Research Article | DOI: https://doi.org/10.31579/2835-785X/094
Pattern of Bedsore in Hospitalized Patients
- Md Shafiullah Prodhania *
Associate Professor, International Institute of Health Sciences, Sylhet, Bangladesh.
*Corresponding Author: Md Shafiullah Prodhania, Associate Professor, International Institute of Health Sciences, Sylhet, Bangladesh.
Citation: Md Shafiullah Prodhania, (2025), Pattern of Bedsore in Hospitalized Patients, International Journal of Clinical Research and Reports. 4(5); DOI:10.31579/2835-785X/094
Copyright: © 2025, Md Shafiullah Prodhania. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 08 August 2025 | Accepted: 22 August 2025 | Published: 01 September 2025
Keywords: pneumatic bed; risk factors; spinal cord injury; stroke
Abstract
This descriptive type of cross-sectional study was conducted to assess pattern and risk factors of bedsore in hospital admitted patients in Dhaka city with a sample size of 114. A pretested, modified, questionnaire was used to collect the data. All the data were entered and analyzed by using Statistical Package of Social Science 16.0 versions.Study found that 17.5%, 41.2%, 27.2% and 14% of the respondents belonged to age group of 1-20 years, 21-40 years, 41-60 years and 61-80 years respectively with mean age 37.97 +16.909 years. Responsible diseases for bedsore were spinal cord injury (41.2%), fracture (30%), stroke (24%), unconsciousness (7.2%) and GBS (2.8%) respectively. Study revealed that common area of bedsore was back of the sacrum (57%), back of the scapula (34.2%), medial aspect of knee joint (22.8%), malleoli (21.1%), greater trochanter of femur (15.8%), external occipital protuberance (14%), olecranon process of ulna (9.6%), above the coccyx (9.6%), iliac crest (7%), spine of the scapula (3.5%), posterior superior iliac joint (2.6%) and sacro-iliac joint (1.8%) respectively. Study also found that superficial and deep type of bedsore were 58.8% and 41.2% consecutively. Besides study revealed that 26.3% of the respondents were diabetic, 31.6% obese, 28.1% suffering from malnutrition, 61.4% did not use pneumatic bed and 7.2% patients did not maintain proper positioning 2 hourly and these were the risk factors of this study. Significant association was found between type of bed sore and use of pneumatic bed (p<0.05) as well as nutritional status (p<0.05). Changing position and use of pneumatic bed was best methods of prevention of bedsore.
Background
Bedsores are a significant health burden, but little is known of the impact on the quality of life of the sufferer. They mainly affect older people; Pressure ulcers produce endless pain; pressure ulcers produce a restricted life; coping with a pressure ulcer. Several patients also reported that pain was exacerbated by their pressure relieving equipment and at dressing change. Patients found that the pressure ulcer restricted their activities and had an impact on their families. In addition, for some, the restrictions delayed their rehabilitation [1]. Pressure ulcers are a common and painful health condition, particularly among people who are elderly or physically impaired. Despite our knowledge of how to prevent pressure ulcers, and improvements in treatment, pressure ulcers remain prevalent and impose a significant burden on financial and labor resources in the healthcare industry. Under nutrition is a risk factor, and nutrition therapy plays a crucial role in pressure ulcer treatment. Micronutrients should be replaced if depleted, but routine supplementation of vitamins and minerals in all pressure ulcer patients is not warranted [2]. Cumulative incidence of Pressure ulcer more in acute hospital admitted patients than bedside in home sitting. The relative rates in rehabilitation and nursing home settings were 1.4 and 1.3, respectively [3]. Patients aged ≥65 years who had surgery for hip fracture were examined by research nurses at baseline and on alternating days for 21 days [4]. Study was found that the mean age of the study was 44.51. Regarding to sex it was found that the highest percentages of the study samples were male 60.4%. It presented that nurses performance were used bed sheets and observe signs and symptoms of sores sites for most of patients as pressure ulcer prevention constituted 100% and 62.5% [5]. Although no gold standard for preventing or treating pressure ulcers has been established, data from clinical trials indicate specific efforts are worthwhile. Preventive strategies include recognizing risk, decreasing the effects of pressure, assessing nutritional status, avoiding excessive bed rest, and preserving the integrity of the skin. Treatment principles include assessing the severity of the wound; reducing pressure, friction, and shear forces; optimizing wound care; removing necrotic debris; managing bacterial contamination; and correcting nutritional deficits [6]. Intervention strategies included PU-specific changes in