case report | DOI: https://doi.org/10.31579/2834-5126/004
Malignant Transformation of Intracranial Epidermoid Cyst Tumor to Squamous Cell Carcinoma, Case Report and Literature Review
1Professor of Neurosurgery, Department of Neurosurgery, Mashhad University of Medical Sciences,Mashhad,Iran.
2Resident Physician in Adult Neurology University of Toronto, Toronto, ON.
3Resident of Neurosurgery, Department of Neurosurgery, Mashhad University of Medical Sciences, Mashhad, Iran.
*Corresponding Author: Mohammad Faraji-Rad, Professor of Neurosurgery, Department of Neurosurgery, Mashhad University of Medical Sciences, Mashhad, Iran.
Citation: Mohammad Faraji-Rad, Elnaz Faraji-Rad and Saman Mohazzab-Torabi, (2022) Malignant Transformation of Intracranial Epidermoid Cyst Tumor to Squamous Cell Carcinoma, Case Report. International J. clinical and Medical Case Reports, 1(1); Doi:10.31579/2834-5126/004
Copyright: © 2022 Mohammad Faraji-Rad, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 09 September 2022 | Accepted: 13 September 2022 | Published: 21 September 2022
Keywords: Malignant Transformation; Intracranial Epidermoid; Cyst Tumor; Squamous Cell Carcinoma
Abstract
Intracranial epidermoid cysts (ECs) are rare, benign tumor of central nervous system that appear from maintain ectodermal implants. Malignant transformation of an EC to squamous-cell carcinoma (SCC) is rarely reported. We present the case of a 43-years old male presenting with left hemianopia and severe headache 6 months after total resection of an epidermoid cyst of right frontal, whose pathological report disclose to be a malignant transformation of previous epidermoid tumor. Optimal total resection in addition adjuvant radiotherapy is the management of choice, although the patient’s general survival of this condition is poor.
Introduction
Intracranial epidermoid cysts comprising for approximately 0.2-1% of brain tumors.[1] They originally develop from aberrant ectodermal embryonic tissue in the neural groove at 4 or 5 weeks of fetal development.[2] Intracranial epidermoid cysts are benign and slow-growing tumors. early presenting symptoms depending on the sites of the tumor. Epidermoid cysts are commonly known to be benign and totally curable by surgery. [3] Malignant transformation of an epidermoid cyst to squamous cell carcinoma (SCC) is very rare in literature. [4] The most prevalent location of occurrence of carcinoma are in cerebellopontine angle (CPA) and in para-pituitary area. [5] As hamlet mentioned, primary squamous cell carcinoma (PSCC) was categorized into five groups: 1) primary malignant transformation of a benign cyst, 2) malignant transformation from a remnant cyst, 3) malignant transformation of a dermoid and epithelial cyst, 4) malignant transformation with leptomeningeal carcinomatosis, and 5) other malignancies arising from benign cysts. [6] We will describe a case of malignant transformation of epidermoid cyst origination as large suprasellar cystic lesion extended to right frontal lobe in first surgery to recurrent brain mass which was pathology approved as SCC after 11 months.
Case Presentation
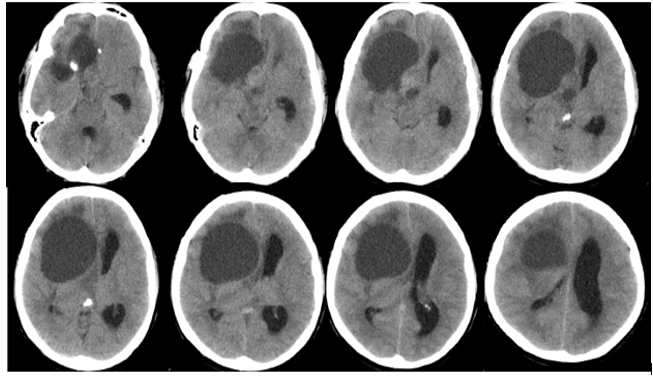
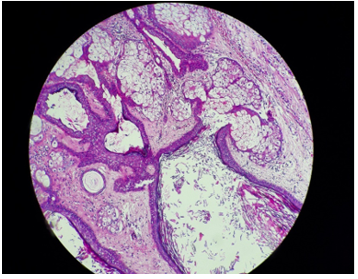
