Research Article | DOI: https://doi.org/10.31579/2834-5142/102
Managing Chronic Kidney Disease among Elderly in Primary Care Settings!
- K. Suresh *
Family Physician & Public Health Consultant, Bengaluru, 560022,
*Corresponding Author: K. Suresh, Family Physician & Public Health Consultant, Bengaluru, 560022.
Citation: María B. Paillalef, Jennifer Nichols, Miguel Fontenla, Maximiliano H. Ramirez, (2025), Managing Chronic Kidney Disease among Elderly in Primary Care Settings!. I Journal of Clinical Nephrology. 4(2); DOI:10.31579/2834-5142/102
Copyright: © 2025, María B. Paillalef. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 14 March 2025 | Accepted: 21 March 2025 | Published: 28 March 2025
Keywords: Manage Hypertension, Diabetes, Chronic Kidney disease Heart diseases, Obesity & Medications in Aged Patients
Abstract
Kidney function naturally declines with age, in addition diabetes, hypertension, heart diseases, and chronic kidney disease exacerbated by Obesity, smoking, and certain medications are the main causes of chronic kidney disease (CKD). include can exacerbate these conditions. Primary care physicians can handle this public health problem of CKD, as the great majority of patients, of those up to stable stage 3, can be managed in primary care setting. Dialysis is the first option when chronic kidney disease progresses to Stage 5, or end-stage renal disease (ESRD), when kidneys fail to filter blood effectively, needing dialysis or a kidney transplant to survive.
In India, the prevalence of chronic kidney disease (CKD) in the general population is around 14.3%, with higher rates of 36.1% in high-risk populations like those with diabetes or hypertension and elderly. Research suggests a higher CKD prevalence in the elderly (≥65 years) 40.6% versus 23.3% in middle-aged adults (45-64 years).
This article attempts to update the general physicians or Primary health care providers about the latest national and international guidelines of managing CKD in elderly.
Materials and Methods:
This article is an outcome of managing dozens of cases of CKD as primary health care provider and working with Nephrologists both in public and private sectors, with giving examples of four cases in the recent past and following up case after tertiary care, quoting about four cases in elderly, complimented by literature search about the latest national & international guidelines.
Introduction
Kidney function naturally declines with age, making older adults more susceptible to kidney disease. While High blood sugar levels over time damage the small blood vessels and filters in the kidneys, leading to diabetic nephropathy, uncontrolled Hypertension puts a strain on the blood vessels in the kidneys, reducing their ability to filter waste effectively [1]. Heart Diseases reduce blood flow to the kidneys, leading to acute kidney injury or worsening CKD. Chronic Kidney Disease (CKD), a progressive condition in which the kidneys gradually lose their ability to filter waste and excess fluid from the blood. Obesity contributes to both diabetes & hypertension and indirectly increases the risk of kidney disease. Smoking damages blood vessels, worsening existing kidney problems. Commonly prescribed medications include antibiotics, diuretics, NSAIDs for pain relief, laxatives for constipation (particularly among the elderly), dietary supplements, statins, antimicrobials, antiviral drugs (such as those for COVID-19 and shingles), vancomycin, and radiocontrast agents do harm to the kidneys. The family history of kidney disease increases the risk of developing the condition. While there is not a direct correlation between religion and kidney disease risk in India, socioeconomic groups, particularly Scheduled Castes and Scheduled Tribes (SC/ST), have a higher prevalence of CKD. This may be due to factors like higher rates of diabetes and hypertension in these communities, as well as socioeconomic disparities affecting access to healthcare and healthy lifestyles [4]. In elderly individuals, thirst sensation often diminishes due to various physiological changes associated with aging, potentially leading to dehydration. This reduced thirst response, coupled with decreased kidney function and cognitive decline, can make older adults more susceptible to dehydration. Sweating increases with hot weather, physical activities, and sports, potentially causing kidney injury. “By the time an older adult feels thirsty, that's already an indication of early dehydration,” [2].
In India, the prevalence of chronic kidney disease (CKD) in the general population is around 14.3%, with higher rates of 36.1% in high-risk populations like those with diabetes or HTN. Research also suggests a higher CKD prevalence of 40.6% in the elderly (≥65 years) versus 23.3% in middle-aged adults (45-64 years) [3,5].
