Research Article | DOI: https://doi.org/10.31579/2835-8465/005
Outcome Analysis of Hemiarthroplasty versus Total Hip Arthroplasty for Unstable Intertrochanteric Fractures in Elderly Osteoporotic Patients
1 Fellowship student, Grant Medical College & J.J. Hospital, Mumbai, India.
2 Honarary Professor & Unit Head, Grant Medical College & J.J. Hospital, Mumbai, India.
3 Associate Professor, Grant Medical College & J.J. Hospital, Mumbai, India.
*Corresponding Author: Sameer Salgar, Fellowship student, Grant Medical College & J.J. Hospital, Mumbai, India.
Citation: Sameer Salgar, Sangeet Gawhale and Nadir Shah, (2023), Outcome Analysis of Hemiarthroplasty versus Total Hip Arthroplasty for Unstable Intertrochanteric Fractures in Elderly Osteoporotic Patients, Orthopaedics Case Reports, 2(2); DOI:10.31579/2835-8465/005
Copyright: © 2023, Sameer Salgar. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 09 March 2023 | Accepted: 23 March 2023 | Published: 14 April 2023
Keywords: hip arthroplasty; hemiarthroplasty; unstable intertrochanteric fractures; osteoporotic patients; AO
Abstract
Hip fractures are common in elderly patients and place significant burden on healthcare system across the world. The demographics of world populations are set to change, with more elderly living in developing countries, and it has been estimated that by 2050 half of hip fractures will occur in Asia. The incidence of proximal femoral fractures has increased due to the higher life expectancy of population. As most patients with intertrochanteric fractures are elderly, operative treatment must be rapid and permit immediate weight bearing postoperatively. The communition, osteoporosis and instability often delay early weight bearing after internal fixation and also affects the prognosis. Also, there is higher incidence of general complication due to prolonged recovery time after internal fixation.
Introduction
Hip fractures are common in elderly patients and place significant burden on healthcare system across the world. The demographics of world populations are set to change, with more elderly living in developing countries, and it has been estimated that by 2050 half of hip fractures will occur in Asia [1]. The incidence of proximal femoral fractures has increased due to the higher life expectancy of population [2]. As most patients with intertrochanteric fractures are elderly, operative treatment must be rapid and permit immediate weight bearing postoperatively. The communition, osteoporosis and instability often delay early weight bearing after internal fixation and also affects the prognosis [3,4,5]. Also, there is higher incidence of general complication due to prolonged recovery time after internal fixation [6,7]. After hemi or total arthroplasty, patients are able to bear weight immediately and encouraged to walk early and exercise the involved limb thus reducing the period of bed rest and complication [8,9]. Currently there are very few published article comparing result of bipolar hemiarthroplasty and total hip replacement. The aim of our study by compare effects and outcomes of bipolar hemiarthroplasty and Total hip replacement in unstable intertrochanteric fractures.
Materials and Methods
All patients were with unstable intertrochanteric fractures were admitted to this hospital between 2016 and 2020. The study is retrospective study. The Singh Index was used as measure of osteoporosis based on anteroposterior AP radiograph of contralateral hip. Total 35 patients with A2.2 and A2.3 Intertrochanteric fracture with age greater than 70 years according to A.O. Classification were treated with either Hemiarthroplasty or Total hip replacement. The follow-up period at 6wks, 3 months, 6 months, 12 months, and yearly thereafter. It ranged from 3 to 5yrs.
2.1 Inclusion criteria:
- Unstable intertrochanteric fractures AO 31A2.2 & 31A2.3
- Age more than 70 yrs.
- Severe osteoporosis sign index less than 3
- Independently mobile with or without aid.
THR is done in mentally healthy & independently mobile patients while BA was chosen in patients with mobility limited to house or short distance outside home.