combination with educational strategies. Most studies reported patient outcome measures, while fewer reported nursing process of care measures. For nearly all the studies, the authors concluded that the intervention had a positive effect [7]. With reported incidence rates of bedsore development in the adult critical care population as high as 56%; the identification of patients at high risk of bedsore development is essential. This paper will explore the association between bedsore development and risk factors [8]. A review was conducted to clarify the role of pressure ulcer risk assessment in clinical practice [9]. This generally well-conducted review concluded that commonly used instruments can predict which patients are more likely to develop a pressure ulcer. There were no clear differences in test accuracy between methods. Advanced static support surfaces were more effective than standard mattresses for reducing risk of pressure ulcers. The review conclusions seem appropriate [10]. Most of the pressure ulcers were stage 2, and the majority was in the sacral area or on the heels. In multivariable analysis, pressure ulcer incidence was significantly associated with increasing age, male gender, dry skin, urinary and fecal incontinence, difficulty turning in bed, nursing home residence prior to admission, recent hospitalization, and poor nutritional status [11]. To identify resident, wound, and treatment characteristics associated with pressure ulcer healing in long-term care residents. In this sample of nursing facility residents, use of moist dressings and adequate nutritional support are strong predictors of pressure ulcer healing [12]. The overall prevalence of pressure ulcers was 27%. Multivariate analysis showed a statistically significant positive association between high-risk condition of pressure ulcer and previous stroke, previous trauma, cardiovascular diseases. The risk of pressure ulcers according to number of full-time nurses and auxiliary staff per 10 beds lower than five was marginally statistically significant [13]. There is no decrease in pressure ulcer incidence was found which might be attributed to use of an assessment scale. However, the use of scales increases the intensity and effectiveness of prevention interventions. The Braden Scale shows optimal validation and the best sensitivity/specificity balance [14]. Absence of pressure ulcers is increasingly being used as an indicator of quality nursing care, based on the premise that pressure ulcers are preventable [15].
Materials and Methods
Descriptive type cross-sectional study was conducted to determine the pattern and risk factors of bedsore with 114 samples. The study site was Dhaka Medical College Hospital Shah Bag, National Institute of Traumatology and Orthopedic Rehabilitation situated in Shamolly and Metropolitan Medical Centre, Mohakhali, of Dhaka city. The study period was conducted for six months started from June 2013 to December 2013. Non randomized purposive sampling method was applied for data collection. A pre tested modified semi-structured questionnaire which were prepared on the basis of objectives and different variables of this study. The collected data was edited by checking rechecking analyzed by using the software SPSS 16.0 version. Then analyzed data were presented according to the variables of the study.
Results
Analysis of socio-demographic variables and (table no.1) showed that 17.5%, 41.2%, 27.2% and 14% of the respondents belonged to age group of 1-20years, 21-40 years, 41-60 years and 61-80 years respectively with mean age 37.97 +16.909 years.
Table 1: Distribution of the respondents by age (n=114)
| Age | Frequency | Percent |
| 1-20 | 20 | 17.5 |
| 21-40 | 47 | 41.2 |
| 41-60 | 31 | 27.2 |
| 61-80 | 16 | 14.0 |
| Total | 114 | 100.0 |
(Table no. 2) showed that most of the respondents 77.2% are Male and rest of them 22.8% are Female of them of the respondents are primary 39.5%, followed by Secondary 20.2%, Higher Secondary 12.3%, Graduate 18.4% and Post Graduate and above 9.6% respectively. Among the respondents Married 72.8%, unmarried 21.9%, Widow/ Widowed 3.5% and only are Divorced/ Separate 1.8% respectively. It is reveals that occupation of the respondents is student 21.9%, service holder 22.8%, employer 15.8%, worker 31.6% and rest of them are retread person 7.9% respectively.
Table 2: Distribution of the respondents by sex (n=114)
| Sex | Frequency | Percent |
| Male | 88 | 77.2 |
| Female | 26 | 22.8 |
| Total | 114 | 100.0 |
(Table no. 3) revealed that common area of bedsore of the respondents were followed by back of the sacrum 57%, back of the scapula 34.2%, medial aspect of knee joint 22.8%, malleoli 21.1%, greater trochanter of femur 15.8%, external occipital protuberance 14%, above the coccyx and olecranon process of ulna 9.6%, iliac crest 7%, spine of the scapula 3.5%, posterior superior iliac joint 2.6%, sacro-iliac joint 1.8%, and respectively.
