Research Article | DOI: https://doi.org/10.31579/2835-7949/015
Menstrual Problems: Menorrhagia And Primary Dysmenorrhagia
1Riggs Pharmaceutic Department of Pharmacy University of Karachi-Pakistan.
2GD Pharmaceutical IncOPJS University Rajasthan India.
*Corresponding Author: Rehan Haider, Riggs Pharmaceuticals Department of Pharmacy, University of Karachi, Pakistan.
Citation: Rehan Haider, Geetha Kumari Das, (2024), Menstrual Problems: Menorrhagia and Primary Dysmenorrhagia, Biomedical Research and Clinical Trials,3(1); DOI: 10.31579/2835-7949/015
Copyright: © 2024, Rehan Haider. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 February 2024 | Accepted: 12 February 2024 | Published: 20 February 2024
Keywords: menstrual problems, menorrhagia, basic dysmenorrhea, difficult menstrual extortion, severe menstrual cramps, chlorosis, prostaglandin, hormonal cure, uterine Fibroids, pain remedy, treatment alternatives, mother's health, quality of growth.
Abstract
Menstrual problems can considerably affect a girl's status in life, accompanied by two universal issues: menorrhagia and basic dysmenorrhea. Menorrhagia, characterized by difficult menstrual draining, is a condition in which a woman experiences extended periods or excessive blood flow. This condition may incapacitate you, leading to blood deficiency, fatigue, and public restraints. The underlying causes of menorrhagia can change, including hormonal imbalances, uterine Fibroids, or added medical environments, which typically include a particularized record of what happened and a physical examination attended by potential situations such as cure, hormonal therapy, or surgical attack.
Primary dysmenorrhea, in another way, refers to harsh menstrual cramps without some fundamental healing condition. It is a common issue among daughters and usually occurs during the first few days of the period. The exact cause of basic dysmenorrhea is not well understood; however, it is expected to be associated with prostaglandin production and uterine shortening. Women with primary dysmenorrhea grant permission for sharp, incapacitating pain, nausea, and additional discomfort, which upset their regular lives. Management options include pain relievers, hormonal contraceptives, behavioral changes, and heat therapy.
Introduction
Menorrhagia and dysmenorrhea are significant gynecological diseases. This is not surprising, since women experience about 400 menstruation between menarche and menopause. Menorrhagia is the main complaint in women referred to gynecologists, and accounts for most hysterectomies and nearly all endometrial ablative procedures.
Menorrhagia (heavy blood loss
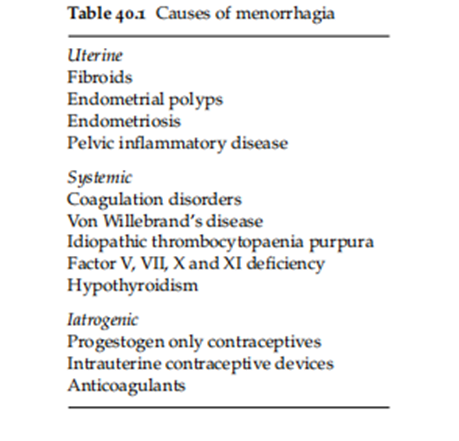
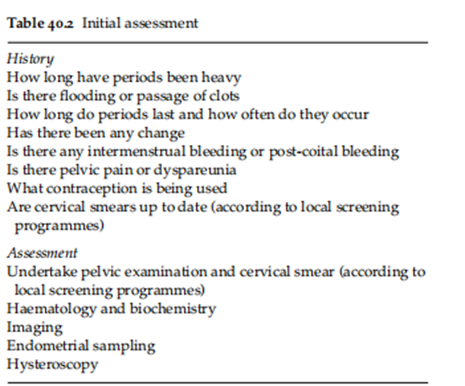
This finding indicates that endocrine abnormalities are frequently probable. However, most cases of menorrhagia are guided by balanced ovulatory cycles and ovular phases, which are likely to occur before menarche or Perimenopause. The presentation and number of patients with menorrhagia usually complain of increased menstrual misfortune, requiring more sanitary protection, or the transition of clots and inundation. The assessment results are listed in Table 40.2. Of note, women find this difficult to find. worship to correctly evaluate ancestral loss. Thus, in dispassionate practice, only 40% of mothers object to menorrhagia and have measured misfortunes of more than 80 mL [3]. The salty hematin procedure is considered the gold standard for weighing menstrual blood misfortune [2]. Here, clean ploys were saturated in 5% sodium hydroxide to convert the blood to soluble hemoglobin, whose optimal state bulk was then calculated. Because it is not usually applicable, various graphic notch wholes exist, but dependability is contradictory [3–5]. Furthermore, recent technological changes in the manufacturing of sanitary towels mean that these pictorial methods need to be re-validated. Measurement of total menstrual fluid using a weighing technique has been described as sufficiently accurate for clinical purposes but requires further evaluation [5].
Investigations
Haematology And Biochemistry
A full blood count should be performed in all women complaining of menorrhagia since it is a common cause of anemia [1]. Testing for bleeding disorders should only be performed if clinically indicated, for example, menorrhagia since menarche and a history of bleeding after dental extractions and childbirth [4, 6]. Thyroid function tests should only be performed if clinically indicated. No other endocrine investigations are warranted.
Imaging
Transvaginal sonography (TVS) is usually the first investigation. TVS measures endometrial thickness and diagnoses polyps and leiomyomata with a sensitivity of 80% and a specificity of 69% [7]. It is well established that endometrial thickness measured by TVS is indicative of the pathology in postmenopausal women. However, the exact cut-off values for endometrial thickness measurement in the ability of premenopausal women to predict endometrial neoplasia is subject to debate. The British ‘RCOG Guideline Development Group’ analyzed several Studies have concluded that 10–12 mm is a reasonable cut-off when using TVS, preferably undertaken in the follicular phase, as a method before more intensive procedures of endometrial assessment [5, 8]. TVS can be enhanced using sonohysterography or color flow Doppler, but its availability may be limited [9, 10].
