Review Article | DOI: https://doi.org/10.31579/2834-8761/24
Recurrent Stroke Associated to Apical Hypertrophic Cardiomyopathy In A Patient Without Atrial Fibrillation
- Elias N. Andrade-Cuellar *
- Ricardo Jesus Pérez-Castellanos
- Guadalupe Baltazar Reyes-Robledo
- Gabriela Melendez Ramírez
- Julieta Morales-Portano
1 Cardiology Service, National Medical Center November 20, Mexico City, Mexico
2 Cardiovascular Imaging Service, National Medical Center November 20, Mexico City, Mexico
*Corresponding Author: Elias N. Andrade-Cuellar, Av. Félix Cuevas #540, Col. Del Valle Del. Benito Juárez, C.P. 03100, Ciudad de México
Citation: Ricardo Jesus Pérez-Castellanos, Elias N. Andrade-Cuellar, Guadalupe Baltazar Reyes-Robledo, Gabriela Melendez Ramírez 2, Julieta Morales-Portano (2023), Recurrent Stroke Associated to Apical Hypertrophic Cardiomyopathy In A Patient Without Atrial Fibrillation, Clinical Endocrinology and Metabolism, 2(3) DOI:10.31579/2834-8761/24
Copyright: © 2023, Elias N. Andrade-Cuellar. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 13 May 2023 | Accepted: 01 May 2023 | Published: 05 June 2023
Keywords: rural alimentation; community health workers; motivation; retention; health system; all rights reserved; no reuse allowed without permission
Abstract
The Yamaguchi syndrome or apical hypertrophic myocardiopathy (AHM), it’s a subtype of non-obstructive hypertrophic myocardiopathy that affects predominantly the left ventricle apex. Its clinical presentation its very wide, inclusively may resemble an acute coronary syndrome, that’s why the diagnosis my pass out or be delayed. In this case report, we aim to share this atypical presentation of a 59 years old male who had the antecedent of 3 ischemic strokes with no etiology described. We also want to share de diversity of the tools we used to make de diagnostic and their value of their prognostic utility
Introduction
AHM was first described in Japan. Sakamoto and col. Described for the first time the typical EKG pattern in 1976 in a Japanese’s case series. But it was Yamaguchi whom first described the clinical syndrome and its ventriculographic characteristics in 19791. Diagnostic criteria have evolved over time, originally dependent of left ventriculography showing the typical shape of ‘ace of spades’ and an apex, obliteration, along with and EKG showing negative ‘giant’ T waves with a high voltage QRS complex2. Current definition needs the demonstration of a left ventricle hypertrophy predominantly at the apex, with a thickness >15 mm (below papillary muscles) and a ratio between maximal apical thickness and posterior wall >1.5 made by echocardiography or magnetic resonance imaging. American Heart Association lacks specific criteria diagnosis for AHMC but uses the same threshold of >15 mm apical thickness for the diagnosis. Apical HCM can exist with or without midventricular obstruction and cavity obliteration, and with or without apical aneurysmal formation. ApHCM can be classified into 3 forms: (1) ‘pure’, with isolated apical hypertrophy; (2) ‘mixed’, apical and septal hypertrophy with more hypertrophic apex; and (3) ‘relative’ ApHCM, which is believed to be and early phenotype of ApHCM3. Negative giant T waves defined as a negative voltage >1 mV (>10 mm) is characteristic, but no mandatory for the diagnosis, and the maximal negativity of the T wave weakly correlate with the apical thickness. 4. Next, we share the case of a 59 years old male with ischemic stroke event with ApHCM, being this his symptomatic debut of this disease.
