Research Article | DOI: https://doi.org/10.31579/2835-7949/001
COVID-19 Risk in Patients with Substance use Disorders at Kuwait Addiction Treatment Center
- Sameh Mohamed Yousri Bondok 1*
- Marwa Mohsen Ramadan 1
- Adel Desoky 1
- Ayman Abdelkader 1
- Mohamed Helmi 1
- Hossam Ahmed 1
- Mina Ibrahim 1
- Sherif Sobhy 1
- Mohamed Hassan 1
- Shaymaa Shabeb 1
- Duaa Zaki 1
- Adel Al Zayed 1
1 Consultant Psychiatrist. Ain Shams University, Kuwait.
*Corresponding Author: Sameh Mohamed Yousri Bondok, Consultant Psychiatrist. Ain Shams University, Kuwait.
Citation: Sameh Mohamed Yousri Bondok, Marwa Mohsen Ramadan, Adel Desoky, Ayman Abdelkader, Mohamed Helmi, (2022) COVID-19 Risk in Patients with Substance use Disorders at Kuwait Addiction Treatment Center. Biomedical Research and Clinical Trials, 1(1): DOI: 10.31579/2835-7949/001
Copyright: © 2022, Sameh Mohamed Yousri Bondok, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 09 September 2022 | Accepted: 14 September 2022 | Published: 29 September 2022
Keywords: substance use disorder; COVID-19; mental health
Abstract
Background: The COVID-19 pandemic is creating major issues for healthcare and broad social structures, exposing societal vulnerabilities. Patients with substance use disorder are considered at increased risk of COVID-19 and its more serious complications, however data on the impact of COVID-19 are lacking. The study aimed to describe the clinical characteristics and outcomes of COVID-19 on patients with substance use disorders seen at Kuwait addiction treatment center.
Method: A cross sectional study was carried including all patients seen in outpatient department and/or admitted in the inpatient wards of Kuwait Addiction Treatment Center, diagnosed as substance use disorder with history of COVID-19 infection during the period from June 2021 to December 2021.
Results: Among 660 substance use disorder patients, the mean age was 36± 10.1 years (94Percentage) were men and (91.1Percentage) were Kuwaiti. The main substance used were Opioid in (41.1Percentage) of patients, stimulant in (25.5Percentage) and synthetics in (11.2Percentage) of patients. One or more comorbidities associated to COVID-19 risk were observed in (29 Percentage) of patients. (9.1Percentage) of patients got COVID-19 infection and 61.5Percentage were vaccinated.
Conclusion: In spite of the hypothetical risk for COVID-19 among patients with SUD, current study declared low prevalence of COVID -19 infection among patients with SUD.
Background, Problem Statement and Aims:
Substance use disorders (SUDs), are complex disorders that affect brain function and behavior, characterized by impaired functioning and considerable harm to the individuals with the disorders and to society as a whole (Grant, 2016).
It’s a global phenomenon affecting about 275 million people worldwide, which is roughly 5.6 per cent of the global population aged 15–64 years, used drugs at least once during 2016. Some of them about 31 million who use drugs suffer from drug use disorders, meaning that their drug use is harmful to the point where they may need treatment (UNDOC, 2018).
The novel coronavirus disease 2019 (COVID-19) is an acute respiratory illness, which raises mortality rates in older people and those with underlying medical conditions such as cardiovascular disease, chronic respiratory disease, diabetes and cancer (Yang et al, 2020).
People with substance use disorders (SUD) are considered at increased risk of COVID-19 and its more serious complications for multiple physiological and social causes (Wei and Shah, 2020).
Comorbidities prevalent among people with SUD, such as cardiovascular diseases, chronic respiratory diseases, diabetes, obesity and cancer, increase vulnerability to COVID-19 and are associated with more severe COVID-19 symptoms, complications and fatalities (Yang et al, 2020).
Moreover, high-risk behaviors such as sharing drug-using paraphernalia, difficulties to maintain quarantines and living in close contact with others in crowded shelters may contribute to the spread of COVID-19 among people with SUD (Wei and Shah, 2020).
