Case Report | DOI: https://doi.org/10.31579/2834-5177/012
Mucocutaneous Manifestations During SARS-CoV-2 İnfection
- Lidaw Déassoua Bawè 1,2
- Awèréou Kotosso 1,2,3
- Bawoubadi Abaltou 1,2,3
- Akouda Akessiwe Patassi 1
- Abdou Razak Moukaila 2
- Christelle Adougba 2
- Koumateh Marzouk Afoda 2
- Gnozi Emmanuel Kanaza 2
- Amélé Déla Akpodo 2
- Abla Enyonam Hoehanou 2
- Gnimdou Tchamdja 4
- Majesté Ihou Watéba 1,2
1Department of Infectious and Tropical Diseases, Sylvanus Olympio University Hospital (Lomé, Togo)
2Regional Hospital of Lomé commune (Togo)
3Army Hospital of Lomé (Togo)
4Army medico-surgical clinic of Lomé (Togo)
*Corresponding Author: Lidaw Déassoua Bawè, Department of Infectious and Tropical Diseases, 12 rue de l’hôpital, Tokoin, Lomé, Togo.
Citation: Lidaw Déassoua Bawè, Awèréou Kotosso, Bawoubadi Abaltou, Akouda Akessiwe Patassi, Abdou Razak Moukaila, et all. (2023), Mucocutaneous Manifestations During SARS-CoV-2 Infection. International Journal of Clinical Infectious Diseases, 2(1); DOI:10.31579/2834-5177/012
Copyright: © 2023, Lidaw Déassoua Bawè. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 13 January 2023 | Accepted: 24 January 2023 | Published: 31 January 2023
Keywords: exanthema; angular cheilitis; erythrosis; sars-cov-2
Abstract
Respiratory symptoms are mainly seen in SARS-CoV-2 infection. However, cutaneous manifestations have been reported. We collected two cases of cutaneous and mucosal manifestations at the Regional Hospital of Lomé commune, the national reference center in Togo for the management of COVID-19. The clinical presentation was marked at the cutaneous level by cutaneous dryness with generalized desquamation, maculo-papular exanthema and erythrosis of the palms and soles. At the mucosal level, there was conjunctival hyperemia and angular cheilitis. The management consisted essentially in a good hydration and a local treatment based on antiseptic soap for the baths and application of dermocorticoid; treatments under which the evolution was favorable.
Introduction
SARS-CoV-2 infection is mainly manifested by respiratory symptoms, the most frequent being rhinitis, cough and dyspnea, which can lead in the most severe cases to severe acute respiratory syndrome. However, multiple organ involvement has been reported and the integument is no exception. With the emergence of this new virus, various cutaneous manifestations have been described [1].
Although this remains rare, integument involvement is more or less described depending on the country, ranging from 20.4% of patients (18 out of 88) in an Italian cohort to 1.8% (2 patients out of 1099) in a Chinese cohort. [1]
The first data on the issue came from Italy, one of the most affected countries in the world, where an initial viewpoint reported 20.4% of skin manifestations in a total of 88 patients with COVID-19 [2].
In Togo, we report two cases of cutaneous and mucosal manifestations related to SARS-CoV-2 infection.
Patients and method
From March 06, 2020, the date of diagnosis of the first COVID-19 in Togo until May 31, 2022, the Regional Hospital of Lomé commune, which is the national reference center for the management of COVID-19, recorded 3139 hospitalized patients, among whom 2 cases of cutaneous manifestations.
Ethical considerations
The anonymity of the patients was respected. The available images that we disseminated and that concerned a single patient do not allow any identification of the patient.
Observation 1
The patient is 28 years old; a military man who was tested positive for SARS-CoV-2 by Polymerase Chain Reaction (PCR) and who had no history of drug use or atopy. He had headache, fever, pruritus, intense asthenia and pruritic maculo-papular eruptions disseminated to all the integuments and evolving for 2 weeks. The examination on admission enabled to note:
-a hyperthermia at 39°4 C ;
-conjunctival hyperemia;
-dry skin with desquamation of the whole body and scalp + scratching lesions of the genitals; erythrosis of the palms and soles of the feet + angular cheilitis;
-maculo-papular exanthema.
