Research Article | DOI: https://doi.org/DOI:10.31579/ 2835-8147/049
Education and Training of Nurses Who Work in Interventional Radiology Services a Special Way of Doing it
1 Investigation Group on Minimally Invasive Techniques Guided by Imaging of the Government of Aragon (Spain). GITMI
2 Interventional Radiology Hospital Parc Tauli Sabadell. Spain President of AEERVI
*Corresponding Author: De Gregorio MA, Investigation Group on Minimally Invasive Techniques Guided by Imaging of the Government of Aragon (Spain). GITMI.
Citation: De G. MA, Yamamoto M, Piquero MC, Langarita I, Gutierrez A, Guirola JA, (2024), Education and Training of Nurses Who Work in Interventional Radiology Services a Special Way of Doing it, Clinics in Nursing, 3(3) DOI:10.31579/ 2835-8147/049
Copyright: © 2024, De Gregorio MA. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 09 February 2024 | Accepted: 18 March 2024 | Published: 01 May 2024
Keywords: interventional radiology; nursing education; specialized training; master's program; professional development; health care specialization
Abstract
Objective: The objective of this study is to evaluate the effectiveness of a pioneering Master's program in bridging the educational gap for nurses in Interventional Radiology (IR) Developed by the University of Zaragoza's research group in Image-Guided Minimally Invasive Techniques and supported by professional societies, the program aims to provide comprehensive training, combining theoretical knowledge with practical skills, to meet the increasing demand for specialized nursing care in IR.
Materials and Methods: This study involves a Master's program offering a blend of theoretical and practical training, including the use of animal models and simulators. The program is evaluated based on enrollment data, satisfaction rates, and the practical applicability of the training. A total of 62 nurses from across Spain participated in the program, which includes 62 ECTS credits. Surveys assessed theoretical content, practical skills, and overall satisfaction, with a focus on the program's ability to meet educational expectations and its relevance to professional development in clinical settings.
Conclusion: The Master's program has demonstrated significant effectiveness in addressing the educational needs of nurses in the specialized field of IR. With an overall satisfaction rate of over 90% and a high rate of applicability of learned skills to professional practice, the program underscores the need for specialized training in nursing education. The findings advocate for the active involvement of nursing faculties, health administration, and professional societies in promoting specialized nursing training. This approach not only enhances the professional development of nurses but also promises to improve patientcare outcomes and the efficiency of the health system. Future research should focus on the long-term impact of such programs and the expansion of specialized training to other areas of emerging healthcare needs.
Abbreviations:
CIRSE: Cardiovascular and Interventional Radiological Society of Europe; | GITMI: Research Group on Minimally Invasive Techniques; |
EBIR: European Board of Interventional Radiology; | MDC: Master’s Degree Course; |
AEERVI: Spanish Association of Nursing in Vascular and Interventional Radiology; | SERVEI: Spanish Society of Vascular and Interventional Radiology; |
ECTS: European Credit Transfer System; | SIDI: Ibero-American Society of Interventional Radiology; |
IR: Interventional Radiology; | UEMS: European Union of Medical Specialists; |
IRs: Interventional Radiologists; | MFP: Master's Final Project |
Introduction
There are no precise figures on the number of nurses who dedicate part or all of their time to interventional practices. The American Association of Nurse Practitioners (2016) estimates that more than 222,000 licensed Nurse Practitioners (NPs)in the United States work in primary, outpatient, acute, and hospital settings. Additionally, the number of Nurse Practitioners in intensive care settings and other specific specialties has seen a significant increase over the last decade (Echenique et al., 2019). In Spain, although exact figures are not available, it is estimated that more than two hundred nurses work in interventional operating rooms with varying degrees of dedication to interventional practices.
Nursing plays a crucial role in the operating rooms of Image-Guided Minimally Invasive Surgery. There are two significant challenges for nursing education in Interventional Radiology (IR). In the vast majority of universities, the nursing degree does not include or teach specific content on IR, both theoretical and practical. Postgraduate training is left to the hospital IR services or units. Access to IR services is not determined by qualification or certification but by non-academic merits, such as years of work experience in the health system.