In addition, social and economic changes caused by the pandemic, along with the difficulties regarding treatment access and adherence, can aggravate the SUD. Healthcare policies, including physical and social distancing isolation and restricted medical visits during the pandemic make it difficult for healthcare providers to address the needs of people with SUD with the availability of medications, harm reductions programs and mutual supports groups (Sheridan et al, 2020).
There is a little if any studies about COVID -19 risk in patients with SUD, although, there was a unique retrospective case-control study of electronic health records (EHRs) data at 360 U.S. hospitals, done by (Wang et al, 2021) showed that, among 73,099,850 patients, there was 12,030 had a diagnosis of COVID-19. Patients with a recent diagnosis of SUD (within past year) were at significantly increased risk for COVID-19 (adjusted odds ratio or AOR = 8.699 [8.411–8.997], P < 10−30), an effect that was strongest for individuals with OUD (AOR = 10.244 [9.107–11.524], P < 10−30), followed by individuals with tobacco use disorder (TUD) (AOR = 8.222 ([7.925–8.530], P < 10−30). Compared to patients without SUD. Patients with SUD had significantly higher prevalence of chronic kidney, liver, lung diseases, cardiovascular diseases, type 2 diabetes, obesity and cancer. Among patients with recent diagnosis of SUD, African Americans had significantly higher risk of COVID-19 than Caucasians (AOR = 2.173 [2.01–2.349], P < 10−30), with strongest effect for OUD (AOR = 4.162 [3.13–5.533], P < 10−25). COVID-19 patients with SUD had significantly worse outcomes (death: 9.6Percentage, hospitalization: 41.0Percentage) than general COVID-19 patients (death: 6.6Percentage, hospitalization: 30.1Percentage) and African Americans with COVID-19 and SUD had worse outcomes (death: 13.0Percentage, hospitalization: 50.7Percentage) than Caucasians (death: 8.6Percentage, hospitalization: 35.2Percentage). These findings identify individuals with SUD, especially individuals with OUD and African Americans, as having increased risk for COVID-19 and its adverse outcomes, highlighting the need to screen and treat individuals with SUD as part of the strategy to control the pandemic while ensuring no disparities in access to healthcare support (Wang et al, 2021).
Rationale of the study:
Despite this emerging health threat for people with substance use disorder, data on COVID-19 in relation to patients with substance use disorder were scant.
Hypothesis:
It is hypothesized that patients with substance use disorder are considered at increased risk of COVID-19 and its more serious complications.
Aim of the study:
To describe the clinical characteristics, related factors and clinical outcomes of COVID-19 in people with substance use disorder.
Research design and Methods:
Study design: This is a cross sectional exploratory study.
Characteristics of study area and target population:
This study carried out in Kuwait Addiction Treatment Center in the period between June 2021 and December 2021.
Patients seen in outpatient department and/or admitted in the inpatient wards of Kuwait Addiction Treatment Center diagnosed as substance use disorder with history of COVID-19 infection from the start of the pandemic on February 2020 to December 2021 will be included in the study.
Sampling:
All patients seen in outpatient department and/or admitted in the inpatient wards of Kuwait Addiction Treatment Center diagnosed as substance use disorder with history of COVID-19 infection during the period from June to December 2021.
Ministry of health record system will be checked for number of COVID -19 deaths associated with history of substance use disorder.
Data collection tools and measurements:
The study was explained to all participants and who consented to participate in the study were interviewed using Structured Clinical Interview for DSM-IV (SCID-I) and history of COVID-19 infection questionnaire.
Ethical Consideration
The study received ethical approval from the Kuwait Ministry of Health’s
Patients were ensured about the confidentiality of information. Participation in the study was completely voluntary, and patients were informed that they could withdraw from the assessment at any time. Moreover, they were informed that withdrawal from the study would not affect their management
Study procedure:
- Study aims and general principles were discussed with all participants and Written informed consent was obtained. And for ethical considerations included the observance of confidentiality and anonymity; the participants didn’t write their names on the questionnaire.