Table 3: Distribution of the respondents by common area of bedsore (Multiple Responses)
| Variables | Frequency | Percent |
| External occipital protuberance | 16 | 14.0 |
| Spine of the scapula | 4 | 3.5 |
| Back of the scapula | 39 | 34.2 |
| Olecranon process of ulna | 11 | 9.6 |
| Iliac crest | 8 | 7.0 |
| Posterior superior iliac joint | 3 | 2.6 |
| Sacro-iliac joint | 2 | 1.8 |
| Back of the sacrum | 65 | 57.0 |
| Above the coccyx | 11 | 9.6 |
| Greater trochanter of femur | 18 | 15.8 |
| Medial aspect of knee joint | 26 | 22.8 |
| Malleoli | 24 | 21.1 |
(Figure no. 1) found that superficial and deep type of bedsore were 58.8% and 41.2% respectively.
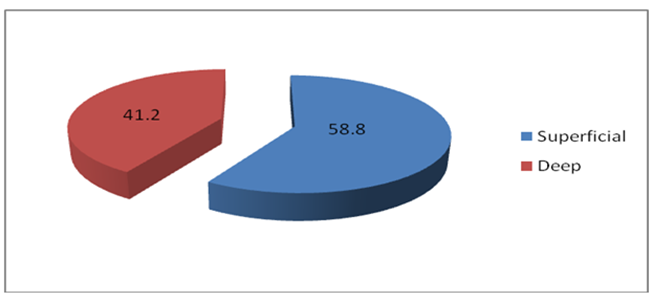
Figure 1: Distribution of the respondents by type of bed sore (n=114)
(Table no. 4) revealed that several risk factors influenced the develop and severity of bedsore that were 61.4% did not use pneumatic bed (air mattress), 31.6% obese, 28.1% malnourished, 26.3% the respondents were diabetic and 7.2% patient did not maintain proper positioning 2 hourly.
Table 4: Distribution of the respondents by risk factors (n=114)
| Risk factors | Frequency | Percent |
| Diabetic | 30 | 26.3 |
| Obese | 36 | 31.6 |
| Malnutrition | 32 | 28.1 |
| Do not use pneumatic bed | 70 | 61.4 |
| Lack of positioning 2 hourly | 9 | 7.2 |
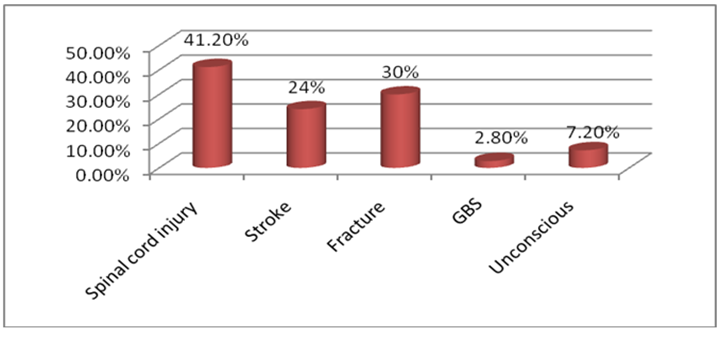
(Figure no. 2) reveled that responsible disease for bedsore were spinal cord injury 41.2%, fracture 30%, stroke 24%, unconsciousness 7.2%, GBS 2.8%.
Figure 2: Distribution of the respondents by responsible disease for bedsore (Multiple Responses)
(Table no. 5) revealed that a highly significant association was found between types of bedsore and use pneumatic bed (p<0>
Table 5: Distribution of respondents by association between type of bedsore and use pneumatic bed (n=114)
Types of bed sore | Use Pneumatic bed | Total | p-value | |
| Yes | No | |||
| Superficial | 12 | 55 | 67 |
0.000 |
| Deep | 32 | 15 | 47 | |
| Total | 44 | 70 | 114 | |
(Table no. 6) revealed that a significant association was found between type of bedsore and nutritional status of patients (p<0>
Table 6: Distribution of respondents by association between type of bedsore and nutritional status of patients (n=114)
| Type of bed sore | Nutritional status of patients | Total | p-Value | |
| Yes | No | |||
| Superficial | 55 | 12 | 67 |
0.004 |
| Deep | 27 | 20 | 47 | |
| Total | 82 | 32 | 114 | |
Discussion
Study revealed that common area of bedsore were back of the sacrum 57%, back of the scapula 34.2%, medial aspect of knee joint 22.8%, malleoli 21.1%, greater trochanter of femur 15.8% this findings was similar to the study carried out by the Mona Baumgarten, David Margolis, et al editors.4 Responsible diseases for bedsore were spinal cord injury 41.2%, fracture 30%, stroke 24%, unconscious 7.2% and GBS 2.8% respectively which was also similar to the study of A Capon, N Pavoni, et al editors.13 The present study found that 58.8% superficial type of bedsore and 41.2% was deep. Study revealed that 26.3% of the respondents were diabetic, 31.6% obese, 28.1% suffered from malnutrition, 61.4% did not use pneumatic bed and 7.2% patients did not maintain proper positioning 2 hourly this finding was supported by the study of Sewchuk D, Padula C, Osborne E. [15]. There were statistically significant association between type of bad sore with nutritional status of patient and use pneumatic bed and this finding was similar to the study carried out by the M Baumgarten, DJ Margolis, Localio, et al editors [11].