Endometrial Sampling
The purpose of endometrial sampling for menorrhagia is to exclude or diagnose endometrial cancer or hyperplasia. Endometrial sampling is recommended in women aged more than 40 years, and those with an increased risk of endometrial malignancy. Significant risk factors for the development of endometrial carcinoma are obesity, diabetes mellitus, hypertension, chronic anovulation, nulliparity with a history of infertility, family history of endometrial and colonic cancer, and tamoxifen therapy [5]. In younger Endometrial sampling can also be indicated if abnormal bleeding does not resolve with medical treatment. polycystic ovary syndrome, in which endometrial hyperplasia is a common finding in endometrial assessment Maybe it is necessary if abnormal bleeding is presenting symptoms or suspicious sonographic endometrial features are observed [5, 8].
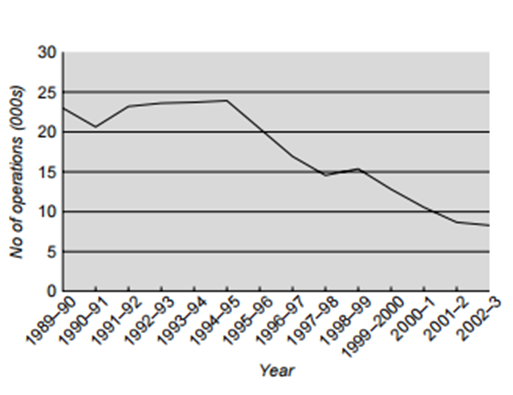
Fig: 40.1 Numbers of hysterectomies for menorrhagia between 1989/90 and 2002/3 in NHS Trusts in England. (Reid and Mukri [12]). Reproduced with permission from the BMJ Publishing Group
The most common methods of endometrial sampling are as follows:
• Aspiration curettage (Pipelle, Vabra)
• Dilatation and curettage (D&C)
• Hysteroscopy
‘One-stop’ outpatient services based on initial TVS may reduce the need for further procedures such as Hysteroscopy [11].
Management
Management has changed over the past two decades with the introduction in the mid-1980s of therapeutic endoscopic endometrial destructive procedures and the levonorgestrel-releasing intrauterine device in the UK in 1995.The number of hysterectomies for menorrhagia was estimated to have decreased by 36?tween 1989 and 2002 [6, 12] (Fig. 40.1). In addition, an inverse social gradient has been observed in hysterectomy, with surgery being inversely related to social class and education, especially at younger ages [7,13]
Drug therapy
Therapy aims to reduce blood loss, reduce the risk of anemia, and improve quality of life. Medical therapy is indicated when there is no obvious pelvic abnormality and the woman wishes to retain her fertility. As menstrual loss, in the absence of pathology, does not change markedly, treatment is long-term. Thus, the preferred drug procedure must solve a problem, have few or mild reactions, and be suitable for the patient. It is mainly to determine drug cures in terms of lowering calculated menstrual ancestry misfortune by way of the poor equivalence between two points: the objective and emotional amount of menstrual ancestry misfortune. Medical therapy may be divided into two main classes:
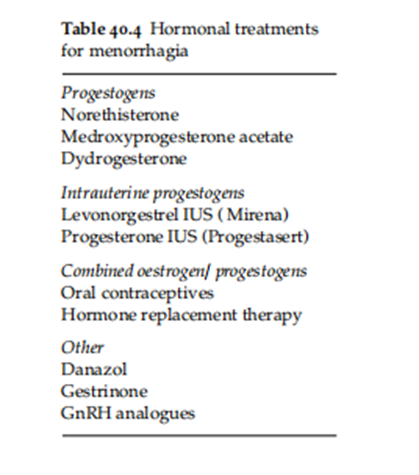
non-hormonal and hormonal factors The old contains non-steroidal antagonistic-inflammatory drugs and antifibrinolytics. and the concluding progestogens, spoken contraceptives, and birth control methods substitute cure, danazol, gestrinone, and GnRH analogs (Tables 40.3 and 40.4). Non-hormonal treatment is captured throughout the entire period and concedes the possibility of being a first-line in first-contact medical care, utilizing either mefenamic acid or tranexamic acid; both may be secondhand together, but skilled are worthless studies of the effect of the blend. Referral should be considered whether prostaglandin synthesis inhibitors or antifibrinolytics agents are effective after 3 months of therapy [1].
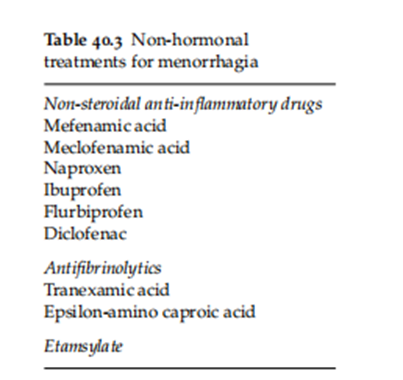
Non-Hormonal
enzymes, Non-steroidal anti-inflammatory drugs The cyclooxygenase (COX) pathway with its two enzymes, cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) 2) is one of the major routes for the oxidative metabolism of arachidonic acid to prostaglandins. The demonstrated involvement of prostaglandins in the genesis of menorrhagia points to cyclooxygenase inhibitors as a potentially effective treatment. Cyclooxygenase inhibitors, commonly referred to as non-steroidal anti-inflammatory drugs (NSAIDs), can be chemically classified and divided into two main groups: COX-1 inhibitors: salicylates (aspirin), indoleacetic acid analogs (indometacin), arylpropionic acid derivates (naproxen, ibuprofen), fenamates (mefenamic acid, flufenamic acid, meclofenamic acid) and COX-2 inhibitors: coxibs (celecoxib). Various NSAIDs have been evaluated in several randomized trials and have, to date, been limited to COX-1 inhibitors. In a Cochrane review, five of seven randomized trials showed that the mean menstrual blood loss was less with NSAIDs than with placebo, and two showed no difference [8, 14]. Furthermore, there was no evidence that one NSAID (naproxen or mefenamic acid) were superior to other NSAIDs. Fenamates (e.g., mefenamic acid) are the most extensively studied NSAIDs. They have the unique property of inhibiting prostaglandin synthesis and binding to prostaglandin receptors, which are significantly increased in the uterus of women with menorrhagia [15]. Reductions in menstrual blood flow range from 22 to 46% with this therapy. About long-term therapy, a follow-up of 12 to 15 months after commencing treatment showed continuing efficacy of the NSAID mefenamic acid [16]. Reduction in menstrual blood loss has also been evaluated for other NSAIDs, such as naproxen, ibuprofen, sodium diclofenac, and flurbiprofen. The percentage of blood loss reduction varied from 25 to 47%, depending onell-indulgeRegarding the agent and dosage used [15], Furthermore, they are also effective for women using copper or non-hormonal intrauterine contraceptive devices. An additional benefit is that these drugs also alleviate the symptoms of dysmenorrhea. It is difficult to define the optimal doses and schedules.