Recent literature highlights the increasing complexity of procedures in Interventional Radiology and the essential role nurses play in these environments. Studies like the one by Echenique underline the need for specialized training for nurses in IR, highlighting the gap between generalist training and the specific skills required. Furthermore, research by Dittman et al. (2018) emphasizes the importance of practical experience and ongoing training in advanced technologies and patient care protocols in IR. However, there is a lack of standardized and accessible training programs, leading to significant variations in the preparation and competence of nurses in this field.
Our study aims to address these gaps identified in the literature, presenting an innovative training model that integrates both theoretical knowledge and specific practical skills for IR. This approach seeks not only to improve nurses' preparedness for the technical and clinical challenges of IR but also to facilitate a more structured and meritocratic pathway to these specialized roles.
In summary, a method to enhance the education and training of nurses working in Interventional Radiology is presented, as well as the need to address current challenges in nursing education to ensure quality care in minimally invasive medical procedures guided by imaging.
Materials and Methods
From 2020 to the present, the University of Zaragoza has organized four editions (one per year) of the "Master’s Degree in Continuing Education in Vascular and Non-Vascular Image-Guided Minimally Invasive Surgery for Nursing." These courses are classified as Master's degrees since they consist of 60 ECTS credits (European Credit Transfer System) equivalent to 1800 hours of academic work. The Master's program is organized by the University of Zaragoza and endorsed by the esteemed College of Nursing of Zaragoza, the Ibero-American Society of Interventionism (SIDI), the Spanish Society of Vascular and Interventional Radiology (SERVEI), and the Spanish Association of Nursing in Vascular and Interventional Radiology (AEERVI).
To ensure relevant and high-quality practical training, hospitals for clinical practice were selected based on stringent criteria that included accreditation in Interventional Radiology, a significant volume of interventional procedures performed annually, and the availability of qualified staff to supervise and teach students. Hospitals with established training programs in Interventional Radiology were prioritized, as well as those offering a wide range of procedures for student observation and participation.
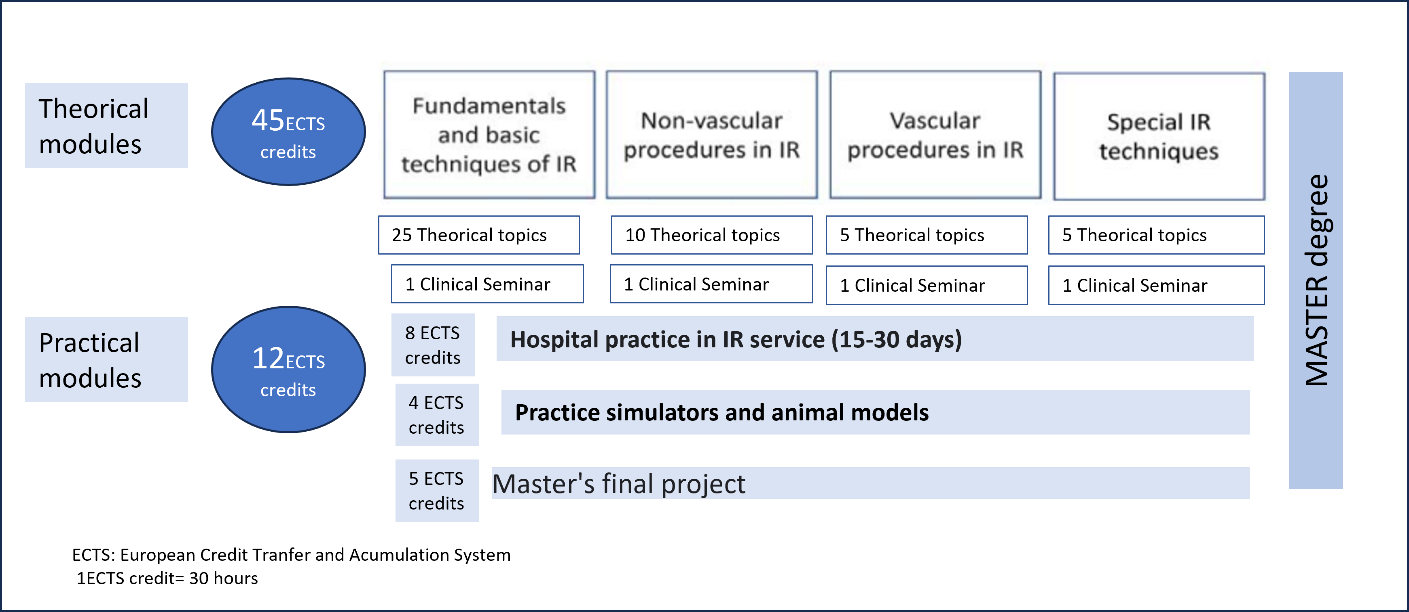
Figure 1: MDC organization chart and distribution and ECTS credits of the MDC program.