CKD among the elderly primarily results from diabetes, hypertension, and cardiovascular diseases, which progressively impair kidney function. Other factors contributing to kidney problems in the elderly include certain medications, dehydration, urinary tract infections, and kidney stones. Primary care physicians can handle majority of patients, at least up to stable stage 3, in primary care setting [5,6].
This article is an outcome of managing dozens of cases of CKD, quoting about four cases in elderly, to update the general physicians or Primary health care providers about the latest national and international guidelines of managing CKD in elderly.
Case Reports:
Case 1 Hypertension, Osteo Arthritis & CKD: Shreedhar, a male aged 74 years, known hypertensive for a decade on anti-hypertensives complained Pedal swelling in September 2023. Used to consume alcohol 5-6 times a month. He has been suffering Osteoarthritis of both knees for the last 10 years & used to pop-in NSAIDs frequently for pain relief.
A Nephrologists consultation led to Physical examination that showed pedal pitting edema, BP=210/140 mm hg, Pulse 198/min & recommending KFT, LFT & other biomarkers, Abdomen & Pelvis scans.

The reports read: i) HbA1c=5%, ii) estimated average glucose= 97mg/dl, iii) FBS= 86mg/dl, iv) Serum Creatinine= 2 mg /dl (0.7-1.3) v) Total Cholesterol 175 mg/dl, vi) Triglycerides 134 mg/dl, vii) HDL 39 mg/dl (40-60), viii)LDL-105 mg/Dl (<100 Urea=20 xss=removed>
Case 2. Liver disease, GI disease, CKD, ending in Uremic Encephalopathy:
Mr. S Murthy, aged 67 years, consulted a physician in Belagavi, Karnataka, on 12 February 2024 with complaints of abdominal discomfort, difficulty in micturition and swelling of feet and poor appetite. A general examination revealed a pallor, BP= 156/102 mm hg, slight tenderness in Rt. upper quadrant of abdomen. Investigations i) A CBC showed 10.5% Hb, Iron deficiency anemia ii) Blood urea (24 mg/dl) & Creatinine (1.0 mg/dl), all were in normal ranges. A prostate-specific antigen (PSA) test and Liver & Kidney function biomarkers tests wer also in normal ranges. He was prescribed Dytor 20 mg (a diuretic) half tablet BD, Tab Envas 2.5 mg (antihypertensive), Tab. Urimax 0.4 mg once day for BPH one tab every night and Tab Detox (for indigestion) after lunch /day.
But for reduction in pedal oedema, no improvements were seen in next 2 Months. In April 2024, in a follow up visit the clinical examination revealed BP under control (132/89 mm Hg). Abdomen and Pelvic Scanning showed i) Liver normal size with coarse eco-structure and surface nodularity ii) Gall bladder distended with a few Calculi largest measuring about 3.6 mm in diameter with No GB wall thickening and pericholecystic oedema iii) Urinary bladder moderately distended and mild thickening of the wall measuring 5.2 mm with internal echoes & 2-3 tandem calculi largest measuring 6.9 x 3.5mm. iv) Pre-voiding urine volume was 246 ml and post-voiding residual urine of 126 ml. v) Prostate was enlarged measuring 4.4x3.8x4.6 cm and a volume of 41.5cc. vi) Blood PSA level was raised to 0.54 (<0>
Since mid-May 2024, he noticed bloating abdomen and swelling of the feet. As the abdominal distension was discomforting, he consulted a local Physician on 26 June 2024 and Liver function tests were repeated. This time LFT showed abnormal biomarkers (normal range in parenthesis) – i) Serum Creatinine-2.0 (0.6-1.6), Na-122 (136-145) and Chorides-92 (97-111), Serum Bilirubin-3.4 mg/dl (0-1.3), Direct Bilirubin -0.8 mg/dl (0.0-0.3) Indirect Bilirubin -2.6 mg (0.2-1.0), Alkaline Phosphate-145 u/l (41-137) & Gamma GT GGT)-51 u/ l (0-50) a first indication of Liver dysfunction. He was put on a dozen drugs for liver, kidney, prostate maladies. Repeat Biomarker tests on 21 July 2024 showed a bit improvement in i) Creatintine-1.5, Na-124. However, the abdominal distension had increased discomforting him, therefore, about 1.5 Liter of abdominal fluid was tapped, providing a temporary relief but soon the abdomen started bulging again. In September 2024 he started complaining of sever fatigue & inability to walk. On 7 September 2024, he suddenly became disoriented, confused, unable to swallow fluids and urinary retention. The local physician referred him to & he was admitted to an ICU of a private Medical College Hospital. On admission his BP recorded 86/54 mm Hg. At the MCH the biomarkers read Blood Urea 118 mg/dl (10-45), Serum Creatinine-5.4 mg/dl (0.7-1.5), Sodium-134 mmol/l (135-155), Potassium -5.8 mmol/L (3.5-5.5), Chlorides-112 mmol /L (98-107).
