Case Report | DOI: https://doi.org/10.31579/2834-8664/022
Not just Typical Sinusitis, Granulomatosis with Polyangiitis: A Case Report
1 Florida State University College of Medicine.
2 Arnold Palmer Hospital for Children Pediatric Residency Group.
*Corresponding Author: Hanna Lateef, Florida State University College of Medicine.
Citation: Hanna Lateef, Austin West, Mariam Zeini, (2023), Not just Typical Sinusitis, Granulomatosis with Polyangiitis: A Case Report, International Journal of clinical and Medical Case Reports, 2(3); Doi:10.31579/2834-8664/022
Copyright: © 2023 Hanna Lateef, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 01 May 2023 | Accepted: 10 May 2023 | Published: 17 May 2023
Keywords: polyangiitis; granulomatosis; pulmonary
Abstract
Granulomatosis with polyangiitis (GPA) is a rare, life-threatening autoimmune Antineutrophil Cytoplasmic Antibody (ANCA)- associated vasculitis. GPA has the ability to affect small- to medium-sized blood vessels anywhere in the body, but it typically causes clinical manifestations in the upper and lower respiratory tract as well as the kidneys, yielding the characteristic triad of nasal, pulmonary, and renal involvement
Introduction
Granulomatosis with polyangiitis (GPA) is a rare, life-threatening autoimmune Antineutrophil Cytoplasmic Antibody (ANCA)- associated vasculitis. GPA has the ability to affect small- to medium-sized blood vessels anywhere in the body, but it typically causes clinical manifestations in the upper and lower respiratory tract as well as the kidneys, yielding the characteristic triad of nasal, pulmonary, and renal involvement [1]. GPA in pediatric patients presents with a higher prevalence of ear, nose, and throat involvement and milder presentations of weight loss, fever, and malaise in comparison to adults with GPA. Renal involvement is less common in the pediatric population [2]. GPA is more commonly reported in the adult population, with the peak incidence of disease being observed at 64-75 years of age [3]. The estimated incidence of GPA in a pediatric patient is 1:1,000,000, compared to the estimated yearly incidence in adults of 1:100,000 [4]. GPA has a strong predilection for affecting females over males and the Caucasian population over all other races with recorded GPA [5].
Case Presentation
A 17-year-old male with a complex past medical history including polysplenia, incomplete vena cava, and aortic dilation of the ascending aorta presented to the emergency department with worsening nasal congestion of six week’s duration. He had been recently diagnosed with a sinus infection at an outside facility and was unsuccessfully treated with two courses of Azithromycin, Ampicillin/Sulbactam, and steroids.
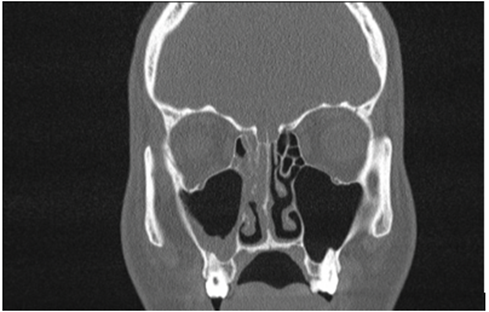
On arrival, the patient was afebrile and hypertensive at 141/72. Remarkable laboratory data revealed WBC 13,300, CRP 201.9, ESR 109, Anti-streptolysin O titer within normal limits, negative Mononucleosis screen, negative drug panel, and negative urinalysis. Autoimmune etiology was suspected. ANCA panel for vasculitis was obtained. Results later revealed positive c-ANCA and negative p-ANCA along with negative ANA screen. Computerized tomography (CT) scan of his sinuses demonstrated opacification of his right sinus (Figure 1). The patient was admitted to the pediatric unit for further evaluation and management.
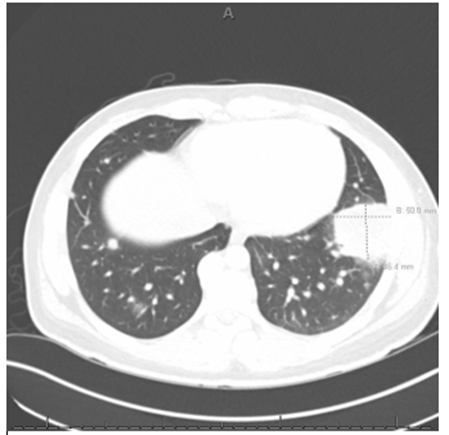
Viral atypical pneumonia PCR panel was unremarkable. Further work-up with chest x-ray revealed mass-like opacities in lungs concerning for malignancy. Follow-up CT with contrast was remarkable for bilateral non-cavitary pulmonary nodules and masses with concern for pulmonary metastatic disease versus pulmonary lymphomatous involvement versus atypical infection (Figure 2). The largest mass measuring 5.0 x 4.6cm, abutting the left pleura was targeted for CT-guided needle biopsy.