Inclusion criteria for patients involved in practical training were based on the educational relevance of the cases, ensuring students had the opportunity to observe and participate in a variety of procedures covering the program's key competencies. High-risk cases or those with ethical or privacy considerations that could complicate student participation were excluded. Patient selection was always conducted with informed consent and in compliance with established ethical and privacy protocols.
Practical content is carried out in Interventional Radiology services of accredited hospitals in the students' area of location. Additionally, 10 hours of practice on animal models and simulators on the most relevant topics are conducted. Before receiving the Master's degree, students must complete and pass a Master's Final Project (evaluative) signed by the rector of the University.
It is mandatory in the Master's program at UNIZAR to conduct surveys evaluating the teaching content, faculty, and objectives. These surveys are overseen by the university administration. Two different surveys were conducted among students of the four editions of the Nursing Master's program already completed. The survey on theoretical content was conducted online, while the survey on practical content was conducted in person, coinciding with the practices on animal models and simulators. Each of the two surveys consisted of five general questions and were anonymous. Figures 2-3.
Figure 2: Surveys to Master's students in relation to theoretical content
 |
Figure 3: Surveys to Master's students in relation to practical content
Surveys were evaluated in both positive and negative terms (numerical value and percentage), and finally, "Don't know/No answer" was also given a numerical value and percentage.
Results
A total of 62 students from various Spanish regions enrolled. The average daily study time dedicated to theoretical content was 74 minutes, with a range from 61 to 134 minutes. Regarding the number of students per academic year, the average was 13 students, with a range from 12 to 16 students. The participation rate in forums was high, exceeding 70% of students who participated at least once. Forty-eight students, representing 