- Participant’s demographic data were registered in a designed Socio-demographic sheet.
- All patients were assessed using addiction treatment center semi-structured clinical sheet, including age, address, educational level, past psychiatric history, past medical history, family history of psychiatric disorders, or other medical illnesses and mental state examination.
- All patients were assessed for drugs use using urine drug screen and alcohol blood level.
- All patients are were interviewed using Structured Clinical Interview for DSM-IV (SCID-I) and history of COVID-19 infection questionnaire.
- Structured Clinical Interview for DSM-IV (SCID-I)16It is used to diagnose an axis I diagnosis. It will be applied to both groups. It is a semi-structured diagnostic interview which has been updated for DSM-IV. It begins with a section on demographic information and clinical background. Then there are 7 diagnostic modules, focused on different diagnostic groups: mood, psychotic, substance use, anxiety, somatoform, eating, and adjustment disorders. Both required and optional probes are provided, and skip outs are subjected when no further questioning is warranted. It is considered the standard interview to verify diagnosis in clinical trials and is extensively used in other forms of psychiatric research (First MB, et al 1995).
- History of COVID-19 infection questionnaire. It's a self - administrated questionnaire prepared to meet the objectives of the study and designed to collect the following data:
- Personal data: of the studied participant as (age, sex, marital status, occupation, main substance of use, duration of illness, medical comorbidity, on Opioid Substitution Treatment or not).
- History of COVID-19 infection and hospitalization.
- History of COVID-19 vaccine (type, number of doses).
- Ministry of health record system were asked for the number of COVID -19 deaths associated with history of substance use disorder.
Statistical Analysis: Results were reviewed, given codes, and enrolled into the Statistical Package for Social Science (IBM SPSS) version 23. Quantitative data were displayed as means, standard deviations, and ranges with parametric data. Also, non-quantitative data were displayed as numbers and percentages. Comparison in non-quantitative data was done by Chi-square test. Comparison in quantitative data with the parametric patterns was done by Independent t-test The confidence interval was established as 95Percentage and the accepted margin of error was established as 5Percentage. So p-value was said to be significant if less than 0.05.
Results
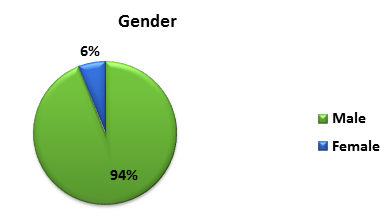
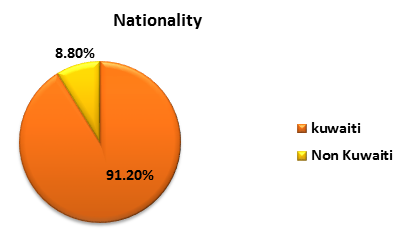
The study showed that, among 660 patients with substance use disorder, the mean age was 36.1 ± 10.1 years with age range 18–72 years, 94 Percentage (n =620) of the sample were males while 6Percentage (n = 40) were females. Kuwaiti patients represented 91.2Percentage (n = 602) while 8.8Percentage (n = 58) were non- Kuwaiti. (Figure 1, 2).