All LFT biomarkers were off the mark too e.g., T Bilirubin-3.1 mg/dl, (0-1.2) D Bilirubin-0.4 (0-0.3), IBilirubin-2.7mg/dl (0-1.5), Total Protein -5.6 gm /dl (6.0-8.3), Albumin-1.9 gm/dl, (3.4-4.5) were reduced, and Globulin 3.7 gm/dl (2.0-3.5) was raised, SGOT-239 u/L (0-46), SGPT-91 U/L (0-49) were more than double, Hb%-8.6 g/l had come down further. The Albumin level in Peritoneal fluid was 2.1 gm/dl. With SAAG working out to be 1.9/2.1= 0.905, a diagnosis of Hepatorenal failure consequent to AKI, was made and led to Hypovolemic shock, and anuria, and the patient died on the early morning of 8th September 2024. It was concluded that the patient went into Uremic encephalopathy, a cerebral dysfunction caused by the accumulation of toxins due to chronic renal failure, as estimated glomerular filtration rate was below 05 mL/min.
Case Report 3: Hidden Diabetes and Diabetic Nephropathy
A 65-year-old Hanumappa of rural background presented with pedal edema, hypertensive for 5 years, on standard therapy to my clinic. Basic investigation revealed proteinuria and hypoalbuminemia with normal fasting blood sugar levels. However, a consultation in Nephrology hospital followed by a renal biopsy revealed diabetic nephropathy changes. Later a continuous glucose monitoring system (CGMS) for 2 weeks revealed that his daily blood glucose levels met the criteria for diabetes. This case demonstrates that some individuals with diabetic nephropathy may have "hidden" diabetes or impaired glucose tolerance, highlighting the importance of investigating potential diabetes even in the absence of a formal diagnosis. He has been put on SGLT2is dapagliflozin to reduce the risk of heart attack, stroke, or cardiovascular events.
Case Report 4: Diabetic Nephropathy and CKD Progression
A 50-year-old female patient with a 15-year history of type 2 diabetes and non-proliferative diabetic retinopathy approached with complaints of pedal edema. Diagnostic tests revealed elevated blood sugar, creatinine, and signs of kidney damage, that led to a diagnosis of progressive chronic kidney disease due to diabetic nephropathy. This case highlights the typical presentation of diabetic nephropathy and the need for comprehensive management, including insulin, medications to protect the kidneys, and lifestyle changes.
She is being managed using a combination of sodium-glucose co-transporter 2 inhibitors (SGLT2is) dapagliflozin and glucagon-like peptide-1 receptor agonists (GLP1-RAs) Semaglutide
Discussions:
Globally Older people are more at risk of some kidney & urinary tract diseases like i) inflammation or swelling of the kidneys – called glomerulonephritis ii) diabetes damages blood vessels & nerves, even if the diabetes is well managed iii) urinary tract infections, left untreated, spread into the kidneys and cause lasting damage. Urinary tract infections are very common, particularly in women and with increasing age iv) Urinary incontinence, a condition of uncontrolled leaking of urine from the bladder, increases the risk of urinary tract infections, an enlarged prostate in men may cause incontinence. Renovascular disease like fatty deposits, cholesterol, calcium and other substances are deposited in the inner lining of the arteries, causing narrowing or blockage of the renal artery, affecting the kidneys’ filters and reducing the blood supply to the kidneys, resulting in Hypertension and reduced kidney function, a most common cause of kidney failure in the elderly. high blood pressure if left untreated, or not well monitored and maintained increase the risk of heart attack, stroke and loss of vision, and cause kidney damage. Hereditary kidney diseases like polycystic kidney disease are uncommon causes.