92.3%, passed the evaluations, achieving a 100% approval rate when considering the practical grade and the Master's Final Project. Attendance at practices with animal models and simulators was 67.7%. The survey results, for both theoretical and practical content, are presented in Figures 4 and 5. It is important to note that the surveys on theoretical content were answered by all students (62 students, 100%), while those related to practical content were answered by 51 students, representing an 82.2% participation rate.
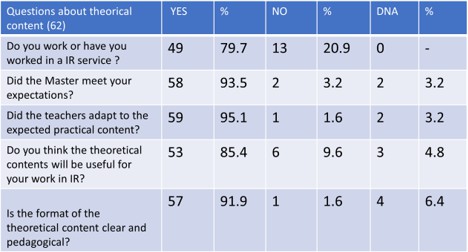
Figure 4A: Survey on theoretical contents
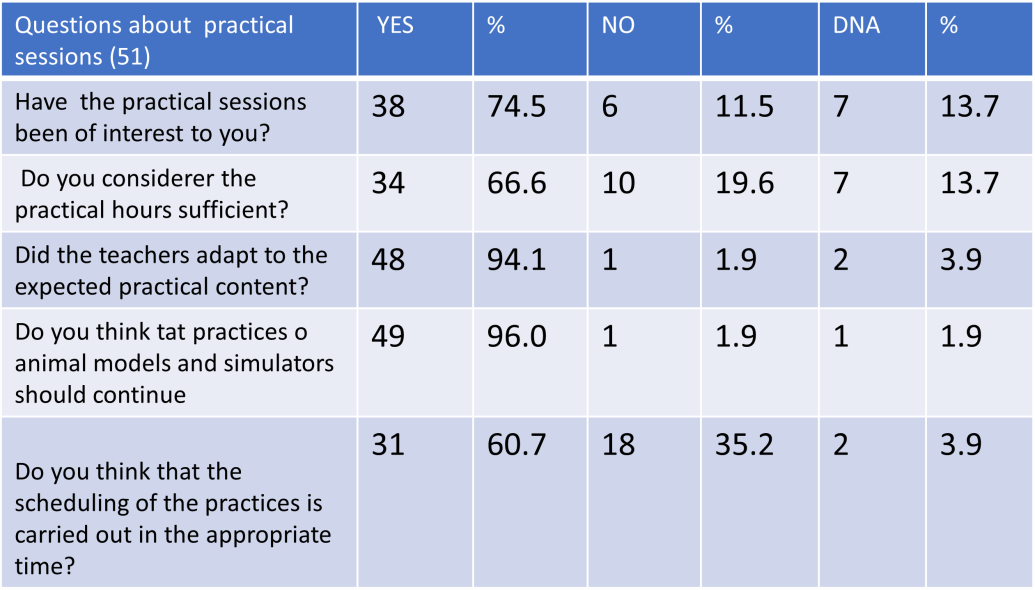 |
Figure 4B: Survey on practical content
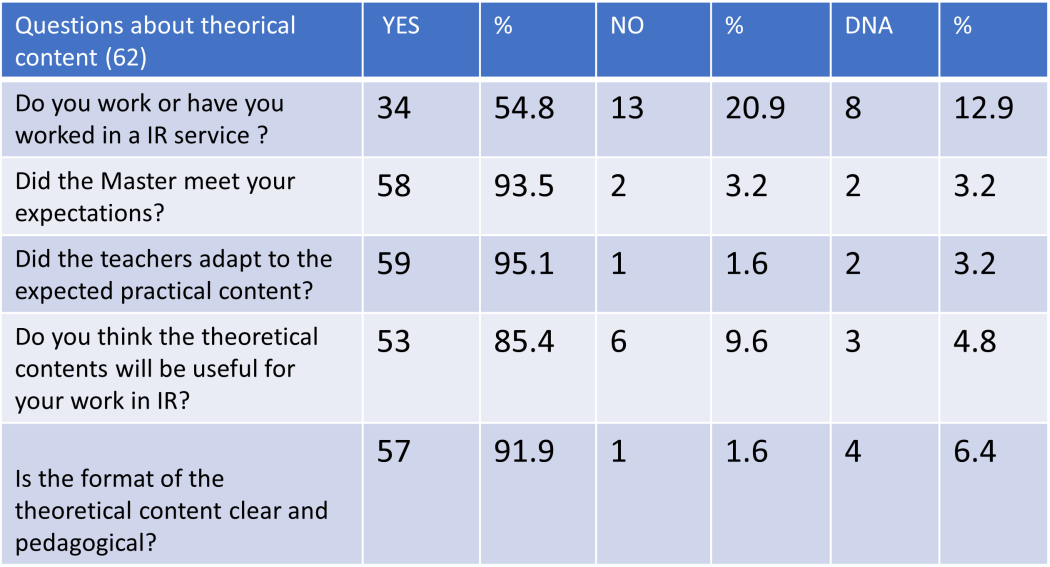 |
Figure 5: Survey on practical content
Approximately 80% of the students were working or had worked in the Interventional Radiology (IR) service. However, 11 of them (17.7%) did not have stable employment, and although they expressed interest in IR, they had not had the opportunity to choose that job position. The majority (93% of the students) felt that the Master's program had met the educational expectations they had at enrollment. The instructors adapted to the preset program in 95% of cases. Additionally, 85?lieved that what they learned would be useful for their job. The theoretical content was well written and clear for 91.9% of the students.
Discussion
The role that nurses play in tertiary hospitals, where the progress and development of super-specialization have necessitated the creation of multidisciplinary teams, is undeniable, with nursing playing a significant role in areas such as palliative care and critical care units (Dittman K, 2018; Heale R, 2014). In some countries, like the United States, the proliferation of nursing specialties was so significant that, in 2008, the National Council of State Boards of Nursing published a document on the uniformity of nursing practices (Harris C, 2014). However, in Spain, except for very specific activities, nursing specialization is not established, highlighting the need to adapt to the demands for specialization in certain medical areas, such as Interventional Radiology and Interventional Cardiology (Echenique & Wempe, 2019).