Retroviral serology and HBsAg tests were negative.
Management was symptomatic with the use of antipyretics and analgesics (Paracetamol + Nefopam), good hydration, an antihistamine (Hydroxyzine), a bath with a local antiseptic soap (Chlorhexidine gluconate, Chlorocresol, Hexamidine di-istionate) and the use of dermocorticoid (Betamethasone Dipropionate).
The PCR was negative after 10 days. The evolution of the lesions was favorable after 15 days of hospitalization.
Observation 2
It is a 67-years-old patient, hypertensive, retired electrician. He has been tested positive for SARS-CoV-2 in a context of disabling joint pain, myalgias, fever, skin lesions and pruritus, all evolving for 3 weeks. The examination on admission enabled to note:
-an apyrexia;
-dry skin (picture 1), maculo-papular exanthema (picture 2) with generalized desquamation over the whole body (pictures 3 and 4) involving the scalp, hands, feet and genitals.
Annexe
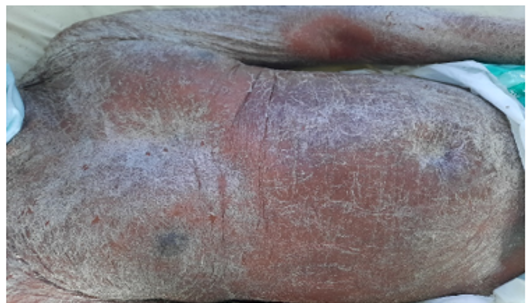
Picture 1: Dry Skin
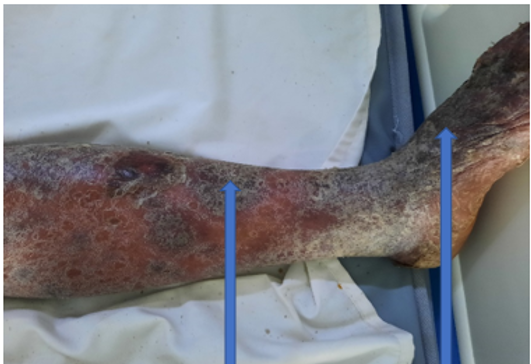
Picture 2: Maculo-papular exanthema of the lower limb

Picture 3: Dry Skin with Desquamation
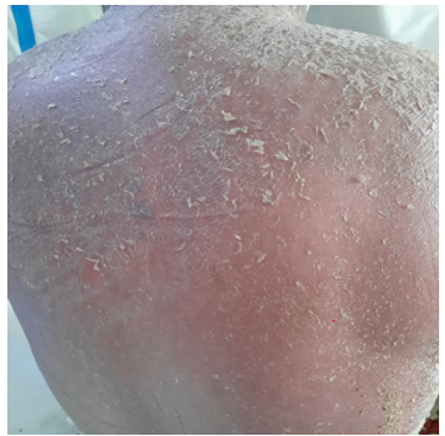
Picture 4: Desquamation of the beak
Retroviral serology and tests for hepatitis B and C were negative. He received local treatment with a bath based on local antiseptic soap (Chlorhexidine gluconate, Chlorocresol, Hexamidine di-istionate), a dermocorticoid (Betamethasone dipropionate) and an antihistamine (Hydroxyzine).The SARS-CoV-2 PCR became negative after 9 days and the evolution was favorable.Discussion The clinical manifestations related to the infection with the new coronavirus SARS-CoV-2 seem to be very polymorphic and multi-systemic, going far beyond the typically respiratory nosological framework. These manifestations can be cardiovascular, dermatological, ENT, hepatic, renal, ophthalmological and even neurological [3].
The first descriptions in Italy in 2020 reported signs of erythematous rash, generalized urticaria and vesicular lesions resembling chickenpox. The trunk was the main area involved. Itching was mild or absent and the lesions as a whole were not correlated with disease severity and resolved spontaneously [2]. Later, Schuhler et al. described the clinical presentation of SARS-CoV-2 skin involvement in three types namely: -paraviral rash consisting of macular and/or papular exanthema and urticarial rash made of highly pruritic edematous papules;-vesiculo-crusty eruptions;-and vasculitic eruptions including purpuric eruptions, pseudoengelations (erythematous macule or papule in the form of a plaque) and lividoid eruptions which are bluish lesions [1]. The manifestations observed in Morocco are an erythematopapular and papulovesicular rash on the trunk and lower limbs [4].