Most studies, however, analyzed regimens starting on the first day of menstruation and continuing for five days or until the cessation of menstruation. Common side effects of NSAIDs include gastrointestinal irritation and the inhibition of platelet aggregation. Specific inhibitors of COX-2 might be more satisfactory in the case of menorrhagia, but there is excellent doubt about the security of this class of drugs [17].
Antifibrinolytics
Plasminogen electrical device inhibitors have thus been supporting menorrhagia by raising endometrial fibrinolytic ventures in women with menorrhagia, which is an artificial lysine derivative that utilizes the allure antifibrinolytics effect by reversibly obstructing lysine-binding sites on plasminogen and thus forestalling fibrin shame [18]. Tranexamic acid, 2 to 4.5 g/epoch for Four to seven days reduced menstrual ancestry flow by 34–59% over two to three eras. The effect was superior to that of the placebo. mefenamic acid, flurbiprofen, ethamsylate, and spoken luteal development of norethisterone at clinically appropriate dosages [9, 19]. Antifibrinolytics are too persuasive in women accompanying policeman or non-hormonal intrauterine designs [18, 19]. Tranexamic Acid is regularly w. These side effects are mainly restricted to mild gastrointestinal discomfort. A Cochrane review established no meaningful increase in stated events accompanying antifibrinolytics remedies distinguished from fake pills or added treatments [9, 19]. Earlier hypothetical concerns about thromboembolism leading to the antifibrinolytics operation of tranexamic acid have been refuted by general studies.
Ethamsylate
Ethamsylate is an idea to act by reducing blood flow pathway frangibleness, although the exact systems are changeable. Studies with objective MBL calculations utilizing monthly, regularly urged doses show that they are useless [1, 5, 8].
Hormonal Treatments
Progestogens
The use of progestogens has established the erroneous idea that daughters with accompanying menorrhagia mainly have anovula-conservative cycles, for which a progestogen supplement is necessary. Progestogens are the prevailing medicine for wives complaining of menorrhagia. Oral, intrauterine, and intramuscular depot injections were administered. The last is used primarily for birth control and skills concerning menorrhagia. Oral administration. Traditionally, the presidency was at the luteal point. However, studies with a calculated menstrual deficit accompanying luteal administration for 7 days of norethisterone 5 mg twice regularly show either a decrease or an increase in flow [10, 20]. However, norethisterone 5 mg three times daily from day 5–26 is effective [21]. Side effects include weight gain, headaches, and bloating. Intrauterine Administration. Intrauterine administration, especially of levonorgestrel (LNG), is very effective. There are currently two progestogen-impregnated devices: the Mirena intrauterine system (IUS) (Schering, Germany), which delivers 20 µg of LNG over 24 hours for about 5 years, and Progestasert (Alza Pharmaceuticals, USA), which releases about 65 µg of progesterone over 24 hours for approximately 16 months. Other newer, so-called frameless devices are currently being evaluated.
Mirena IUS (LNG-IUS) reduces menstrual blood loss by up to 96 and 20% of women using the LNG-IUS are reported to be amenorrheic after one year [11, 22]. Over In 3 years, 65% of the women with LNG-IUS continued to report improved menstrual bleeding. In addition to reducing menstrual blood loss, LNG-IUS may alleviate symptoms of dysmenorrhea and reduce the incidence of pelvic inflammatory disease. The LNG-IUS also provides effective contraception. The results are comparable to those of endometrial resection [12, 23], and they can be employed as an alternative to hysterectomy [24]. The main adverse effects associated with LNG-IUS are variable bleeding and spotting, particularly within the first few months of use. LNG-IUS is also sometimes associated with the development of ovarian cysts, but these are usually symptom less and show a high rate of spontaneous resolution. Compared with other medications and hysterectomy, LNG-IUS is much cheaper per menstrual cycle unless it is removed before five years. LNG-IUS showed similar efficacy and patient satisfaction at much lower costs ($1530 for IUS versus $4222 for hysterectomy) [24]. It also preserves fertility while providing contraception and progestogen for systemic hormone replacement therapy in perimenopausal women. Progestasert was the first hormonally implanted device; however, prospective randomized studies on menorrhagia are lacking. The main disadvantage of this device is its association with an increased risk of ectopic pregnancy.
Oestrogen/progestogen
From clinical experience, oral contraceptive pills (OCPs) are generally considered effective in the management of dysfunctional menstrual bleeding. However, few data points are available to support this observation [13, 25]. Data for hormone replacement therapy is limited.
Danazol. Danazol is an isoxazole derivative of 17α-methyltestosterone that acts on the hypothalamic-pituitary axis as well as on the endometrium to induce atrophy. Danazol reduced menstrual blood loss by up to 80% from baseline. Higher doses of danazol (≥200 mg/day) seem to be more effective than low-dosage therapy [26]. Its Clinical use of gestrinone is limited by androgenic side effects, which occur in up to three-quarters of patients. Gestrinone is a 19-testosterone derivative with anti-progestogenic, anti-estrogenic, and androgenic activities. In a placebo-controlled study, it reduced menstrual blood loss in 79% of patients with objective menorrhagia [27]. However, it also causes androgenic side effects. Gonadotropin-releasing hormone agonists Gonadotropin-releasing hormone (GnRH) agonists, administered continuously or in depot form, downregulate the expression of GnRH receptors, which blocks gonadotropin secretion from the anterior pituitary This leads to ovarian suppression. GnRH is mainly used to treat fibroid-associated bleeding [28]. Concerns about the long-term effects of ovarian suppression, such as osteoporosis, generally limit its use beyond 6 months, even when add-back therapy and estrogen/progesterone hormone replacement therapy are used in conjunction. The anti-progestational agent Mifepristone (RU-486) is a synthetic 19-norsteroid with Anti-progestogen activity inhibits ovulation and disrupts endometrial integrity. A systematic review showed that it induces amenorrhea and reduces leiomyomas size [29]. However, a notable adverse effect is the development of endometrial hyperplasia.