The lack of qualified nurses can cause dysfunctions in medical teams and require a significant amount of time to reach the appropriate qualification level. It is concerning that many nursing faculties lack theoretical and practical training in specialized medical areas, underscoring the need for changes in undergraduate teaching to adapt to new techniques and advanced knowledge (Avadhani, 2017).
Theoretical-practical master's programs for nursing and expert courses offered by some universities, along with the support of scientific societies and associations, can play a crucial role in overcoming these training deficiencies. Our Master's program, an initiative of a research group in Image-Guided Minimally Invasive Techniques at the University of Zaragoza and endorsed by professional societies of radiologists and interventional nurses (SERVEI and AEERVI), has proven to be an effective initiative to address these training needs. In these four editions, 62 nurses from across the country have enrolled, achieving overall satisfaction of over 90% in both theoretical and practical areas. The practical contents, based on animal models and simulators, are considered sufficient to acquire the necessary skills for professional development in the clinic (Scherer K, 2019; Miller ZA, 2019).
We conclude that the Nursing Master's is a regulated education in Interventional Radiology, evaluated and supervised by a university, which grants an official qualification of 62 ECTS credits. It is imperative that more entities, such as the Health Administration, Nursing Faculties, and Nursing Societies, get involved in this effort to contribute to the training and professionalization of nursing in Interventional Radiology.
Future implications and directions for additional studies include the need to evaluate the long-term impact of these training programs on patient care outcomes and the efficiency of the health system. It would also be beneficial to explore the development of specialization programs in other areas of emerging need, ensuring that nursing training keeps pace with technological advances and new medical practices. Finally, it is crucial to research and address the barriers to access to specialized education, in order to promote equity in training and professional development opportunities for nurses in various geographic and socioeconomic contexts.
Conclusion
It is essential for entities such as the Health Administration, Nursing Faculties, and Nursing Societies to actively involve themselves in promoting the training and professionalization of nursing in specialized areas such as Interventional Radiology. This will not only improve work efficiency but will also directly benefit patients.
This comprehensive approach not only proposes immediate improvements in nursing training but also raises fundamental questions for future research, aiming to continuously adapt nursing education and practice to the changing demands of specialized healthcare.
References
- Echenique A, Wempe EP. (2019). Simulation-Based Training of the Nurse Practitioner in Interventional Radiology. Tech Vasc Interv Radiol. 22(1):26-31.
View at Publisher | View at Google Scholar - Dittman K, Hughes S. (2018). Increased Nursing Participation in Multidisciplinary Rounds to Enhance Communication, Patient Safety, and Parent Satisfaction. Crit Care Nurs Clin North Am.
View at Publisher | View at Google Scholar - Harris C. (2014). Bridging the gap between acute care nurse practitioner education and practice: The need for postgraduate residency programs. J Nurse Prac. 10:331- 336.
View at Publisher | View at Google Scholar - Shogi M, Sajadi M, Oskuie F, Dehnad A, Borijemad L. (2019). Hellyion. 5:e2503.
View at Publisher | View at Google Scholar - Heale R, Dickieson P, Carter L, et al. (2014). Nurse practitioners’ perceptions of interprofessional team functioning with implications for nurse managers. J Nurs Manag. 22:924-930.
View at Publisher | View at Google Scholar - Scherer K, Winokur RS. (2019). Multidisciplinary Team Training Simulation in Interventional Radiology. Tech Vasc Interv Radiol. 22(1):32-34.
View at Publisher | View at Google Scholar - Miller ZA, Amin A, Tu J, Echenique A, Winokur RS. (2019). Simulation-based Training for Interventional Radiology and Opportunities for Improving the Educational Paradigm. Tech Vasc Interv Radiol. 22(1):35-40.
View at Publisher | View at Google Scholar - Avadhani A. (2017). Should procedural skills be a part of the Acute Care Nurse Practitioner curriculum? Nurse Educ Today. 50:115-118.
View at Publisher | View at Google Scholar

 Clinic
Clinic