Case Presentation
59 years old male, with antecedent of type 2 diabetes, systemic hypertension and 3 ischemic strokes. Enters to the emergency room presenting motor aphasia, with an initial NIHSS of 14 points, being on window period for thrombolysis, Neurology team then decides to administer rTPA, improving neurological symptoms to a NIHSS of 9 points at the next hour. As a part of the etiology diagnosis protocol Neurology requested our intervention. Initially we took an EKG which showed sinus rhythm but with classical giant negative T waves in precordial derivations (Figure 1), that’s why we proceed to make an transthoracic echocardiogram, showing an no dilated left ventricle with hypertrophy at medial and apical segments, normal mobility and thickness, preserved systolic function (LVEF 53%), and diminished global longitudinal strain (GLS) of -12% and a incremented global circumferential strain of -35%, evidence of ventricle diastolic function grade I, LA Volume index if 25 ml/m2 and without valvulopathy (Figure 2). Suspecting atrial fibrillation as the main cause, a Holter was requested, nevertheless, the report showed sinus rhythm throughout the record. At this moment, ApHCM was highly suspected, that’s why a Cardiac Magnetic Resonance was requested (Figure 3), corroborating the diagnosis with a anterior apical thickness of 17 mm, also, highlighting the presence of moderate fibrosis.
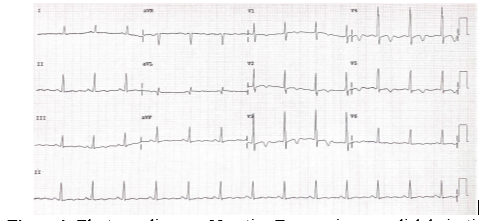
Figure 1: Electrocardiogram. Negative T waves in precordial derivations.
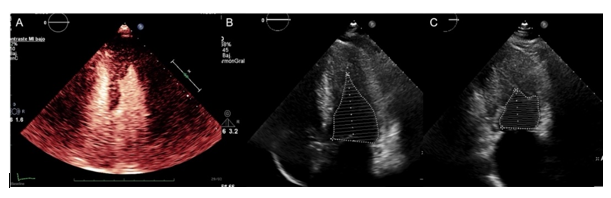
Figure 2: Transthoracic echocardiogram. A: ETT with contrast showing apical hypertrophy. B y C: Apical Apical 4 chambers showing apical obliteration at end-diastolic and preserved ejection fraction.
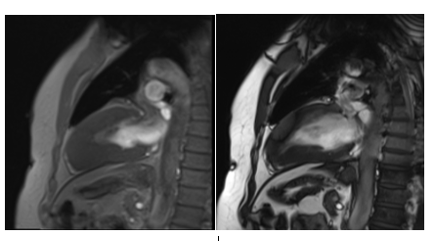
Figure 3: Cardiac Magnetic Resomange Imaging. Wall thickness of the apical segment: 17 mm, apical septim 16 mm, inferior apical segment 16 mm, lateral apical segment 13 mm. Intramyocardial gadolinium late enhancement (GLE) in anteroseptal basal segment, and diffuse intramyocardial GLE at the apex and inferior segment.
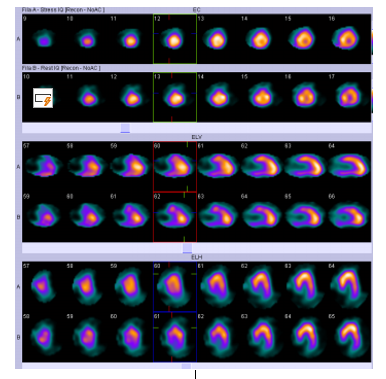
Figure 4. Nuclear imaging. No perfusion defects

Discussion
In the contemporary clinical practice, echocardiography is the standard tool for the diagnosis and integral evaluation of ApHCM. Transthoracic echocardiography can reveale apical hypertrophy, differentiate between ‘pure’ and ‘mixed’ forms, and identify adittional prognostic characteristics that my influence the long term results, like the presence of diastolic function, cavity obliteration or aneurysmal formation. Contrast echocardiography helps to confirm or exclude the diagnosis by this method, when non-contrast imaging are suboptimal [1]. Cardiac Magnetic Resonance Imaging (CMRI) can detect early ApHCM phenotypes better than echocardiography. CMRI is more sensitive to detect apical aneurysm and it can identify between the 25% and 43% aneurysm that are not evident with TTE [5]. Late Gadolinium Enhancement (LGE) its common in HMC, the presence and quantity of LGE may be associated to the severity of the hypertrophy, as well as a higher risk for development of heart failure [6]. An study of 1293 patients, showed that an LGE >15% of LV mass has a 2-fold risk increase of Sudden Cardiac Death (SCD) in those patients first considered with low risk, with an estimated probability of 6% SCD events at 5 years. In this cohort, an increase of 10% in LGE was associated with and increase of the 40% relative risk of SCD events. LGE pattern in ApHCM are characteristically