Surgery
Surgery may be necessary to treat pelvic abnormalities, such as polyps, Fibroids, chronic pelvic inflammation, disease, or endometriotic masses. Operations should be as conservative as possible for women who wish to retain fertility. Surgery included the removal of endometrial polyps, endometrial destruction, myomectomy, and hysterectomy. Mucous Fibroids or endometrial.
The polyps should be removed hysteroscopically. the most common [14, 30]. The latter has the potential for short hospital stays (1 day or less), but is currently frequently used in the UK [14, 30]. Hysterectomy should be offered only to women whose families are complete. The complications associated with a hysterectomy are often underestimated.
The VALUE study in England and Wales is a recent assessment of complications [14, 30]. Unfortunately, only 45% of these cases have been reported. Overall, operative complications occurred in 3.5% of patients, with 9% receiving postoperative recommendations. The death rate 6 weeks after surgery was 0.38 per 1000. Visceral damage occurred in 0.76% of the patients after TAH. 0.61% and 1.13?ter VH and LAVH, respectively. Significant bleeding was found in 2.3% of TAH cases, 1.9?ter VH, and 4.2?ter LAVH. Following LAVH, 1.5% of the women returned to the theater, compared to 0.7?ter TAH or VH. In a study from the USA, the fever rate after TAH was Blood transfusion was required in 30% and 15% of the patients, respectively [31]. Pyrexia occurred in 15% of cases after VH. A bowel injury occurred in 3:1000 women following abdominal hysterectomy and 6/1000 after a vaginal hysterectomy. The urinary tract was damaged in 3/1000 after an abdominal hysterectomy but in 14/1000 with the vaginal route. Mortality was 1/1000. Long-term sequelae A hysterectomy may or may not be accompanied by oophorectomy and may be total or subtotal. Even if the ovaries are conserved, there are concerns that menopause may occur early. Other concerns include mental well-being, psychosexual dysfunction, and urinary tract and bowel symptoms.Bilateral oophorectomy or surgical menopause results in an immediate menopause, which may be intensely symptomatic. Hysterectomy without oophorectomy can induce ovarian failure either in the immediate postoperative period, where in some cases it may be temporary, or at a later stage, where it may occur sooner than the time of natural menopause, that is, 51. Early ovarian failure increases the risk of developing cardiovascular disease and osteoporosis. The diagnosis of ovarian failure is more difficult in the absence of menstrual function. A case could be made for annual follicle-stimulating hormone (FSH) estimation in women who have had a hysterectomy before the age of 40.
There is currently a vogue for subtotal hysterectomy. with the understanding that sexual function is better preserved than with a total hysterectomy. The downside is that cervical smears have to be continued. Also, there may be some endometrium in the cervical stump, and this has been reported in 7% of women [15, 32]. This UK randomized trial found that neither subtotal nor total abdominal hysterectomy adversely affects urinary, bowel, or sexual function at 12 months [15, 32]. A Dutch study found that sexual pleasure improves after vaginal hysterectomy, subtotal abdominal hysterectomy, and total abdominal hysterectomy. The prevalence of one or more bothersome sexual problems 6 months after vaginal hysterectomy, Subtotal abdominal hysterectomy and total abdominal hysterectomy were 43% (38/89), 41% (31/76), and 39% (57/145), respectively [16, 33].
In the late 1970s, it was believed from retrospective studies that hysterectomy increased psychiatric morbidity, but this was refuted by subsequent prospective studies. This has been confirmed in a study of total versus subtotal hysterectomy [34]. All women showed an improvement in psychological symptoms following both operations, and no difference was found between the two procedures.
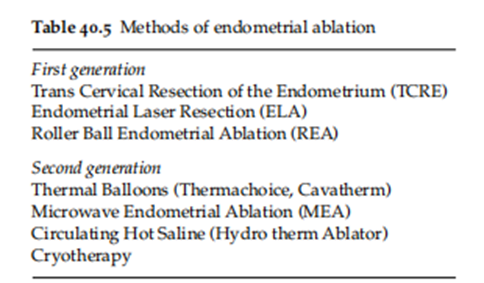
Endometrial Ablation
There are two classes of methods, with the second generation not requiring hysteroscopic skills (Table 40.5). The advantage of these methods is that hospital stays are much shorter, being 1 day rather than 5–6 for VH or TAH. Like hysterectomy, these treatments should only be offered to women who desire no further children. Several factors affect clinical outcomes. Women older than 45-year-olds are more likely to become amenorrhoeic. Adenomyosis has been associated with a higher failure rate of first-generation techniques. The reported incidence of intra-operative complications is relatively low, at about 1%. The most common complications are hemorrhage, perforation, need for emergency surgery, and absorption of a distending medium (radiofrequency-induced thermal Ablation, microwaves, and thermal balloons do not use a distending medium. The MISTLETOE study (Minimally Invasive Surgical Technique—Laser, Endothermal, or Endo resection) showed that uterine perforation and hemorrhage were more common with TCRE, and fluid overload occurred more frequently with laser ablation. While some of the variability in the rates of complications can be explained by inherent differences between the treatment modalities, there were also considerable differences in training and supervision, as 52% of doctors use the resectoscope alone, compared to only 7% using rays of light. Most snags were attacked in the first 100 cases by an individual physician [17,35]. A concern is the need for repeat surgery, such as hysterectomies. Reported rates change by an order of 21% at 6.5 years of age [36]. A systematic review has established few meaningful differences between the consequences of first- and second-era methods containing bleeding and delight, status-of-history measures, and repeat resection rates. Second-era techniques had considerably smaller operating and troupe opportunities, and they gave the impression of hardly any weighty perioperative antagonistic belongings [18, 37]. While the likelihood of later gestation endometrial devaluation due to use is depressed, the commonality has been stated as expected at 0.7%, accompanying an assortment of difficulties and adverse outcomes for the blastula. Women are the ones who withstand this procedure, thus becoming aware of the information needed to use persuasive birth control.
Decision aids
The conclusion is that increasing patient partnership in situations is mainly on account of the wide selections available. Decision-acquired immune deficiency syndrome involves a variety of formats, including leaflets, audiotapes, conclusion boards, calculating programs, videos, websites, and structured interviews. These were checked in a randomized controlled trial accompanying two-year-old inquiries of 894 daughters [19, 38]. Women were randomized to the control group, the news alone group (pamphlet and program), or the news plus interview group (interview).