The COVID-Skin study of the French Society of Dermatology reports cutaneous signs such as facial rash, diffuse maculopapular exanthema, eczema, purpura/livedo, urticaria, vesicular rash, and thoracic placard [5].
The reported SARS-coV-2-related skin manifestations were often mild, but one case of Stevens-Johnson syndrome (SJS) associated with SARS-coV-2 infection was reported. It was a bullous exanthema, with skin erosions predominantly involving the trunk, upper extremities and face with a positive Nikolski sign. Erosions of the oral and genital mucosa and conjunctivitis were observed. The case was getting complicated with respiratory distress. In a pandemic context with respiratory symptoms and pyrexia, the SARS-CoV-2 PCR was positive. A chest CT scan showed lung involvement compatible with SARS-CoV-2 infection. Serological and PCR results for Mycoplasma pneumoniae and other infectious causes were negative. The drug hypothesis was unlikely considering the chronological score; the diagnosis of SJS secondary to SARS-CoV-2 infection was retained. The cutaneous evolution was rapidly favorable [6].
The physiopathology of cutaneous manifestations during SARS-CoV-2 infection is still poorly understood but two mechanisms seem to explain it. The first mechanism is an immune response to viral nucleotides as observed in viral exanthemata. The second mechanism is that the skin manifestations are secondary to an inflammatory/immune response to the presence of the virus in the body (as seen in vasculitis and thrombotic vasculopathies) [7].
Conclusion
Cutaneous and mucosal manifestations related to SARS-CoV-2 infection are very rare in Togo. Those collected since the beginning of the pandemic are mainly paraviral eruptions with a favorable evolution. The management was essentially symptomatic and consisted of good hydration, use of antipyretics and antihistamines. Locally, the use of dermocorticoids brought a good response to the treatment of skin lesions.
References
- Schuhler C, Alberto C, Toutous-Trellu L, Kaya G. (2021); Infection par le SARS-CoV-2 et manifestations cutanées. Rev Med Suisse 17: 642-645.
View at Publisher | View at Google Scholar - Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020; 34(5):e212-e213.
View at Publisher | View at Google Scholar - Kashongwe IM, Lepira FB, Situakibanza HNT, Makulo J-RR, Sumaili EK, Kayembe J-MN. Manifestations cliniques de l’infection à Coronavirus SARS-Cov-2 (COVID-19). Ann. Afr. Med. 2020 ; 13 (3) :e3685-e3693.
View at Publisher | View at Google Scholar - El Jazouly M, Chahboun FZ, Chiheb S. Les manifestations cutanées au cours du COVID-19: état des lieux. Pan African Medical Journal. 2020;35(2):132. 10.11604/pamj.supp.2020.35.132.24842.
View at Publisher | View at Google Scholar - Guelimi R, Salle R, Dousset L, Assier H, Fourati S, Barbarot S, Boulard C, Bourseau Quetier C, Cambon L, Cazenave C, Colin A, Kostrzewa E, Lesort C, Levy Roy A, Lombart F, Marco-Bonnet J, Monfort J-B, Samimi M, Tardieu M, Sbidian E, Wolkenstein P, Le Cleach L, Beylot-Bary M, et Société Française de Dermatologie. Manifestations cutanées au cours l’épidémie de COVID-19 : étude COVID-Skin de la Société française de dermatologie. Ann Dermatol Venereol. 2020; 147(12): A135.
View at Publisher | View at Google Scholar - Sergeant M, Monitor L, Barbier C-M, Colné J, Bursztejn A-C. Syndrome de Stevens-Johnson secondaire à une infection à SARS-CoV-2. Annales de Dermatologie et de Vénéréologie 2020 ; 147(12):A202-A203.
View at Publisher | View at Google Scholar - Kaya G, Kaya A, Saurat JH. Clinical and Histopathological Features and Potential Pathological Mechanisms of Skin Lesions in COVID-19: Review of the Literature. Dermatopathology (Basel) 2020;7:3-16.
View at Publisher | View at Google Scholar

 Clinic
Clinic