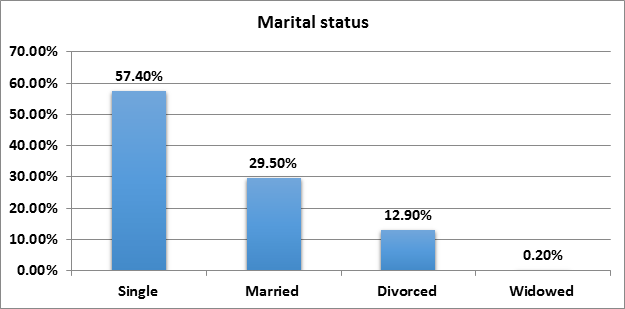
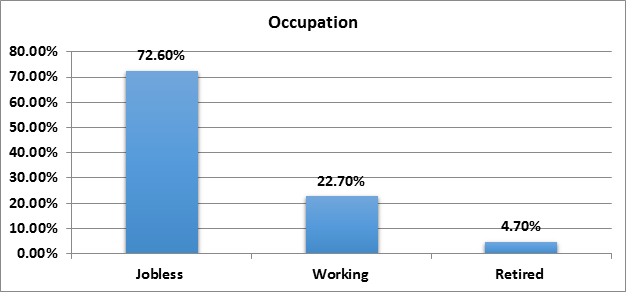
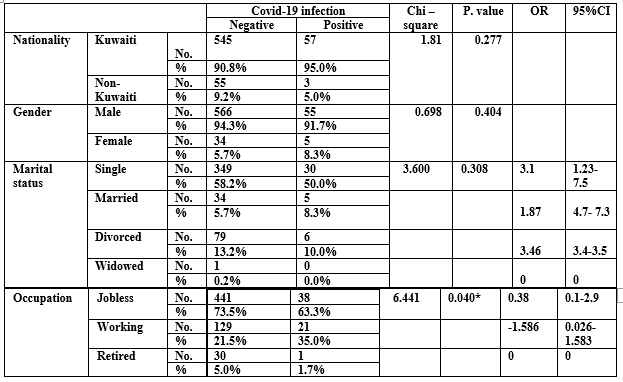
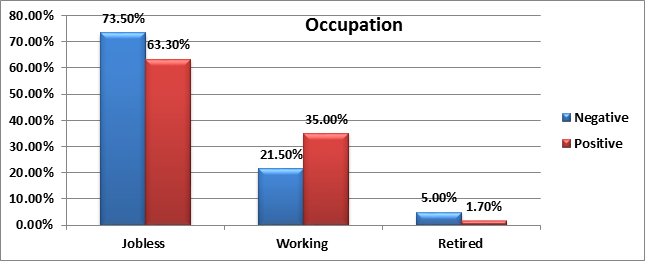
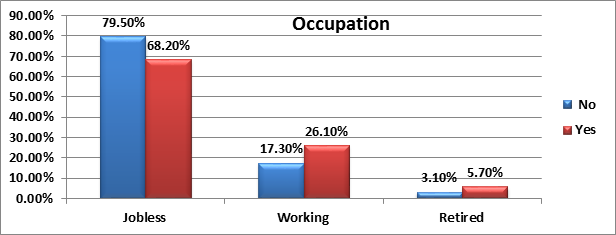
Among the studied sample 57.4Percentage (n = 379) were single, 29.5Percentage (n = 195) were married, 12.9Percentage (n = 85) were divorced and 0.2Percentage (n = 1) were widowed. Also, 72.6Percentage (n = 479) were jobless while 22.7Percentage (n = 150) had a job and 4.7Percentage (n = 31) were retired. (Figure 3, 4).
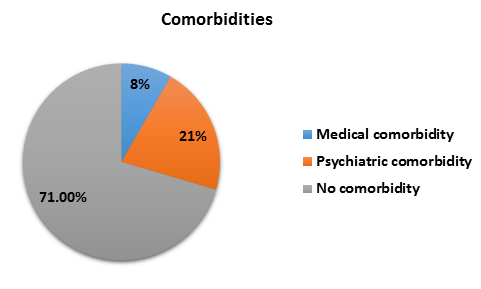
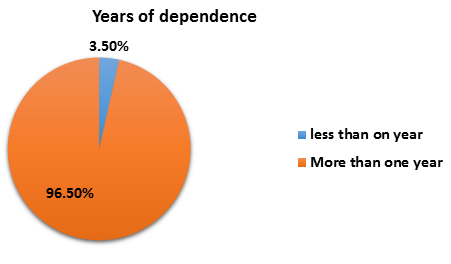
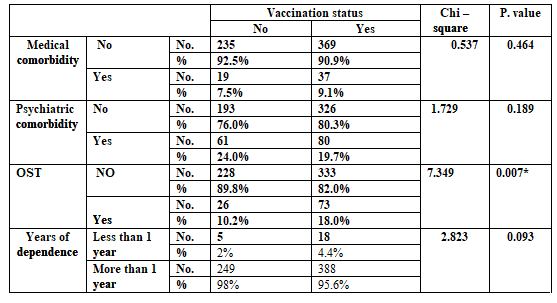
The study showed that, 8Percentage (n = 56) of the sample had medical comorbidity while 21Percentage (n = 141) had psychiatric comorbidity. Also, 15Percentage (n = 99) received oral substitution treatment and 96.5Percentage (n = 637) had a history of substance use disorder for more than one year. (Figure 5, 6).