Hysterectomy rates were lower for wives in the interview group (38%) (adjusted advantage percentage [OR]) than in the control group (48%), and daughters received the information unique (48%). The interview group had a lower mean cost ($1566) than the control group ($2751) (mean difference, $1184; 95% CI, $684–$2110), and the facts group $2026 (mean dissimilarity, $461; 95% CI, $236–$696). Thus, providing daughters with unique information did not influence situational selections; however, the addition of an interview to explain principles and obtain weaknesses had a significant effect on women’s management and resulted in decreased costs.
Dysmenorrhoea
Derived from the Greek aim of troublesome monthly flow, complete dysmenorrhoea has an equal mean hard brothers situation. Dysmenorrhoea may be classified as either the mother of Jesus or a subordinate. In the erstwhile type of skill, there is no pelvic study of plants, while the latter indicates fundamental physiology that leads to an arduous period.
Primary dysmenorrhoea
The predominance of dysmenorrhoea is extreme. A Swedish study found that 72% of 19-period-traditional daughters stated dysmenorrhoea, nearly 40% commonly used secondhand drugs for the pain, and 8% stopped being absent from work or school at every period [39]. According to an American study, 60% of brothers strutting young daughters endured dysmenorrhoea, and 14?ily missed school [40].
Primary dysmenorrhoea is guided uterine hyper contractility from overdone size and frequency of shortenings and an extreme ‘inactive’ attitude between shortenings. During shortenings, endometrial ancestry flow is diminished and there appears to be a good equilibrium between minimal ancestry flow and maximum colicky pain, favoring the idea that ischemia due to hyper contractility causes basic dysmenorrhoea. Prostaglandin and leukotriene levels are elevated in fathers' menstrual fluid and uterine fabric of wives accompanying dysmenorrhoea as are systemic levels of vasopressin.
Presentation and assessment
In general, basic dysmenorrhoea occurs 6–12 months after the menarche, when ovulatory phases start to settle. The early cycles following in position or time the menarche are usu partner an ovular and likely expected painless. The pain ordinarily resides in lower intestinal cramps and backaches, and there may be mixed gastrointestinal disturbances, such as looseness of the bowels and disgorging. Symptoms occur predominantly all along the first 2 days of the period.
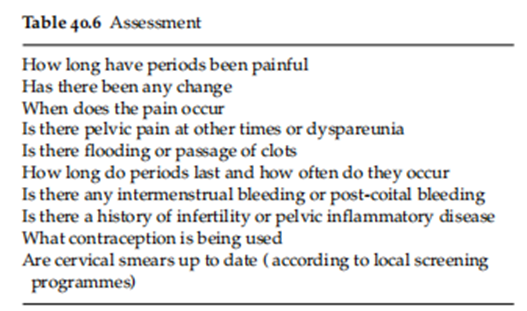
The disease of basic dysmenorrhoea is one of expulsion (Table 40.6). If manifestations are usual of basic dysmenorrhoea, a therapeutic trial can be entered before seeing some examination and review, particularly in juveniles. If dispassionate evaluation raises suspicion of subordinate dysmenorrhoea, transvaginal sonography (TVS), attractive reverberation depiction (MRI), or Laparoscopy should be thought out. Similarly, if syndromes of basic dysmenorrhoea are not relieved with either NSAIDs, the combined oral contraceptive pill or the combination of the two secondary causes of dysmenorrhoea need to be considered. Secondary dysmenorrhoea should also be suspected if symptoms are initially typical of primary dysmenorrhoea and worsen in duration (starting premenstrually) and intensity.
Management
Women will usually seek medical advice when seeking self-help measures such as heat and over-the-counter NSAIDs have failed [41]. The mainstays of treatment are NSAIDs and the combined oral contraceptive pill, especially when fertility control is required.
Non-Steroidal Anti-Inflammatory Drugs
Meta-analysis shows that COX-1 inhibitors such as mefenamic acid, naproxen, ibuprofen, and aspirin are all effective [20, 21, 42, 43]. Ibuprofen is the preferred analgesic because of its favorable efficacy and safety profiles [20, 42, 44]. Commencing treatment before the onset of menstruation appears to have no demonstrable advantage over starting treatment when bleeding starts. This observation is compatible with the short plasma half-life of NSAIDs. The advantage of starting treatment at the onset of menstruation is that it prevents the patient from treating herself when she is unknowingly pregnant, which would only become apparent when a period is missed. It is interesting to note that traditional healers have used plants with significant COX-inhibitory activity to treat menstrual pain [45]
The Combined Oral Contraceptive Pill
Although commonly used, clinical trial evidence supporting the efficacy of combined oral contraceptives in primary dysmenorrhoea is limited. They are thought to act by inhibiting ovulation and decreasing endometrial production of prostaglandins and leukotrienes by inducing endometrial atrophy and therefore reducing the amount of endometrial tissue available to produce these mediators [23,]. However, most of the clinical trials were undertaken with contraceptives with higher doses of hormones than those currently used [24-31].
Other Hormonal Methods
Although primarily designed for parous women, the LNG-IUS may be an effective treatment for nulliparous women who have a contraindication to either NSAIDs or the combined oral contraceptive. In women aged 25–47 years, the frequency of menstrual pain decreased from 60 to 29?ter 36 months of use of the device [48]. Other alternatives include depot progestogens used for contraception. Clinically, they are effective since they render most women amenorrhoeic, but clinical trial data are scant. Some of the new progestogen-only contraceptive pills (e.g., 75 mcg desogestrel) effectively inhibit ovulation and thus probably relieve the symptoms of dysmenorrhoea.
Other Methods
Several other pharmaceutical agents exist that alleviate the symptoms of dysmenorrhoea. An orally active vasopressin receptor antagonist is effective. Beta-adrenergic agonists and calcium channel blockers can reduce uterine contractility and thus are potentially effective, but clinical trials have not been undertaken. Transdermal glyceryl trinitrate has also been evaluated. A placebo-controlled trial found both placebo and vitamin E are effective in relieving symptoms due to primary dysmenorrhoea, but the effects of vitamin E are more marked. A randomized control study found supplementation with omega-3 polyunsaturated fatty acids beneficial in the management of dysmenorrhoea in adolescents. The mode of action is presumed to involve altered prostaglandin biosynthesis.