Chronic inflammation often starts when our body's natural response to a problem, like an infection or injury, doesn't shut off as it should. It can develop in several ways. One possibility is that the problem remains because the body can't rid itself of the offending substance, be it an infectious organism, an irritant, or a chemical toxin. The immune system is pretty good at eliminating invaders, but sometimes pathogens resist even our best defenses and hide out in tissues, provoking the inflammatory response again and again. This leads to Renal Insult and failure over time as happened in our second case.
The signs of chronic inflammation are not as obvious as those of acute inflammation. No sharp twinge of pain, no swelling or redness to alert about a problem. Chronic inflammation can be widespread or more localized to specific areas of the body. Some of the symptoms associated with chronic inflammation include: fatigue and lack of energy, depression, anxiety, muscle aches and joint pain as was observed in our first case, or constipation, diarrhea, other gastrointestinal complaints, abdominal distension due to peritoneal fluids because of liver damage, changes in weight or appetite, headaches and a "fuzzy" mental state as was seen in our second case.
Chronic kidney disease:
CKD is defined as evidence of kidney disease with/without decrease in GFR < 60>3 months), Markers of kidney damage (one or more) [5]
- Albuminuria, Albumin excretion rate (AER) >30 mg/24 hours; ACR >30 mg/g of creatinine
- Urine sediment abnormalities Electrolyte and other abnormalities due to tubular disorders Abnormalities detected by histology
- Structural abnormalities detected by imaging
- History of kidney transplantation
| category GFR (ml/min/1.73 m2) | Terms |
G1 | >90 | High or normal |
G2 | 60-89 | Mild decrease |
G3a | 59-45 | Mild to moderate decrease |
G3b | 44-30 | Moderate to severe |
G4 | 29-15 | Severe decrease |
G5 | <15> | Kidney failure |
Table 1: GFR - glomerular filtration rate [5].
Albuminuria category in CKD - Based on degree of proteinuria, there are three stages of albuminuria, category as shown below [5]:
Category | AER (mg/24 hrs) | ACR (mg/gm) | Terms |
A1 | <30> | <30> | Normal or mild increase |
A2 | 30-300 | 30-300 | Moderate increase |
A3 | >300 | >300 | Severe increase |
Table 2: AER- albumin excretion rate, ACR- albumin-to-creatinine ratio
Dialysis is the first option when chronic kidney disease progresses to Stage 5, or end-stage renal disease (ESRD), where kidneys fail to filter blood effectively. In this stage, dialysis or a kidney transplant is necessary to survive [5].
Management od’s CKD in India:
“kidney disease” is manifested by evidence of urinary Proteinuria and hematuria and/or radiological abnormality and/or decrease in kidney function as assessed by increase in serum creatinine corresponding to decrease in Glomerular Filtration Rate, GFR). These are the diseases where there is either evidence of kidney damage and/or evidence of low glomerular filtration rate below < 60>
Lifestyle Modifications:
i) Maintaining a healthy weight ii) Regular exercise, even starting with short walks, iii) Quitting tobacco use for slowing down CKD progression and iv) Finding healthy ways like meditation, Yoga and participation social service etc. to manage stress.
Dietary Changes include i) Reducing salt intake to less than 5g per day ii) Controlling protein intake, with a low- animal protein diet for advanced CKD.
Blood Pressure Control:
Regular blood pressure monitoring at home with digital BP apparatus in supine, sitting and standing positions at least twice a week, prescribe and moderating the doses of the drugs ACE inhibitors, ARBs, along with diuretics, based on kidney function.
Glycemic Control: For diabetic patients, maintaining blood sugar levels within the target range.
Medication Management:
Avoidance of NSAIDs, among people with arthritis or Rheumatoid arthritis which are harmful to the kidneys. Primary prevention strategies (PPS): PPS such as promoting healthy lifestyles and early screening for risk factors, are crucial for preventing the development of CKD.
Using a combination of SGLT2is and GLP1-RAs provides additional protection against kidney Heart Dise
A recent study published in The Lancet Diabetes & Endocrinology suggested that using a combination of sodium-glucose co-transporter 2 inhibitors (SGLT2is) and glucagon-like peptide-1 receptor agonists (GLP1-RAs) provide additional protection against kidney and heart disease in patients with diabetes. SGLT2is, or gliflozins, helps lower blood glucose levels by promoting its excretion through urine. On the other hand, GLP-1RAs, such as Ozempic, enhance insulin release and sensitivity. The new findings are based on a meta-analysis of 12 large-scale involving 73,238 diabetic patients, 3,065 of whom were already receiving GLP1-RAs. The results indicated that SGLT2is reduced the risk of heart attack, stroke, or cardiovascular death by 11%, independent of GLP1-RAs. It also reduced the risk of chronic kidney disease progression by 33% when combined with GLP1-RAs and slowed the annual loss of kidney function by nearly 60% [6].