2.2 Exclusion criteria:
- Senile Dementia
- Osteoarthritis OR Rheumatoid arthritis in fractured hip
2.3 Surgical technique:
All patients underwent surgery with transtrochanteric approach. In lateral position with either spinal-epidural anesthesia or general anaesthesia. Lateral skin incision centered over greater trochanter is taken. Subcutaneous tissue and TFL incised in line with skin incision. Head extracted with corkscrew and size of head is measured with gauge. Length between centre of head to lower end of neck measured. Femoral canal was prepared with canal finder and rasp. Cement restrictor placed at appropriate distance and cement introduced in canal in doughy state. Stem is inserted with height of prosthesis kept equal to distance measured from center of head to lower end of neck. The version was determined keeping prosthesis 15 degree anteverted with respect to transcondylar axis which is perpendicular to vertical tibia. Hip reduced & check for range of motion and stability. Isolated fragment of lesser trochanter were not reduced and fixed.
For THR group, the acetabulum was prepared & cemented or uncemented cup was used with UHMWPE liner inside. The Optimal socket position was 40 +/- 10 degree of abduction and 15+/- 10 degree of anteversion (Lewinnek safe zone). The Greater trochanter fragments were wired with SS wire. Routine closure was performed over vacuum drain. Post operatively, all patients underwent physiotherapy. Check dress was performed after 48hrs with removal of vacuum drain. Pillow was kept between legs to prevent excess adduction for 2 weeks. Patients are mobilized on 3rd to 5th post operative day. The Functional outcome is evaluated using Harris Hip Score (HHS). X-ray of the hip is taken at regular interval.
2.4 Postoperative protocol
In post operative period, operated limb was kept in abducted position with abduction pillow between the legs. All patients were mobilised on the next postoperative day with walker. Check dressing was done after 48 hours.
Results
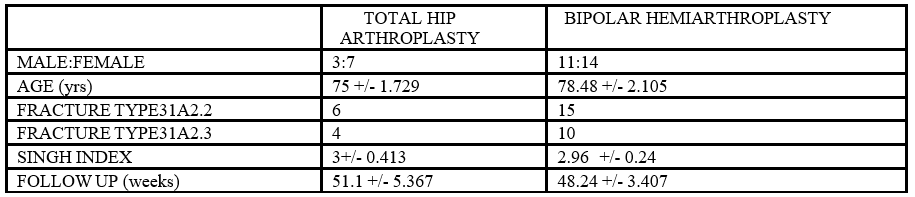
All patients with unstable intertrochanteric fractures were admitted between 2015 & 2019.Out of total 35 patients,10 patients underwent Total Hip Arthroplsty (figure 2.1 & 2.2) & 25 patients were operated for Bipolar hemiarthroplasty (fig.1.1 & 1.2). The mean follow up period for BA was 48.25 months (36-60 months) while for THA group, it was 50.5 months (37-60 months) with statistically insignificant difference. As per demographic information (Table 1.1) the THA group includes 3 males & 7 females with mean age being 75yrs while BA group consisted of 11 males & 14 females with mean age of 78.48 yrs. There were 6 & 4 cases of 31A2.2 & 31A2.3 fracture pattern respectively in THR group & 15 & 10 cases of 31A2.2 & 31A2.3 in BA group. The other parameters such as Singh index and Follow up period were statistically insignificant.
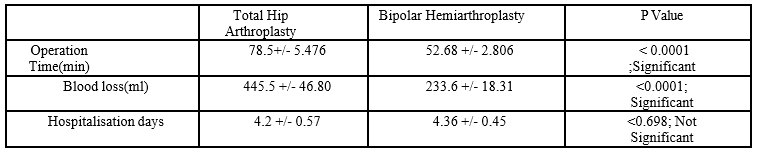
In operative records (Table 1.2), mean operation time is 78.5 min & 52.68 min for THR and BA respectively. The average blood loss of the THA group is 445.5 ml & for BA group is 233.6 ml. The mean hospitalization days for THA group is 4.2 days & for BA is 4.36 days. The statistically significant difference was found in blood loss and operation time, while hospitalization days were statistically insignificant.