Research Method:
The research proposed to explore menstrual problems, expressly menorrhagia and basic dysmenorrhea, to better understand their prevalence, causes, and management. An assorted-systems approach was working to collect and resolve dossiers.
For the determinable facet of the research, a survey was administered to a different sample of wives of generative age (18–45 years) to draw news about the commonality and asperity of menorrhagia and primary dysmenorrhea. The survey contained questions related to syndromes, a record of what happened, and the impact of these menstrual problems on the colleagues' regular lives. Data were collected through online surveys and resolved using a mathematical operating system to identify styles and friendships.
For the subjective component, in-depth interviews were conducted, accompanying a subspace of the survey, with the accused, who stated experience with menorrhagia and basic dysmenorrhea. These interviews aimed to gain a deeper understanding of the private occurrences, management plans, and challenges faced by things accompanying these menstrual issues.
Result:
The determinable data reasoning showed that a solid portion of the surveyed daughters knew about menorrhagia and basic dysmenorrhea, with 45% reporting difficult menstrual grieving (menorrhagia) and 60% reporting severe menstrual cramps (basic dysmenorrhea). Furthermore, a meaningful imbricate was noticed, with 30% of partners experiencing two conditions together. These environments were raised to have a substantial impact on the members' features of existence, including misplaced work or the best time of life and deteriorated friendly activities.
The concerning qualities, not quantities, interviews supported valuable visions into the emotional and material toll of these menstrual questions. Many players meant frustration accompanying the restricted situation alternatives and the societal taboo encircling considering period openly. Coping means categorized from investment in company pain cure to lifestyle modifications and psychological support from companions and classification.
Discussion:
The findings imply that menorrhagia and basic dysmenorrhea are universal and repeatedly co-occur with mothers of generative age. These conditions have a solid effect on people's everyday lives, often due to misplaced time and diminished comfort. The shame guide reviews menstruation remnants as an impediment to pursuing help and support, emphasizing the need for upgraded instruction and knowledge.
The study climaxes on the importance of approachable and persuasive situational alternatives for managing these environments. Health professionals concede the possibility of being better equipped to recognize and address menorrhagia and basic dysmenorrhea, adjusting situational plans to individual needs. Additionally, public health campaigns and instructional drives are unavoidable to reduce the shame encircling menstrual questions and help open discussions.
Conclusion
Addressing menstrual problems like menorrhagia and primary dysmenorrhea is vital for enhancing the quality of life and overall well-being of affected individuals. This research underscores the significance of a multidimensional approach, combining quantitative and qualitative methods, to gain a comprehensive understanding of these issues and inform more effective interventions and support systems.
Acknowledgment
The completion of this research project would not have been possible without the contributions and support of many individuals and organizations. We are deeply grateful to all those who played a role in the success of this project We would also like to thank my mentor, Naweed Imam Syed, Prof. Department of Cell Biology at the University of Calgary, and Dr. Sadaf Ahmed Psychophysiology Lab, University of Karachi, for their invaluable input and support throughout the research. Their insights and expertise were instrumental in shaping the direction of this project.
Declaration of Interest
I at this moment declare that:
I have no pecuniary or other personal interest, direct or indirect, in any matter that raises or may raise a conflict with my duties as a manager of my office Management
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Financial support and sponsorship: No Funding was received to assist with the preparation of this manuscript
References
- Kho, adequate. A., & Shields, J. K. (2020). Analysis and administration of number one dysmenorrhea. JAMA, 323, 268–269. https://doi.org/10.1001/napping clothes.2019.16921
View at Publisher | View at Google Scholar - Iacovides, S., Avidon, I., & Baker, F. C. (2015). What we pay interest on about number one dysmenorrhea modern-day: A fault-finding evaluation. Human reproduction replaces 21,762–778.
View at Publisher | View at Google Scholar - Fajrin, I., Alam, G., & Usman, A. N. (2020). Prostaglandin diploma for fundamental dysmenorrhea ache patients. Enfermería Clínica, 30, 5–9. https://doi.org/10.1016/j.enfcli.2019.07.016
View at Publisher | View at Google Scholar - Smith, R. P. (2018). The characteristic of prostaglandins in dysmenorrhea and menorrhagia. In Dysmenorrhea and Menorrhagia (pp. 75–88),. Boca Raton: Springer.
View at Publisher | View at Google Scholar - Najimudeen, M., Myint, M. H., & Masharudin, A. W. (2020). Reappraisal of the management of essential dysmenorrhoea in minors. College Students Global Journal of Obstetrics and Gynecology, three, 192–199. https://doi.org/10.36348/sijog.2020.v03i09.001
View at Publisher | View at Google Scholar - Al-Jefout, M., & Nawaiseh, N. (2016). non-stop norethisterone acetate in opposition to repetitive drospirenone 3 mg/ethinyl estradiol 20 μg for the administration of primary dysmenorrhea in youngster better halves. magazine of pediatric and adolescent gynecology, 29, 1437. https://doi.org/10.1016/j.jpag.2015.08.009
View at Publisher | View at Google Scholar - Speroff, L., & Fritz, M. A. (2005). Scientific gynecologic endocrinology and unproductiveness (seventh ed.). Lippincott Williams & Wilkins.