A 45-year-old male patient presented to the outpatient department of neurosurgery with complaints of severe headache of 3-months duration. He was apparently well before this episode. On examination, there was right hemi-anopia. The rest of general physical examination and neurological examination was normal. Hematological assessment and serum markers revealed no abnormality. Non-Contrast CT scan revealed a homogenous right parasellar and frontal cyst with peripheral rim of calcification. This mass was found to be compressing over the lateral and fourth ventricle resulting (Figure. 1). The tumor was removed via the sub frontal approach in the supine position, and surgery revealed on gross inspection a large cyst with a thin layer of white capsule containing yellowish-white, firm in consistency, and cheesy material. The cyst including the capsule and contents was removed completely. The patient recovered without incident, and the histological diagnosis was epidermoid cyst. ( Figure-2)
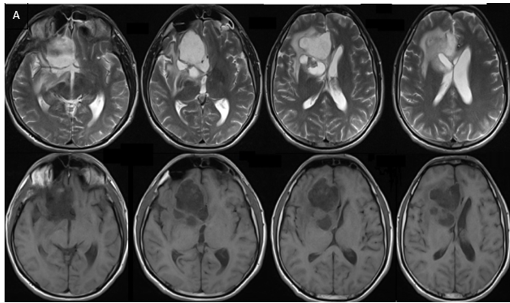
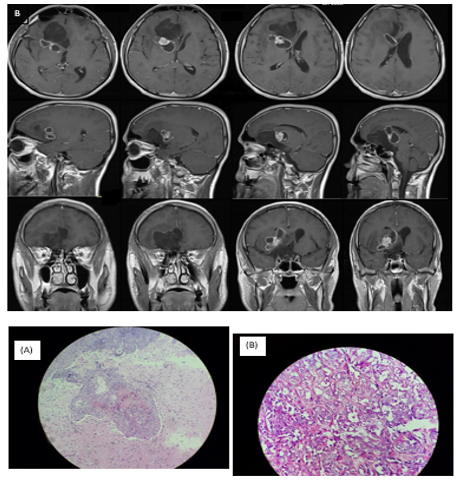
Six months after the initial surgery, he again manifested severe intermittent headache, right eye blindness and intracranial pressure (ICP). MRI demonstrated a large heterogeneous mass isointense on T1-weighted image, hyperintense on T2- weighted image, strongly enhanced after gadolinium, expanding from upper-Sella to right frontal and unusual edema (Figure 3). Rapid neurological deterioration associated with the site of the enhanced lesion in MRI suggests malignant transformation of EC. He underwent followed by second total brain resection of the recurrent tumor, and histological biopsy assessment of the specimen showed a cystic lesion lined by bland squamous epithelium and filled with laminated keratin which gathered with several small scattered islands of severely atypical squamous epithelium. These locations of typical epidermal cyst were collocated with zones that displayed marked nuclear irregularity with mitotic activity and an infiltrative growth pattern (Figure 4-5). Immunohistochemistry (IHC) showed positivity of the tumor cells for P53 protein. Based on these findings, the diagnosis of squamous cell carcinoma (SCC) approved in an EC was made.
Discussion
The authors provided a 43 years old male patient with two malignant transformation of epidermoid cyst tumor to SCC in secondary surgery. Malignant transformation of an epidermoid cyst tumor to SCC has been seldomly described in the reports. [7] Based on our current research, The patient’s age ranged from 40 to 85 years (mean age 53 years) and female was more reported. The mechanism of malignant transformation of a remnant benign EC to SCC is still imprecise. [8]
It has been described that long term inflammation prompt from spillage of materials comprising within the EC due to either perused cyst rupture and perhaps come up with by intra-operative introduction of foreign materials may lead to cellular atypia to neoplasia. [9] Another hypothesis assigns malignant transformation of benign EC to carcinoma in situ formation. [10]
Progression of clinical symptoms is the most important indicator of malignant transformation of EC. Previous reports described malignant interval time were highly variable ranged from 2 months to 33 years with average presenting time within 2 years of primary diagnosis. [11] consequently, in a stable patient after total or subtotal resection of an intracranial epidermoid cyst tumor, clinical and image follow-up every 6 months for 2 years and annually thereafter is necessary. besides, supposing developing clinical worsening in a formerly stable patient emergent brain MRI must be evaluated. [12] Although, past researches reported malignant transformation of EC to SCC in brain parenchyma, Somasundaram described this phenomenon in spinal cord. [5]
Malignant transformation of intracranial epidermoid cysts appears as