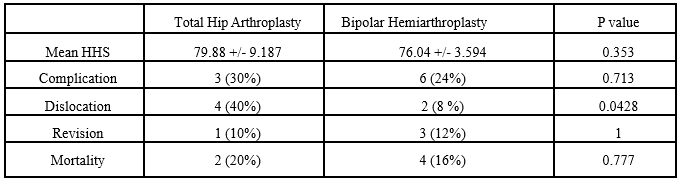
The outcome analysis (Table 1.3) showed that mean HHS was 79.88 in THR group & 76.04 in BA group with statistically insignificant difference. No statistically significant difference was found in complication, revision surgery and mortality. Dislocation rate was statistically significant in THA group compared to BA group. Two dislocations occurred in THA group which were close reduced while four dislocations occurred in BA group, which were also close reduced. One patient in THA group and 3 patients in BA group required revision. Moreover, mortality rate was statistically insignificant. Radiograph at the last follow up showed trochanter nonunion in four cases in BA. In BA, three patients required revision for periprosthetic fracture, imlplant loosening and infection. In THR group one patient developed heterotrophic ossification (figure 2.2).




Discussion
Multiple operative treatment option are available for unstable intertrochanteric fracture. Tronzo first reported the use of long straight stem prosthesis for intertrochanteric fractures in 1974 [10]. Stern & Goldstein in 1979 reported 43 cases of communities intertrochanteric fractures by long stem Leinbach prosthesis [11]. Review of literature shows that many publications suggested the use of hip replacement to treat communited intertrochanteric fractures in elderly patients in view of dramatic pain relief, immediate weight bearingand easier postoperative rehabilitation [12-19]. Sidhu et al., also proved in their study on 53 patients that THA may be valid treatment option in mentally healthy elderly patients [20]. Haentjens et al. [14,15], reviewed the literature and summarized reports regarding prosthetic replacement for treatment of intertrochanteric fractures and their complication. They concluded that patient with severe osteoporosis may benefit from prosthetic replacement for communitied intertrochanteric fractures and nonunion.
Complication associated with hip replacement such as dislocation is associated with bed sores, deep vein thrombosis and pneumonia. Dislocation is seen in 4 out of 10 cases in THA group while 2 out of 25 cases were observed in BA group. All cases were close reduced and given abduction brace. In BA group, complication such as protrusion, stem fracture, implant loosening & trochanter nonunion were seen. Unreduced fracture of lesser trochanter were not problematic for patients.
Protrusion occurs due to acetabular wear. Case of protrusion was revised to THA. Also complications such as implant loosening & stem fracture were revised to THA.
It is also found that 27 percentage cases expired before 5yrs. Using internal fixation devices, high rates of local and general complication is related to restricted weight bearing causing prolonged bed rest and consequently higher mortality rate.
Hip replacement may offer potential for quick recovery with little risk of mechanical failure, avoids the risk associated with internal fixation and enables patients to maintain good level of function after surgery. It Is not associated with complication such as malunion, nonunion or a avascular necrosis of femoral head.
To compare surgical outcome between BA and THA for unstable intertrochanteric fractures three intraoperative & four post op factors in were considered. The BA vis-a-vis THA has the advantages of less complexity & shorter operation time (Table 1.2 & 1.3). The BA is associated with concerns of groin pain due to acetabular erosion which affects long term survival of the implant. There is no statistically significant difference between BA group & THA group in mean Harris Hip Score, general complication, revision rate, mortality and hospitalization days. However, operation time for THA is evidently longer and blood loss volume is significantly higher.
This is a retrospective study which bears some limitations such small sample size and shorter follow up period. A prospective randomized study with larger sample size and longer follow up is required.
Conclusion
In this study it is observed that functional score (HHS)is similar in both THA & BA group and there is no statistically significant difference in complication, revision, mortality rate and hospitalization days. Both THA and BA are reliable method for unstable intertrochanteric fractures in elderly osteoporotic patients. However, greater intraoperative blood loss, longer duration of surgery & high dislocation rate indicates that Bipolar hemiarthroplasty is better choice compared to Total Hip Arthroplasty.
References
- Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop. 2011 Jan;45(1):15-22.