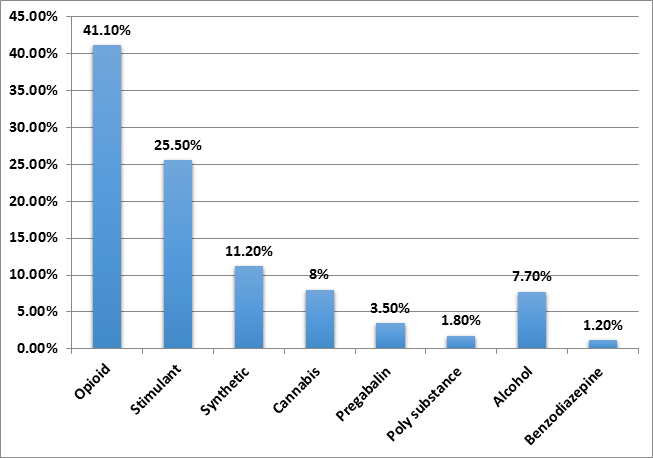
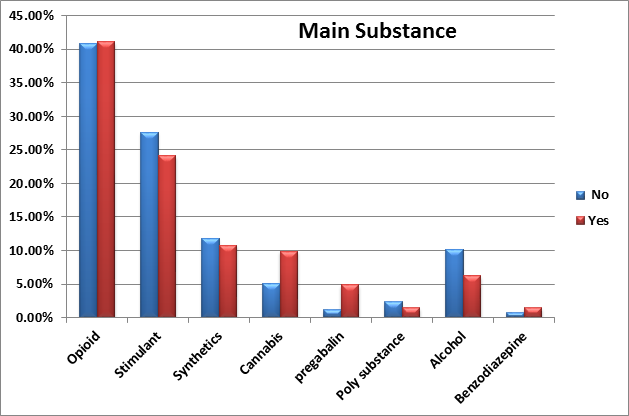
Among the 660 patients 41.1Percentage (n = 271) were opioid dependent, 25.5Percentage (n = 168) were stimulant dependent, 11.2Percentage (n = 74) were synthetics dependent, 8Percentage (n = 53) were cannabinoid dependent, 7.7Percentage (n = 51) were alcohol dependent, 3.5Percentage (n = 23) were pregabalin dependent, 1.2Percentage (n = 8) were benzodiazepine dependent and 1.8 Percentage (n = 12) were poly substance dependent. (Figure 7).
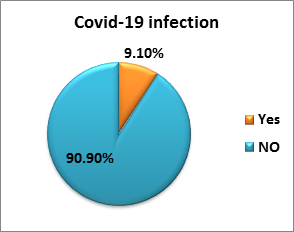
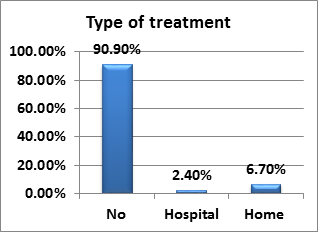
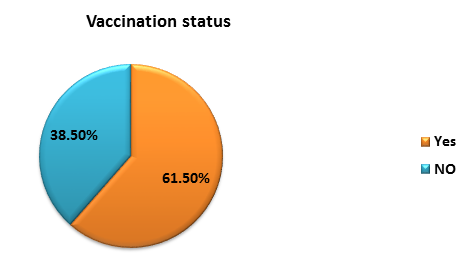
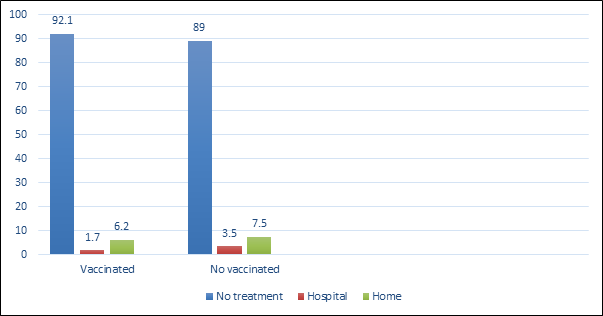
The study found that only 9.1Percentage (n = 60) of the studied sample were infected with COVID 19 virus, 2.4Percentage (n = 16) of them were hospitalized while 6.7Percentage (n = 44) received home treatment. Also, among the studied sample 61.5 Percentage (n = 406) were vaccinated while 38.5Percentage (n = 254) were non-vaccinated. (Figure 8, 9, 10).