View at Publisher | View at Google Scholar - Ibrahim, N. ok., Al-Sharabi, B. M., Al-Asiri, R. A., Alotaibi, N. A., Al-Husaini, W. I., Al-Khajah, H. A., Rakkah, R. M., & Turkistani, A. M. (2015). Dysmenorrhea with female healing students at King Abdulaziz College: prevalence, predictors, and effect. Pakistan Mag of Medical Sciences, 31, 1312. https://doi.org/10.12669/pjms.316.8752
View at Publisher | View at Google Scholar - Rafique, N., & Al-Sheikh, M. H. (2018). incidence of menstrual questions and their union accompanying cognitive pressure in more youthful woman juniors gaining knowledge of properly-being sciences. Saudi clinical mag, 39, 67. https://doi.org/10.15537/smj.2018.1.21438
View at Publisher | View at Google Scholar - Abd El-Mawgod, M. M., Alshaibany, A. S., & Al-Anazi, A. M. (2016). Epidemiology of dysmenorrhea with subordinate college juniors in Northern Saudi Arabia. Journal of the Egypt Public Fitness Association, 91, 115–119. https://doi.org/10.1097/01.EPX.0000489884.20641.90 5
View at Publisher | View at Google Scholar - Saleem, M. A. (2018). Dysmenorrhea, blended manifestations, and control among graduates at King Khalid University, Saudi Arabia: A preliminary observation. journal of the circle of relatives remedy and primary care, 7, 769. https://doi.org/10.4103/jfmpc.jfmpc_113_18
View at Publisher | View at Google Scholar - Haşim, R. T., Alkhalifah, S. S., Alsalman, A. A., Alfaris, D. M., Al-Hussaini, M. A., Qasim, R. S., & Shaik, S. A. (2020). occurrence of fundamental dysmenorrhea and appeal effect at the situation of history amongst female recuperation pupils at King Saud University, Riyadh, Saudi Arabia. Saudi Scientific Magazine, 41, 283–289. https://doi.org/10.15537/smj.2020.3.24988
View at Publisher | View at Google Scholar - Ju, H., Jones, M., & Mishra, G. (2014). The prevalence and hazard determinants of dysmenorrhea. Epidemiologic opinions, 36, 104. https://doi.org/10.1093/epirev/mxt009
View at Publisher | View at Google Scholar - Burnett, M., & Lemyre, M. (2017). No. 345-number one dysmenorrhea consensus guiding principle. mag of Obstetrics and Gynecology Canada, 39, 585–595. https://doi.org/10.1016/j.jogc.2016.12.023
View at Publisher | View at Google Scholar - Andersch, B., & Milsom, I. (1982). An epidemiologic study of younger daughters accompanying dysmenorrhea. American Journal of Obstetrics and Gynecology, 144, 655–660. https://doi.org/10.1016/0002-9378(eighty two)90433-1
View at Publisher | View at Google Scholar - Campbell, M. A., & McGrath, P. J. (1997). Use of drugs by children for the management of menstrual soreness. Facts of Pediatrics & Adolescent Remedy, 151, 905–913. https://doi.org/10.1001/archpedi.1997.02170460043007
View at Publisher | View at Google Scholar - Hailemeskel, S., Demissie, A., & Assefa, N. (2016). primary dysmenorrhea duration, risk determinants, and allure effect on educational performance: evidence from female academy students in Ethiopia. global magazine of girls' health, 8, 489–496. https://doi.org/10.2147/IJWH.S112768
View at Publisher | View at Google Scholar - Subasinghe, A. Okay., Happo, L., Jayasinghe, Y. L., Garland, S. M., Gorelik, A., & Wark, J. D. (2016). The occurrence and severity of dysmenorrhoea and management alternatives were discussed with young Australian mothers. Australian family physician, 45, 829–834.
View at Publisher | View at Google Scholar - Habibi, N., Huang, M. S. L., Gan, W. Y., Zulida, R., & Safavi, S. M. (2015). incidence of primary dysmenorrhea and determinants guide charm pressure with senior students: A circulate-divided check. Pain Management Nursing, sixteen, 855–861. https://doi.org/10.1016/j.pmn.2015.07.001
View at Publisher | View at Google Scholar - Ortiz, M. I. (2010). Number one dysmenorrhea among Mexican academy juniors: incidence, effect, and scenario. eu magazine of Obstetrics & Gynecology and Reproductive Biology, 152, 73–77 https://doi.org/10.1016/j.ejogrb.2010.04.0.5
View at Publisher | View at Google Scholar - Bajalan, Z., Alimoradi, Z., & Moafi, F. (2019). nutrients as a potential determinant of basic dysmenorrhea: an orderly evaluation of realistic research. Gynecologic and Obstetric Investigation, 84, 209–224. https://doi.org/10.1159/000495408
View at Publisher | View at Google Scholar - Al-Jefout, M., Seham, A. F., Jameel, H., Randa, A. Q., & Luscombe, G. (2015). Dysmenorrhea: prevalence and circumstances of lifestyles with teen Jordanian girls. magazine of pediatric and adolescent gynecology, 28, 173–185. https://doi.org/10.1016/j.jpag.2014.07.zero.five
View at Publisher | View at Google Scholar - Hailemeskel, S., Demissie, A., & Assefa, N. (2016). primary dysmenorrhea importance, befriended hazard determinants, and charm impact on the academic act: evidence from girl academy graduates in Ethiopia. international magazine of women's fitness, eight, 489–496. https://doi.org/10.2147/IJWH.S112768
View at Publisher | View at Google Scholar - Ameade, E. P., Amalba, A., & Mohammed, B. S. (2018). Incidence of dysmenorrhea amongst academy juniors in Northern Ghana; enchantment impact and control planning. BMC Women's Fitness, 18, 1–nine. https://doi.org/10.1186/s12905-018-0532-1
View at Publisher | View at Google Scholar - Al-Matouq, S., Al-Mutairi, H., Al-Mutairi, O., Abdulaziz, F., Al-Basri, D., Al-Enzi, M., & Al-Taiar, A. (2019). Dysmenorrhea among extreme-faculty graduates and attraction are combined determinants in Kuwait. BMC Pediatrics, 19, eighty. https://doi.org/10.1186/s12887-019-1442-6
View at Publisher | View at Google Scholar - Tomás-Rodríguez, M. I., Palazon-Bru, A., Martínez-St John, D. R., Navarro-Cremades, F., Toledo-Marhuenda, J. V., & Gil-Guillén, V. F. (2017). factors manually raised ache in number one dysmenorrhea: analysis making use of a multivariate orderly logistic regression model. Magazine of Pediatric and Adolescent Gynecology, 30, 199–202. https://doi.org/10.1016/j.jpag.2016.09.007
View at Publisher | View at Google Scholar - Laganà, A. S., l. a. Rosa, V. L., Rapisarda, A. M., Valenti, G., Sapia, F., Chiofalo, B., Rossetti, D., Frangež, H. B., Bokal, E. V., & Vitale, S. G. (2017). tension and concavity in sufferers accompanying endometriosis: effect and management disturbing situations. global magazine of women's health, nine, 323.
View at Publisher | View at Google Scholar - Sansone, A., De Rosa, N., Giampaolino, P., Guida, M., Laganà, A. S., & Di Carlo, C. (2018). effects of etonogestrel insert on the person of records, sex feature, and pelvic ache in women suffering from endometriosis: consequences from a multicenter, predicted, sensible look at. data of Gynecology and Obstetrics, 298, 731–736.