apical and subendocardial. Perfusion abnormalities at rest have been well described in classic HCM and corelates with LGE severity, hypertrophy grade and myocardial fibrosis [7]. An LGE >14.4% its considered an independent predictor of thromboembolic event in patients with HCM (Sensitivity 65%, specificity 78%, P <0>[8] In a review of 33 studies, prevalence of atrial fibrillation (AF) in HCM was 22%, and the incidence of thromboembolic events in patients with HCM and AF was 3.8% per patient per year. In fact, the European Society of Cardiology affirms that all patients with AF (paroxysmal, persistent and permanent) with HCM should be offer anticoagulation regardless their CHA 2 DS 2 ‐VASc score8. In this case, we couldn’t be able to identify AF episodes that explained the stroke events, nevertheless, with CMRI we identified moderate fibrosis at apical and basal segments, that could explain the embolic source. There is lack of evidence to justify anticoagulation in patients with ApHCM with moderate fibrosis and recurrent ischemic strokes.
Conclusions
Hypertrophic myocardiopathy its a disease with important prevalence and incidence, which entails great mortality for its great risk of sudden death and thromboembolic events. As related to thromboembolism, the prevalence its 1 to 4 patients per 100 in a year, atrial fibrillation is recognized as the main cause of this events. Our main interest to share this case, is the lack of diagnosis of paroxysmal atrial fibrillation in this patient, what may directly indicate the need of anticoagulation. Nonetheless, recurrence of ischemic stroke events in the absence of atrial fibrillation, suggest the probability of silent episodes or that purely ApMCH be the cause of this embolic events due to blood stasis generated by the akinetic apex.
Funding and outreach support:
Does not apply
Interest conflict:
The authors declare no conflict of interest.
References
- Hughes, R. K. et al. (2020). Apical Hypertrophic Cardiomyopathy: The Variant Less Known. J Am Heart Assoc 9,
View at Publisher | View at Google Scholar - Yamaguchi, H. et al. (1979) Hypertrophic nonobstructive cardiomyopathy with giant negative T waves (apical hypertrophy): ventriculographic and echocardiographic features in 30 patients. Am J Cardiol 44, 401–412.
View at Publisher | View at Google Scholar - Chen, C. C., Lei, M. H., Hsu, Y. C., Chung, S. L. et al, (2011). Apical hypertrophic cardiomyopathy: correlations between echocardiographic parameters, angiographic left ventricular morphology, and clinical outcomes. Clin Cardiol 34, 233–238
View at Publisher | View at Google Scholar - Maron, M. S. et al. (2008). Prevalence, clinical significance, and natural history of left ventricular apical aneurysms in hypertrophic cardiomyopathy. Circulation 118, 1541–1549
View at Publisher | View at Google Scholar - Eriksson, M. J. et al. (2002). Long-term outcome in patients with apical hypertrophic cardiomyopathy. J Am Coll Cardiol 39, 638–645
View at Publisher | View at Google Scholar - Hohneck, A. et al. (2020). Extent of Late Gadolinium Enhancement Predicts Thromboembolic Events in Patients With Hypertrophic Cardiomyopathy. Circ J 84, 754–762
View at Publisher | View at Google Scholar - Guttmann, O. P., Rahman, M. S., O’Mahony, C., Anastasakis, A. & Elliott, P. M. Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: systematic review. Heart 100, 465–472
View at Publisher | View at Google Scholar - Zamorano, J. L. et al. (2014) ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 35, 2733–2779
View at Publisher | View at Google Scholar

 Clinic
Clinic