predominant enhanced by contrast imaging. Benign intracranial epidermoid cyst tumor commonly demonstrated on imaging low signal intensity on T1-weighted MRI, high signal intensity on T2-weighted MRI and restricted diffusion on diffusion weighted MRI. after contrast, minimal rim enhancement may be seen in 25% of the patients. [7] Malignant transformation exhibits on image by the edema, tissue invasion, rapid growth, and new enhancement following contrast. accordingly, new contrast enhancement of a residue intracranial EC need tissue diagnosis before adjuvant therapy for malignant transformation is considered.[13] In addition, Macmahon et al, reported malignant transformation of epidermoid cyst to glioblastoma. [14]
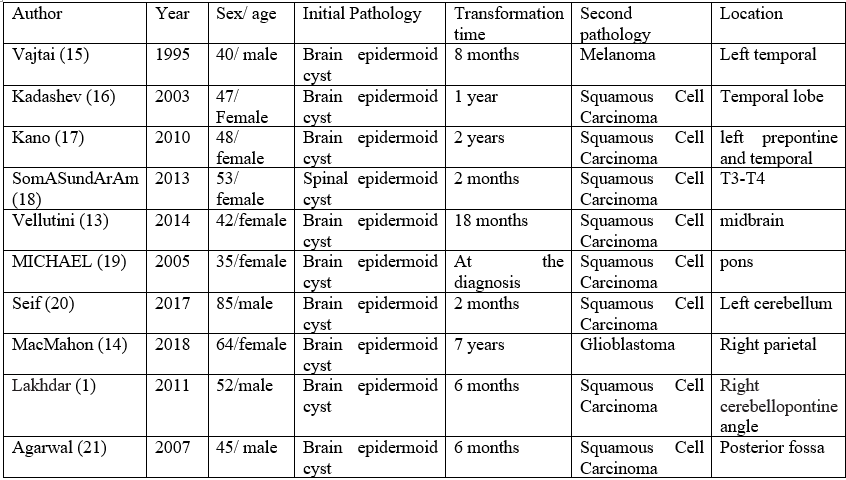
The maximum management of an epidermoid cyst tumor is total surgical resection of both cyst and inside components. However, total gross resection is possible in only 70-80% of the patients. [10] treatment of intracranial SCC arising in a residual EC is controversial and poor prognosis is reported. [1] We have known, patients’ mortality period ranged from 3 months to 5 years. consequently, Nagasawa et al., reported an overall survival of 6.6 months for patients with malignant transformation of a benign EC to SCC treated with surgery only and a significant growing in survival to 12.7 months when adjuvant radiotherapy was used. [12] The average survival time for patients’ management with surgery alone was only 1 month, for those treated with surgery plus external-beam radiation was 18 months, and the median survival time for those managed with surgery plus stereotactic radiosurgery was 44 months. [12] we recommend that stereotactic radiosurgery offers the optimistic survival rate. We review past reports about malignant transformation of EC to SCC. (Table 1).
Table 1. Reports about malignant transformation of EC to SCC.
Finally, malignant transformation of a residual epidermoid cyst tumor is a rarely occurrence with controversial management and poor prognosis. The results of our case the optimal method for treating malignantly transformed ECs is resection with adjuvant radiotherapy. Attentive clinical observation of patients should be performed after resection of brain ECs, given that this report suggests that malignant transformation can occur even months after resection of an EC. Prospective studies are required to define optimal management of patients presenting with squamous cell transformation of a remnant benign EC.
References
- Lakhdar F, Hakkou EM, Gana R, Maaqili RM, Bellakhdar F. Malignant transformation six months after removal of intracranial epidermoid cyst: a case report. Case Reports in Neurological Medicine. 2011;2011.
View at Publisher | View at Google Scholar - Czernicki T, Kunert P, Nowak A, Wojciechowski J, Marchel A. Epidermoid cysts of the cerebellopontine angle: Clinical features and treatment outcomes. Neurologia i neurochirurgia polska. 2016;50(2):75-82.
View at Publisher | View at Google Scholar - Vellutini EAS, de Oliveira MF, Ribeiro APC, Rotta JM. Malignant transformation of intracranial epidermoid cyst. British Journal of Neurosurgery. 2014;28(4):507-509.
View at Publisher | View at Google Scholar - Ding S, Jin Y, Jiang J. Malignant transformation of an epidermoid cyst in the temporal and prepontine region: Report of a case and differential diagnosis. Oncology letters. 2016;11(5):3097-100.
View at Publisher | View at Google Scholar - Somasundaram A, Lesser GJ, Mott RT, Hsu W. Malignant transformation of an intramedullary epidermoid cyst in the thoracic region of the spinal cord: Case report. Journal of Neurosurgery: Spine. 2013;19(5):591-594.