View at Publisher | View at Google Scholar - Brasil, D. L., Montagna, E., Trevisan, C. M., l. a. Rosa, V. L., Lagana, A. S., Barbosa, C. P., & Bianco, B. (2019). intellectual pressure ranges in moms accompanying endometriosis: systematic assessment and meta-check of sensible research. Minerva Medica, 111, 90–102.
View at Publisher | View at Google Scholar - Aksu, H., & Özsoy, S. (2016). Primary dysmenorrhea and herbals, magazine of health communication, 1, 23.
View at Publisher | View at Google Scholar - Savitha, V., Roopa, D., & Sridhara, Okay. M. (2016). take a look at to determine the impact of an organized schooling program on facts regarding home remedies on reducing dysmenorrhea among adolescent ladies at St. Paul’s Ladies Immoderate College. Davangere, Asian magazine of nursing schooling and studies, 6, 327–330. https://doi.org/10.5958/2349-2996.2016.00061.6
View at Publisher | View at Google Scholar - Dawood, M. Y. (2006). Primary dysmenorrhea: advances in pathogenesis and administration. Obstetrics and Gynecology, 108(2), 428–441. Link
View at Publisher | View at Google Scholar - Iacovides, S., Avidon, I., & Baker, F. C. (2015). What we hear about basic dysmenorrhea contemporary: A fault-finding review. Human Reproduction Update, 21(6), 762–778. Link
View at Publisher | View at Google Scholar - Habibi, N., Huang, M. S. L., Gan, W. Y., Zulida, R., & Safavi, S. M. (2015). Prevalence of basic dysmenorrhea and allure cause with academy juniors: A cross-localized study. Pain Management Nursing, 16(6), 855–861. Link
View at Publisher | View at Google Scholar - Osayande, A. S., & Mehulic, S. (2014). Diagnosis and beginning administration of dysmenorrhea. American Family Physician, 89(5), 341–346. Link
View at Publisher | View at Google Scholar - Burnett, M. A., & Lemyre, M. (2017). No. 345: Primary Dysmenorrhea Consensus Guideline. Journal of Obstetrics and Gynecology Canada, 39 (7), 585–595. Link
View at Publisher | View at Google Scholar - Harel, Z. (2006). Dysmenorrhea in teenagers and young women: An update on pharmacological situations and administration methods. Expert Opinion on Pharmacotherapy, 7(4), 503–510. Link
View at Publisher | View at Google Scholar - Patel, V., Tanksale, V., Sahasrabhojanee, M., Gupte, S., & Nevrekar, P. (2006). The burden and cause of dysmenorrhoea: A culture-located survey of 2262 wives in Goa, India. BJOG: An International Journal of Obstetrics & Gynecology, 113(4), 453–463. Link
View at Publisher | View at Google Scholar - Campbell, M. A., & McGrath, P. J. (1999). Use of drugs by youngsters for the administration of menstrual discomfort. Archives of Pediatrics & Adolescent Medicine, 153(5), 508–513. Link
View at Publisher | View at Google Scholar - Proctor, M. L., & Murphy, P. A. (2001). Herbal and digestive analyses for basic and subordinate dysmenorrhoea. Cochrane Database of Systematic Reviews, (2), CD002124. Link
View at Publisher | View at Google Scholar - French, L. (2005). Dysmenorrhea. American Family Physician, 71(2), 285–291. Link
View at Publisher | View at Google Scholar - Parazzini, F., Tozzi, L., Mezzopane, R., Luchini, L., & Marchini, M. (1994). The severity of dysmenorrhea and the allure connection accompanying the period. Obstetrics and Gynecology, 84(2), 248–251. Link
View at Publisher | View at Google Scholar - Westling, A. M., Tu, F. F., & Griffith, J. W. (2013). The association of dysmenorrhea with noncyclic pelvic pain gives reason for mental determinants. American Journal of Obstetrics and Gynecology, 209(5), 422.e1–422.e10. Link
View at Publisher | View at Google Scholar - Dawood, M. Y. (1990). Nonsteroidal antagonistic-instigative drugs and changeful stances toward dysmenorrhea. The American Journal of Medicine, 88(5A), 14S–18S. Link
View at Publisher | View at Google Scholar - Abaraogu, U. O., Tabansi-Ochuogu, C. S., & Igwe, S. E. (2017). Effectiveness of a yoga program in the administration of dysmenorrhea: An orderly review. Evidence-Based Complementary and Alternative Medicine, 2017, 1–9. Link
View at Publisher | View at Google Scholar - Grandi, G., Ferrari, S., Xholli, A., Cannoletta, M., Palma, F., Romani, C., & Volpe, A. (2012). Prevalence of menstrual pain in young wives: What is dysmenorrhea? Journal of Pain Research, 5, 169–174. Link
View at Publisher | View at Google Scholar - Marjoribanks, J., Ayeleke, R. O., Farquhar, C., & Proctor, M. (2015). Nonsteroidal antagonistic-instigative drugs for dysmenorrhoea. Cochrane Database of Systematic Reviews, (7), CD001751.
View at Publisher | View at Google Scholar - Armour, M., Smith, C. A., & Steel, K. A. (2019). Acupuncture for dysmenorrhoea. Cochrane Database of Systematic Reviews, (5), CD007854.
View at Publisher | View at Google Scholar - Zhu, X., Liew, Y., Liu, Z. L., & Liu, J. (2016). Herbal cure for basic dysmenorrhoea. Cochrane Database of Systematic Reviews, (3), CD005288.
View at Publisher | View at Google Scholar - Zhu, X., Proctor, M., Bensoussan, A., Smith, C. A., Wu, E., & Smith, T. (2018). Chinese herbaceous cure for basic dysmenorrhoea. Cochrane Database of Systematic Reviews, (5), CD005288.
View at Publisher | View at Google Scholar - Zhu, X., Proctor, M., Bensoussan, A., Wu, E., Smith, C. A., & Smith, T. (2017). Chinese herbaceous cure for basic dysmenorrhoea. Cochrane Database of Systematic Reviews, (8), CD005288.
View at Publisher | View at Google Scholar - Proctor, M., Farquhar, C., Stones, R. W., & He, L. (2001). Transcutaneous energetic nerve provocation for basic dysmenorrhoea. Cochrane Database of Systematic Reviews, (4), CD002123.
View at Publisher | View at Google Scholar

 Clinic
Clinic