Infectious disease was consulted and recommended HIV antibody, HIV antigen, non-invasive pathogen blood test, and Quantiferon TB Gold lab tests, which were all unremarkable. Patient was started on a course of Linezolid for bacterial sinusitis prophylaxis. Hematology/oncology was consulted to assist in the work up of potential oncologic causes of patient’s lung nodules. LDH, uric acid, and AFP were ordered and were unremarkable. At this time, the results of the patient’s lung biopsy returned and demonstrated necrotizing granulomatous inflammation with no signs of malignancy. Pathology specimen staining was negative for fungal organisms and acid-fast organisms.
Due to suspicion for GPA, nephrology and rheumatology were consulted. Renal ultrasound was obtained and demonstrated normal appearing kidneys without increased echogenicity. Regarding his hypertension, renal etiology was not suspected. Rheumatology confirmed the diagnosis of GPA given the constellation of symptoms, laboratory evaluation, and imaging studies consistent with ACR classification criteria for GPA. The patient was started on a pulse dose of solumedrol and received his first infusion of Rituximab in the hospital. The patient was hemodynamically stable and was discharged with follow-up instructions to monitor for clinical progression of his disease.
Discussion
Granulomatosis with polyangiitis (GPA) is a small-to-medium vessel vasculitis with unclear pathogenesis. It is possible that multiple factors such as abnormalities in the innate and adaptive immune response, extrinsic antigens, and genetics combined may lead to the inflammation of blood vessels that result in the clinical manifestations of GPA [2] ENT manifestations such as recurrent sinusitis, lung involvement, and non-specific systemic symptoms such as fever and weight loss make this case a typical presentation of pediatric GPA [2].
While GPA is typically a disease of adulthood, it should remain on the differential for pediatric patients with multisystem involvement. Pediatric GPA patients have a hospitalization rate 1.3 times higher than that of adults with the disease. Morbidity and mortality of GPA is dependent upon early detection of the disease. Untreated GPA has a one-year mortality rate of approximately 90% compared to 90% five-year survivability with proper treatment [7]. The major long-term complications of GPA become side-effects of these treatments including, but not limited to: steroid induced side effects such as Cushing’s syndrome and osteoporosis, infections secondary to immunosuppression, and infertility [8].
Conclusion
GPA is a disease that typically affects adults; however, it has profound impacts on patients and must be identified early to reduce morbidity and mortality. Our patient with treatment-resistant sinusitis subsequently found to have non-cavitary lung nodules identified on CT provides a suitable framework for workup and treatment of suspected pediatric GPA patients.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- Martinez F, Chung JH, Digumarthy SR, et al. (2012). Common and uncommon manifestations of Wegener granulomatosis at chest CT: radiologic-pathologic correlation. Radiographics.;32(1):51-69.
View at Publisher | View at Google Scholar - Lynch JP, 3rd, Derhovanessian A, Tazelaar H, Belperio JA. (2018). Granulomatosis with Polyangiitis (Wegener's Granulomatosis): Evolving Concepts in Treatment. Semin Respir Crit Care Med.39(4):434-458.
View at Publisher | View at Google Scholar - Kubaisi B, Abu Samra K, Foster CS. (2016). Granulomatosis with polyangiitis (Wegener's disease): An updated review of ocular disease manifestations. Intractable Rare Dis Res. 5(2):61-69.
View at Publisher | View at Google Scholar - Bohm M, Gonzalez Fernandez MI, Ozen S, et al. (2014). Clinical features of childhood granulomatosis with polyangiitis (wegener's granulomatosis). Pediatr Rheumatol Online J.12:18.
View at Publisher | View at Google Scholar - Panupattanapong S, Stwalley DL, White AJ, Olsen MA, French AR, Hartman ME. (2018). Epidemiology and Outcomes of Granulomatosis With Polyangiitis in Pediatric and Working-Age Adult Populations In the United States: Analysis of a Large National Claims Database. Arthritis Rheumatol. Dec;70(12):2067-2076.
View at Publisher | View at Google Scholar - Calatroni, M., Oliva, E., Gianfreda, D., et al. (2017). ANCA-associated vasculitis in childhood: recent advances. Ital J Pediatr 43, 46.
View at Publisher | View at Google Scholar - Bohm M, Gonzalez Fernandez MI, Ozen S, et al. (2014). Clinical features of childhood granulomatosis with polyangiitis (wegener's granulomatosis). Pediatr Rheumatol Online J. May 26;12:18.
View at Publisher | View at Google Scholar - Arulkumaran, N., Jawad, S., Smith, S.W., et al. (2011). Long- term outcome of paediatric patients with ANCA vasculitis. Pediatr Rheumatol 9, 12.
View at Publisher | View at Google Scholar

 Clinic
Clinic