There was no statistically significant difference in gender, nationality, marital status between the COVID-19 positive and negative groups, while there was a statistically significant difference in occupational status between the two groups as 63.3Percentage of COVID-19 positive were jobless and 35Percentage had a job while 1.7Percentage were retired (p=0.04). (Table 5). (Figure 11).
Meanwhile, divorced patients were at significantly increased risk for
COVID-19 (adjusted odds ratio or AOR = 3.46 [3.4–3.5], followed by single patients (AOR = 3.1 ([1.23–7.5]. then married patients (AOR = 1.87 ([4.7–7.3]. (Table 5).
Also, jobless patients were at significantly increased risk for COVID-19 (adjusted odds ratio or AOR = 0.38 [0.1–2.9], followed by worked patients (AOR = -1.586 ([0.026–1.583]. (Table 1).
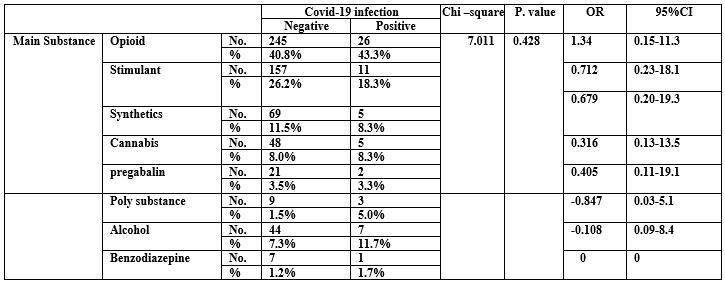
There was no statistically significant difference regarding type of substance between COVID 19 positive and negative groups (p =0.428).
Meanwhile patients with opioid use disorder were at significantly
increased risk for COVID-19 (adjusted odds ratio or AOR = 1.34 [0.15–11.3], followed by patients with stimulant use disorder (AOR = 0.712 ([0.23–18.1]. Then patients with synthetics use disorder (AOR = 0.679 ([0.20–19.3]. (Table 2).
There was no statistically significant difference in medical, psychiatric comorbidities or years of dependence between the COVID 19 positive and negative groups. Meanwhile patients with recent diagnosis of SUD (within past year) were at significantly increased risk for COVID-19 (adjusted odds ratio or AOR = 0.45 [0.15–1.39] (Table 3).