View at Publisher | View at Google Scholar - Koval KJ, Zuckerman JD (1998) Hip fractures are an increasingly important public health problem. Clin Orthop Relat Res 348:2.
View at Publisher | View at Google Scholar - Said GS, Farouk O, El-Sayed A, Said HG (2006) Salvage of failed dynamic hip screw fixation of intertrochanteric fractures. Injury 37:194–202
View at Publisher | View at Google Scholar - Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG (1990) Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br 72:26–31
View at Publisher | View at Google Scholar - 5..Kim WY, Han CH, Park JI, Kim JY(2001)Failure Of Intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop 25(6):360–362
View at Publisher | View at Google Scholar - 6 Baumgaertner MR, Curtin SL, Lindskog DM (1998) Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop 348:87–94
View at Publisher | View at Google Scholar - Brostrom LA, Barrios C, Kronberg M, Stark A, Walheim G (1992) Clinical features and walking ability in the early postoperative period after treatment of trochanteric hip fractures. Results with special reference to fracture type and surgical treatment. Ann Chir Gynaecol 81:66–71.
View at Publisher | View at Google Scholar - Haentjens P, Casteleyn PP, De Boeck H, Handleberg F, Opedcam P (1989) Treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Primary bipolar arthroplasty compared with internal fixation. J Bone Joint Surg Am 71:1214–1225.
View at Publisher | View at Google Scholar - Haentjens P, Casteleyn PP, Opdecam P (1989). Primary bipolar arthroplasty or total hip arthroplasty for the treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Acta Orthop Belg 60(Suppl 1):124–128.
View at Publisher | View at Google Scholar - Tronzo RG (1974). The use of an endoprosthesis for severely comminuted trochanteric fractures. Orthop Clin North Am 5:679-681.
View at Publisher | View at Google Scholar - Stern MB, Goldstein T (1979). Primary treatment of comminuted intertrochanteric fractures of the hip with a Leinbach prosthesis. Int Orthop 3:67-70.
View at Publisher | View at Google Scholar - Chan KC, Gill GS (2000). Cemented hemiarthroplasties for elderly patients with intertrochanteric fractures. Clin Orthop 371:206-215
View at Publisher | View at Google Scholar - Green S, Moore T, Proano F (1987). Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop 224:169-177.
View at Publisher | View at Google Scholar - Haentjens P, Casteleyn PP, De Boeck H et al (1989). Treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Primary bipolar arthroplasty compared with internal fixation. J Bone Joint Surg Am 71:1214–1225.
View at Publisher | View at Google Scholar - Haentjens P, Casteleyn PP, Opdecam P (1994). Primary bipolar arthroplasty or total hip arthroplasty for the treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Acta Orthop Belg; 60[Suppl 1]:124–128
View at Publisher | View at Google Scholar - Harwin SF, Stern RE, Kulick RG (1990). Primary Bateman-Leinbach bipolar prosthetic replacement of the hip in the treatment of unstable intertrochanteric fractures in the elderly. Orthopedics 13:1131–1136
View at Publisher | View at Google Scholar - Pho RW, Nather A, Tong GO, Korku CT (1981). Endoprosthetic replacement of unstable, comminuted intertrochanteric fracture of the femur in the elderly, osteoporotic patients. J Trauma 21:792–797
View at Publisher | View at Google Scholar - Rodop O, KiralA, Kaplan H, Akmaz I (2002). Primary bipolar hemiprosthesis for unstable intertrochanteric fractures. Int Orthop 26:233–237
View at Publisher | View at Google Scholar - Stern MB, Angerman A (1987). Comminuted intertrochanteric fractures treated with a Leinbach prosthesis. Clin Orthop 218:75–80.
View at Publisher | View at Google Scholar - Sidhu AS, Singh AP, Singh AP, Singh S (2010). Total hip replacement as primary treatment of unstable intertrochanteric fractures in elderly patients. Int Orthop. 34(6): 789–792.
View at Publisher | View at Google Scholar

 Clinic
Clinic