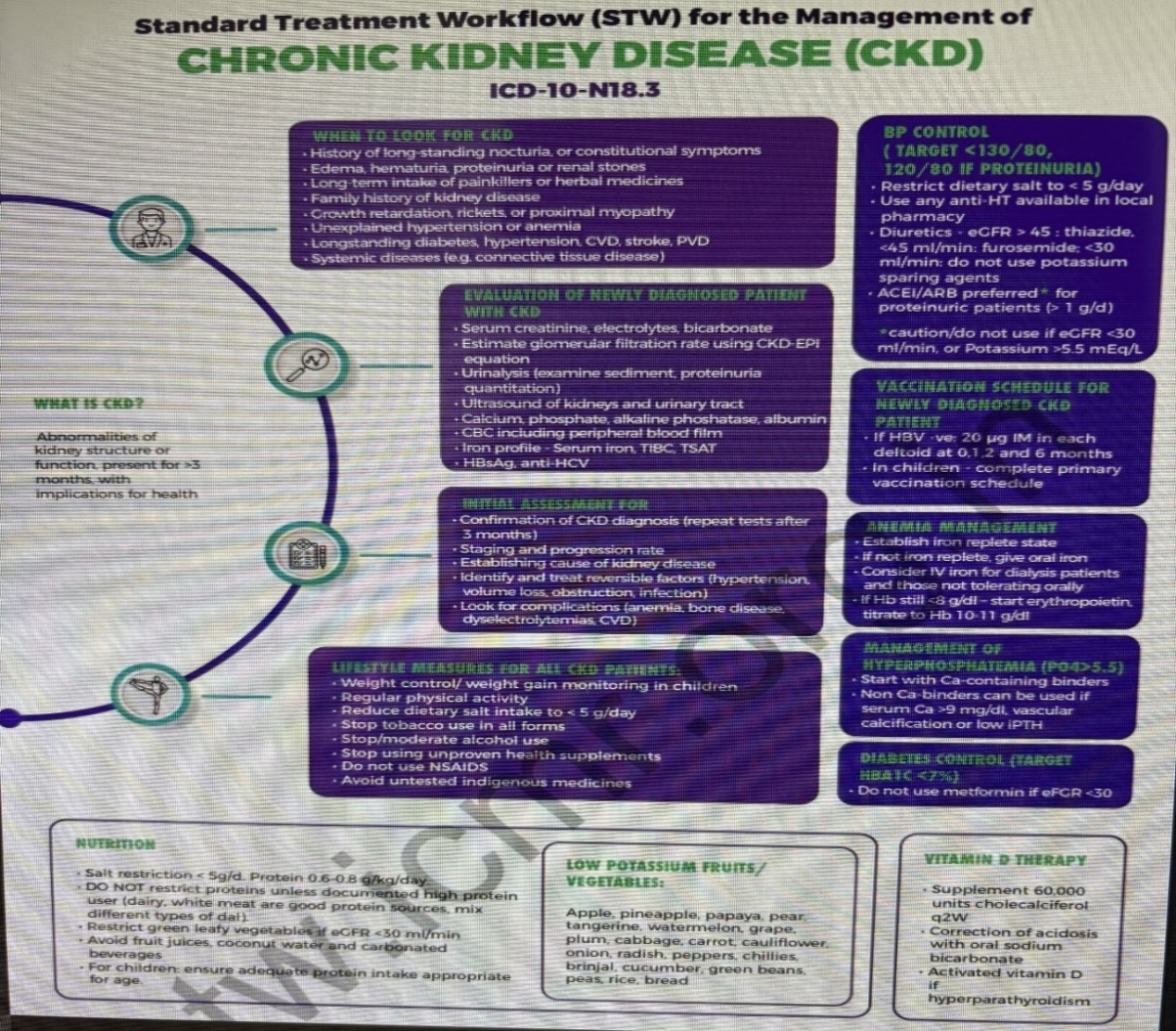
Source: ICMR (4)
Monitoring and Follow-up:
Regular monitoring of kidney function, including GFR (glomerular filtration rate) and albuminuria, is necessary. Managing cardiovascular risk factors, such as high blood pressure, diabetes, and high cholesterol, play an important role. Of late Statins are being prescribed for cardiovascular risk reduction in CKD patients
Patient Education and Support:
Educating patients and their families about CKD, its management, and potential complications facilitates successful outcomes.