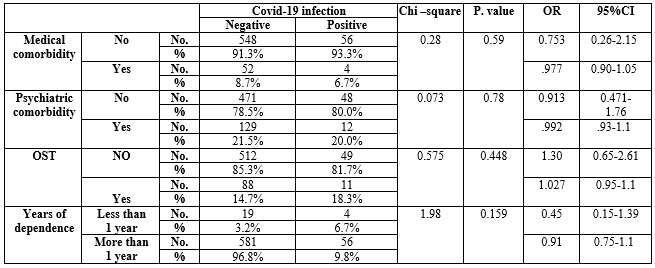
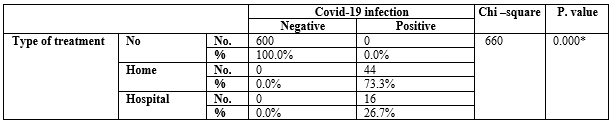
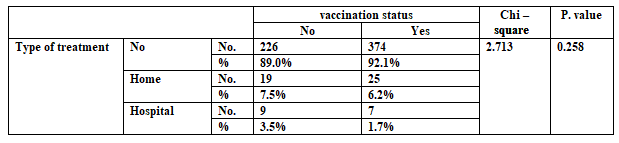
There was a statistically significant difference in kind of treatment received for COVID 19 infection between the two groups as 73.3Percentage of COVID 19 positive received home treatment and 26.7Percentage were hospitalized (p=0.000) (Table 4).
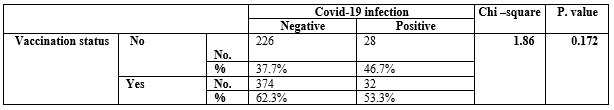
There was no statistically significant difference regarding vaccination status between COVID-19 positive and COVID-19 negative groups. (p= 0.172) (Table 5).
There was no statistically significant difference in gender, nationality, marital status between vaccinated and non-vaccinated groups, while there was a statistically significant difference in occupational status between the two groups as 68.2Percentage of vaccinated patients were jobless while 26Percentage had a job and 5.7Percentage were retired (p=0.006). (figure6).
There was a statistically significant difference regarding type of substance between the vaccinated and non- vaccinated groups were 41.1Percentage of opioid dependent, 24.1Percentage of stimulant dependent, 10.8Percentage of synthetics dependent, 9.9Percentage of cannabinoid dependent, 6.2Percentage of alcohol dependent, 4.9Percentage of pregabalin dependent, 1.5Percentage of benzodiazepine and poly substance dependent received vaccine. (p= 0.02)(Figure 7).
There was no statistically significant difference regarding medical or psychiatric comorbidities and years of dependence between the vaccinated and non-vaccinated groups. (Table 6).
There was no statistically significant difference in kind of treatment received for COVID 19 infection between vaccinated and non-vaccinated groups. (p= 0.258) (Table 11, Figure 7).
Discussion
Currently, there is little if any quantitative analysis of the risks and outcomes for COVID-19 infection in individuals suffering from substance use disorder. In addition, there is minimal data on how socio-demographic factor and other factors as comorbidities, type of substance used and vaccination status which may affect the risk and outcomes of COVID-19 among patients with substance use disorder.
Therefore, this study aimed to describe the clinical characteristics, related factors and clinical outcomes of COVID-19 in People with SUD seen in Kuwait addiction treatment center during the pandemic.
Main finding of this study
In spite of the hypothetical risk for COVID-19 among patients with SUD as reported by NIDA 2020, our study declared low prevalence of COVID -19 infection among patients with SUD, as among the studied 660 patients, only 9.1Percentage were infected with COVID 19 virus, 2.4Percentage of them were hospitalized while 6.7Percentage received home treatment.
Several factors could explain the low percentage of patients with substance use disorder admitted for COVID-19 pneumonia in this study.
First, despite Kuwait has been one of the Middle east countries affected by the COVID-19 pandemic so far, the findings from the recent national survey denotes a low prevalence of the disease in the general population (∼417,762 cases in December 2021) in comparison to other countries in Asia and Europe.
Second, among adults, the risk for severe illness from COVID-19 increases with age, as older adults at highest risk and representing more than 80Percentage of admitted patients with COVID-19 from the general population. By contrast, younger adults < 40>(Garg S et al, 2020). In this study, the mean age of the studied patients was ∼ 36 years.
Moreover, asymptomatic infections, which are more frequent in young adults under 40 years of age of the general population, could have contributed to the low number of COVID-19 among people with SUD.
Finally, the less sever COVID-19 symptoms could have been confused by patients as withdrawal symptoms especially opioids withdrawal. or that patients could have decided not to go to overwhelmed hospital emergency department during the epidemic, suggesting that a substantial number of symptomatic patients with COVID-19 did not undergo medical assessment.
