, Lambert M, Redheuil A, Mirault T, et al. French recommendations for the management of Takayasu’s arteritis. Orphanet J Rare Dis. 2021 Jul 21;16(S3):311.
View at Publisher | View at Google Scholar - Sugiyama K, Ijiri S, Tagawa S, Shimizu K. Takayasu disease on the centenary of its discovery. Jpn J Ophthalmol. 2009 Mar 1;53(2):81–91.
View at Publisher | View at Google Scholar - Alnabwani D, Patel P, Kata P, Patel V, Okere A, Cheriyath P. The Epidemiology and Clinical Manifestations of Takayasu Arteritis: A Descriptive Study of Case Reports. Cureus. 2021 Sep 15;
View at Publisher | View at Google Scholar - Quinn KA, Gribbons KB, Carette S, Cuthbertson D, Khalidi NA, Koening CL, et al. Patterns of clinical presentation in Takayasu’s arteritis. Semin Arthritis Rheum. 2020 Aug;50(4):576–81.
View at Publisher | View at Google Scholar - Dua AB, Kalot MA, Husainat NM, Byram K, Springer JM, James KE, et al. Takayasu Arteritis: a Systematic Review and Meta‐Analysis of Test Accuracy and Benefits and Harms of Common Treatments. ACR Open Rheumatol. 2021 Feb 29;3(2):80–90.
View at Publisher | View at Google Scholar - Singh A, Danda D, Hussain S, Najmi AK, Mathew A, Goel R, et al. Efficacy and safety of tocilizumab in treatment of Takayasu arteritis: A systematic review of randomized controlled trials. Mod Rheumatol. 2021 Jan 2;31(1):197–204.
View at Publisher | View at Google Scholar - Esatoglu SN, Ok AM, Ucar D, Celik AF, Ugurlu S, Hamuryudan V, et al. Takayasu’s arteritis: associated inflammatory diseases. Clin Exp Rheumatol. 2020;38 Suppl 124(2):61–8.
View at Publisher | View at Google Scholar - Sy A, Khalidi N, Dehghan N, Barra L, Carette S, Cuthbertson D, et al. Vasculitis in patients with inflammatory bowel diseases: A study of 32 patients and systematic review of the literature. Semin Arthritis Rheum. 2016 Feb;45(4):475–82.
View at Publisher | View at Google Scholar - Betrains A, Staels F, Schrijvers R, Meyts I, Humblet-Baron S, De Langhe E, et al. Systemic autoinflammatory disease in adults. Autoimmun Rev. 2021 Apr;20(4):102774.
View at Publisher | View at Google Scholar

 Clinic
Clinic