View at Publisher | View at Google Scholar - Liu X, Chen Z, Dong Y, He X, Pan X, Tong D. Primary intracranial squamous cell carcinoma arising de novo: a case report and review of the literature. World Neurosurgery. 2018;120:372-381.
View at Publisher | View at Google Scholar - Shear BM, Jin L, Zhang Y, David WB, Fomchenko EI, Erson-Omay EZ, et al. Extent of resection of epidermoid tumors and risk of recurrence: case report and meta-analysis. Journal of Neurosurgery. 2019;133(2):291-301.
View at Publisher | View at Google Scholar - Pikis S, Margolin E. Malignant transformation of a residual cerebellopontine angle epidermoid cyst. Journal of Clinical Neuroscience. 2016;33:59-62.
View at Publisher | View at Google Scholar - Yawn RJ, Patel NS, Driscoll CL, Link MJ, Haynes DS, Wanna GB, et al. Primary epidermoid tumors of the cerebellopontine angle: a review of 47 cases. Otology & Neurotology. 2016;37(7):951-955.
View at Publisher | View at Google Scholar - Mangraviti A, Mazzucchi E, Izzo A, Sturdà C, Albanese A, Marchese E, et al. Surgical management of intracranial giant epidermoid cysts in adult: A case-based update. Asian journal of neurosurgery. 2018;13(4):1288.
View at Publisher | View at Google Scholar - Chen Z, Araya M, Onishi H. Proton beam therapy for malignant transformation of intracranial epidermoid cyst. BMJ Case Reports CP. 2019;12(7):e229388.
View at Publisher | View at Google Scholar - Kaneko T, Fujinaga Y, Ichinohe F, Ogiwara T, Horiuchi T. Spontaneous regression of radiologically diagnosed epidermoid cyst originating from the cerebellopontine angle. World Neurosurgery. 2020;144:238-243.
View at Publisher | View at Google Scholar - Vellutini EA, de Oliveira MF, Ribeiro AP, Rotta JM. Malignant transformation of intracranial epidermoid cyst. Br J Neurosurg. 2014;28(4):507-509.
View at Publisher | View at Google Scholar - MacMahon P, Labak CM, Martin-Bach SE, Issawi A, Velpula K, Tsung AJ. Glioblastoma formation in a recurrent intracranial epidermoid cyst: a case report. CNS Oncol. 2018;7(4):Cns25.
View at Publisher | View at Google Scholar - Vajtai I, Tassi D, Varga Z, Tarjányi J, Vörös E. [Malignant melanoma evolving inside a cerebral epidermoid cyst]. Orv Hetil. 1995;136(22):1171-1174.
View at Publisher | View at Google Scholar - Kadashev BA, Shkarubo AN, Korshunov AG, Murusidze NA, Taniashin SV. [Malignant transformation of epidermoid cyst]. Zh Vopr Neirokhir Im N N Burdenko. 2003(1):38-40.
View at Publisher | View at Google Scholar - Kano T, Ikota H, Kobayashi S, Iwasa S, Kurosaki S, Wada H. Malignant transformation of an intracranial large epidermoid cyst with leptomeningeal carcinomatosis: case report. Neurol Med Chir (Tokyo). 2010;50(4):349-353.
View at Publisher | View at Google Scholar - Somasundaram A, Lesser GJ, Mott RT, Hsu W. Malignant transformation of an intramedullary epidermoid cyst in the thoracic region of the spinal cord: case report. J Neurosurg Spine. 2013;19(5):591-594.
View at Publisher | View at Google Scholar - Michael LM, 2nd, Moss T, Madhu T, Coakham HB. Malignant transformation of posterior fossa epidermoid cyst. Br J Neurosurg. 2005;19(6):505-510.
View at Publisher | View at Google Scholar - Seif B, Pourkhalili R, Shekarchizadeh A, Mahzouni P. Malignant Transformation of an Intracranial Extradural Epidermoid Cyst into Squamous Cell Carcinoma Presented with Cerebrospinal Fluid Leakage. Adv Biomed Res. 2017;6:16.
View at Publisher | View at Google Scholar - Agarwal S, Rishi A, Suri V, Sharma M, Satyarthi G, Garg A, et al. Primary intracranial squamous cell carcinoma arising in an epidermoid cyst—a case report and review of literature. Clinical neurology and neurosurgery. 2007;109(10):888-891.
View at Publisher | View at Google Scholar

 Clinic
Clinic