Risk associations between SUD and COVID-19
The study showed that, the risk of COVID-19 infection in patient with substance use disorder increased among jobless and divorced patients. Meanwhile patients with opioid use disorder were at significantly increased risk for COVID-19 followed by patients with stimulant, then patients with synthetics use disorder.
Also, patients with a recent diagnosis of SUD (within past year) were at significantly increased risk for COVID-19, an effect that was strongest for individuals with opioid use disorder.
These results are consistent with study done by Wang et al, 2021. which revealed that patients with a recent diagnosis of SUD (within past year) were at significantly increased risk for COVID-19 an effect that was strongest for individuals with opioid use disorder.
The study showed that, there is no risk association of COVID 19 infection in patient with SUD with medical or psychiatric comorbidities. This result is inconsistent with study done by Wang et al, 2021. which revealed that, compared to patients without SUD, Patients with SUD had significantly higher prevalence of chronic kidney, liver, lung diseases, cardiovascular diseases, type 2 diabetes, obesity and cancer.
Effects of socio-demographics, type of substance on vaccination status
The current study revealed that, vaccination is more prevalent among jobless patients with opioid use disorder followed by Stimulant use disorder.
Vaccination status in relation to COVID-19 infection
Current study declared that, nearly half (46.7Percentage) of the studied patient with COVID-19 infection weren't vaccinated.
Conclusion
Despite this emerging health threat for patients with SUD, data on COVID-19 in relation to patients with SUD are scant. The low number of patients with SUD and COVID-19 seen in Kuwait addiction center in this study highlights the urgent need to carry out larger sample sizes and studying patients with SUD admitted with COVID 19 infection in general hospitals and ICU departments in order to more completely understand the effects of COVID-19 among patients with SUD.
Limitation of the day
Although our data collected from one treatment center may limit the generalization of the findings, the addiction treatment center is the referral center for Kuwait with the highest prevalence of people with SUD. Otherwise, the death rate related to COVID-19 in patients with SUD wasn't accessible.
References
- Garg S, Kim L, Whitaker M et al. (2020) Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 states, March 1-30, 2020. MMWR Morb Mortal Wkly Rep, 69(15):458–64.
View at Publisher | View at Google Scholar - Grant BF, Saha TD, Ruan WJ, et al (2016). Epidemiology of DSM-5 Drug Use Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. JAMA Psychiatry; 73:39–47.
View at Publisher | View at Google Scholar - National Institute on Drug Abuse. COVID-19: Potential Implications for Individuals with Substance Use Disorders. Available at: https: //www.drug abuse.gov/about-nida/noras-blog/2020/04/covid-19-potential-implications individuals-substance-use-disorders.
View at Publisher | View at Google Scholar - WeiY, ShahR. (2020) Substance use disorder in the COVID-19 pandemic:a systematic review of vulnerabilities and complications. Pharmaceuticals (Basel), 13(7):155.
View at Publisher | View at Google Scholar - Sheridan Rains L, Johnson S, Barnett P et al. (2020) Early impacts of the COVID-19 pandemic on mental health care and on people with mental health conditions: framework synthesis of international experiences and responses. Soc Psychiatry Epidemiol, 1–12.doi: 10.1007/s00127-020-01924-7.
View at Publisher | View at Google Scholar - Yang J, Zheng Y, Gou X et al. (2020) Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis Int J Infect Dis; 94:91–5.
View at Publisher | View at Google Scholar - First MB, Spitzer RL, Gibbon M, et al (1995). Structured Clinical Interview for DSM-IV Axis I Disorders-Pa-tient Edition (SCID-I/P, Version 2.0). New York: Biometrics Research Department, New York State Psychiatric Institute.
View at Publisher | View at Google Scholar - Quan Qiu Wang, David C. Kaelber, Rong Xu & Nora D (2021).Volkow Molecular Psychiatry, volume 26, pages 30–39.
View at Publisher | View at Google Scholar

 Clinic
Clinic