Prevention:
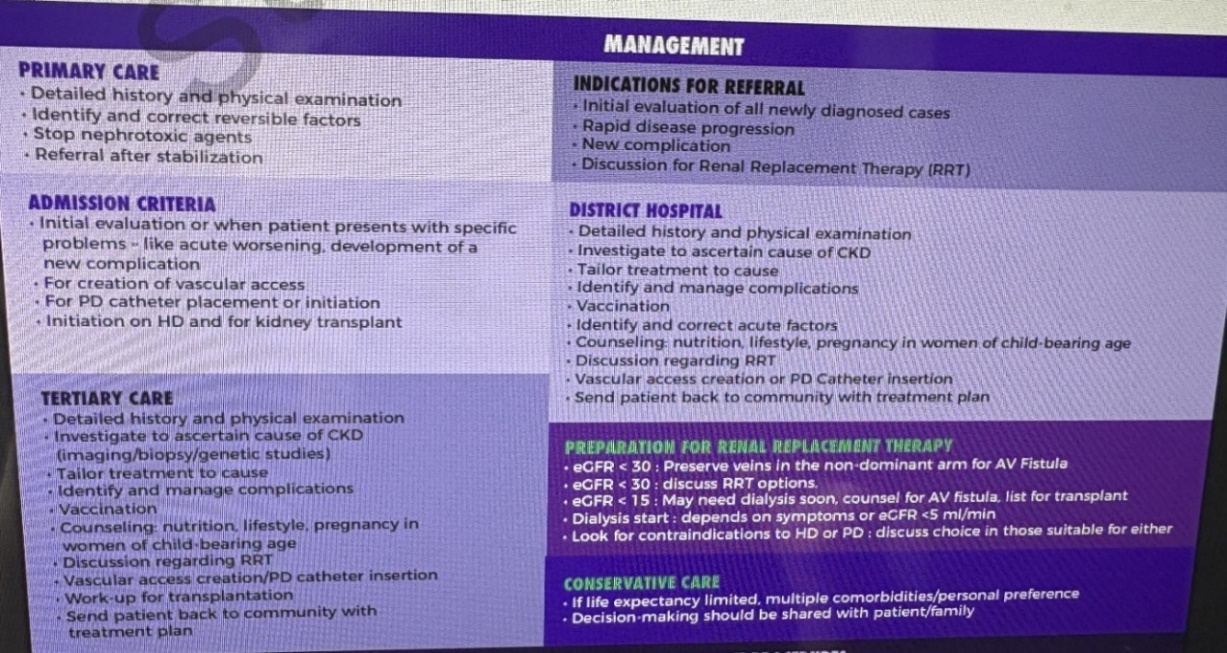
Primary care physicians can handle the public health problem of CKD, as the great majority of CKD patients, particularly those up to stable stage 3 can be managed in primary care setting with guidance from Physician and nephrologists at higher center if required. PHC provider has the following responsibilities in prevention and management of CKD.
A. Early Detection of CKD, B. Reduce the risk of progression, C. Detecting the risk factors of other/Concomitant NCDs, D. Early detection, follow-up and management of CKD associated complications, E. Referral for consultation at higher center, F. Counseling for Renal Replacement Therapy (RRT) for ESKD
References
- Kidneys - age-related problems,
View at Publisher | View at Google Scholar - The Connection Between Age & Dehydration, May 2023
View at Publisher | View at Google Scholar - How acute inflammation turns chronic,
View at Publisher | View at Google Scholar - Stevens, Paul E. et al. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease, Kidney International, Volume 105, Issue 4, S117 - S314.
View at Publisher | View at Google Scholar - Standard Treatment Workflow, for the management of chronic kidney disease (CKD)
View at Publisher | View at Google Scholar - Medical Officers' Manual for Prevention & Management, 21 Nov 2022
View at Publisher | View at Google Scholar - Combined Diabetes Drugs Offer Enhanced Heart & Kidney Protection, 04 May 2025
View at Publisher | View at Google Scholar

 Clinic
Clinic