Conclusion
The present study found pattern and risk factor bedsore, such as obesity, diabetic, malnutrition, did not use pneumatic bed and not maintain proper positioning, bony prominent area of the body in different position especially supine. Above all we concluded that minimizing risk factors and proper physiotherapy care may reduce incidence of bedsore in hospital admitted patients.
References
- Hopkins A, Dealey C, Bale S, Defloor T, Worboys F. Patient stories of living with a pressure ulcer. J Adv Nurs. 2006 Nov;56(4):345‐53.
View at Publisher | View at Google Scholar - Jennifer Doley, Jennifer Doley. Nutrition Management of Pressure Ulcers. Nutr Clin Pract February 2010:25(1 50-60).
View at Publisher | View at Google Scholar - Mona Baumgarten, David J. Margolis, Denise L. Orwig, Michelle D. Shardell,et al editors. Pressure ulcers in elderly hip fracture patients across the continuum of care. J Am Geriatr Soc. 2009 May; 57(5): 863–70.
View at Publisher | View at Google Scholar - Mona Baumgarten, David Margolis, Denise Orwig, William Hawkes, et al editors. Use of pressure-redistributing support surfaces among elderly hip fracture patients across the continuum of care: adherence to pressure ulcer prevention guidelines. Gerontologist. 2010 April; 50(2): 253-62.
View at Publisher | View at Google Scholar - Inshrah Roshdy Mohamed and Esraa Esam-Eldin Mohamed. Nursing Practices for patients at risk to the pressure sores in Minia University Hospital. Journal of American Science 2013;9(4).
View at Publisher | View at Google Scholar - Thomas DR. Prevention and treatment of pressure ulcers: what works? what doesn't? Cleve Clin J Med. 2001 Aug;68(8):704-7, 710-14, 717-22
View at Publisher | View at Google Scholar - Soban LM, Hempel S, Munjas BA, Miles J and Rubenstein LV. Preventing pressure ulcers in hospitals: A systematic review of nurse-focused quality improvement interventions. Jt Comm J Qual Patient Saf. 2011 Jun;37(6):245-52.
View at Publisher | View at Google Scholar - Nahla Tayyib, Fiona Coye and Peter Lewis. Pressure ulcers in the adult intensive care unit: a literature review of patient risk factors and risk assessment scales. Journal of Nursing Education and Practice, 2013; 3(11).
View at Publisher | View at Google Scholar - Moore ZE and Cowman S. Risk assessment tools for the prevention of pressure ulcers. Cochrane Database Syst Rev. 2008 Jul 16;(3):CD006471.
View at Publisher | View at Google Scholar - Chou R, Dana T and Bougatsos C. et al editors. Pressure ulcer risk assessment and prevention: comparative effectiveness. An International Journal;18(4).
View at Publisher | View at Google Scholar - Baumgarten M, Margolis DJ, Localio AR, Kagan SH, et al editors. Pressure ulcers among elderly patients early in the hospital stay. J Gerontol A Biol Sci Med Sci. 2006 Jul;61(7):749‐54.
View at Publisher | View at Google Scholar - Bergstrom N, Horn SD, Smout RJ, Bender SA et al editors. The National Pressure Ulcer Long‐Term Care Study: outcomes of pressure ulcer treatments in long‐term care. J Am Geriatr Soc. 2005 Oct;53(10):1721‐9.
View at Publisher | View at Google Scholar - Capon A, Pavoni N, Mastromattei A, Di Lallo D. Pressure ulcer risk in long‐term units: prevalence and associated factors. J Adv Nurs. 2007 May;58(3):263‐72.
View at Publisher | View at Google Scholar - Pancorbo‐Hidalgo PL, Garcia‐Fernandez FP, Lopez‐Medina IM, Alvarez‐Nieto C. Risk assessment scales for pressure ulcer prevention: a systematic review. J Adv Nurs. 2006 Apr;54(1):94‐110.
View at Publisher | View at Google Scholar - Sewchuk D, Padula C, Osborne E. Prevention and early detection of pressure ulcers in patients undergoing cardiac surgery. AORN J. 2006 Jul;84(1):75‐96.
View at Publisher | View at Google Scholar

 Clinic
Clinic
