Case Report | DOI: https://doi.org/10.31579/2835-785X/098
Coronary Artery to Pulmonary Artery Fistula: A Case Report and Literature Review
- Amit Mandal *
- Shobhit Priyanshu Joseph
Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
*Corresponding Author: Dr Amit Mandal, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
Citation: Amit Mandal, and Shobhit Priyanshu Joseph, (2025), Coronary Artery to Pulmonary Artery Fistula: A Case Report and Literature Review, International Journal of Clinical Research and Reports. 4(3); DOI: 10.31579/2835-785X/098
Copyright: © 2025, Amit Mandal. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 16 May 2025 | Accepted: 28 May 2025 | Published: 06 June 2025
Keywords: coronary artery fistulae; coronary angiography; coronary steal
Abstract
Coronary artery fistulae (CAFs) are rare congenital anomalies characterized by abnormal connections between the coronary arteries and major blood vessels or heart chambers. Coronary pulmonary artery fistulas (CPAFs) can be congenital or acquired. Mostly, CAFs are found as incidental findings on angiographic evaluation. The management of CPAFs varies from case to case depending on size, anatomical location, patient's clinical presentation, and presence of coronary steal phenomenon. We present a 48‐year‐old male who was found to have a right coronary to pulmonary artery fistula when evaluated for exertional dyspnoea.
Introduction
Coronary artery fistulae (CAFs) are rare congenital anomalies characterized by abnormal connections between the coronary arteries and major blood vessels or heart chambers. In children, these fistulae are often asymptomatic and discovered incidentally. However, adults with hemodynamically significant CAFs may experience symptoms and serious complications, including myocardial ischemia or infarction, aneurysm formation and rupture, arrhythmias, and congestive heart failure. Consequently, closure is recommended for large or symptomatic fistulae, which can be achieved through surgical or percutaneous methods. We present here a case of a 48‐year‐old male who was found to have a right coronary to pulmonary artery fistula when evaluated for exertional dyspnoea.
Case Report
A 48‐year‐old male presented with the complaints of palpitations on exertion and dyspnoea NYHA-II for 1 year on-off. There was no history of exertional chest pain or syncope or orthopnea. He gives history of pounding sensation of heart during the palpitation episode. In the current admission baseline ECG and ECHO were normal, Holter done could not find any significant pauses, however TMT was found to be positive. so, he is planned for coronary angiogram.
On examination, he was normotensive and in sinus rhythm. On precordial auscultation, he had no cardiac murmurs or added sounds. Laboratory tests, including cardiac enzymes, were normal.
He underwent trans radial Coronary Angiography and Right Heart Catheterisation (Table 1) which showed Normal epicardial coronary arteries, and right coronary artery had a fistulous connection to Left pulmonary artery (Figure 1) with no PAH. He was advised for coil closure of RCA to LPA fistula if symptomatic for inducible ischemia (coronary steal).
| Saturation |
Aorta | 96% |
Pulmonary Artery | 68% |
IVC | 69% |
Right Atrium | 76% |
Right Ventricle | 66% |
SVC | 65% |
No step up noticed | |
Qp/Qs ratio = 1.07 | |
Table 1: Right Heart Catheterisation findings.
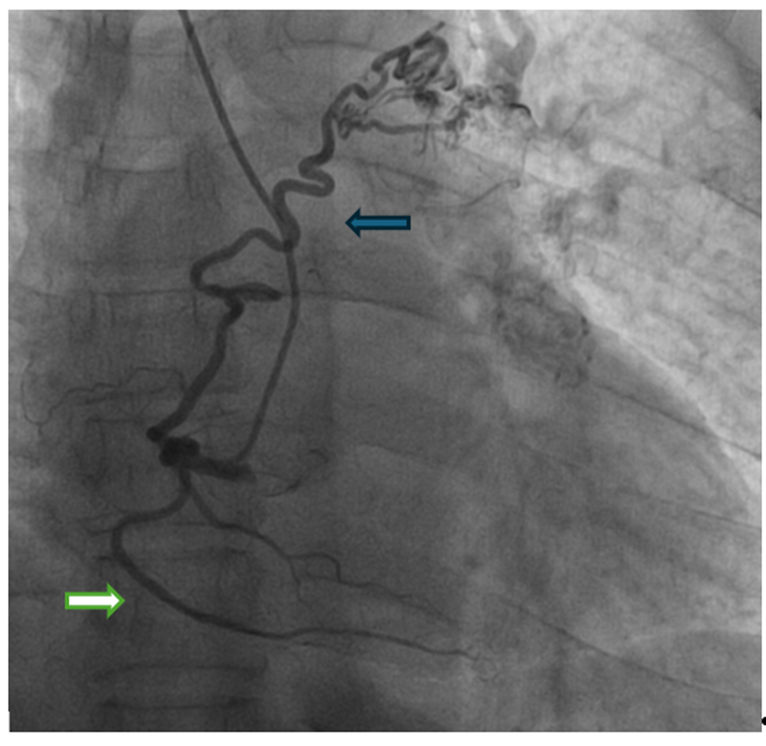
Figure 1: Coronary Angiography revealing right coronary artery (white arrow) had a fistulous connection to Left pulmonary artery (blue arrow).
Discussion
The incidence of coronary anomalies ranges from 0.6% to 1.5% among patients undergoing invasive cardiovascular imaging (1). Coronary artery fistulae (CAF) were first described in 1841 and are defined as abnormal connections between a coronary artery and a major blood vessel or cardiac chamber (2). The incidence of coronary artery fistulae in the general population is approximately 0.002%. Similarly, a study involving 11,000 patients undergoing cardiac catheterization reported the incidence of coronary pulmonary fistulas to be around 0.1% (3). CAF usually leads to blood shunting from left to right side of heart. The consequences of shunting in coronary artery fistulae can vary based on the volume of blood flow and may include pulmonary hypertension, rupture, and coronary steal phenomena. Additional complications can involve endocarditis, early atherosclerosis, hemopericardium, and myocardial ischemia (4).
Most patients with coronary artery fistulae (CAF) are asymptomatic, as they typically have small, insignificant shunts. However, the most common presenting symptom is angina, which may arise from coronary artery disease (CAD) or coronary steal phenomena in the absence of CAD. Other symptoms can include those associated with congestive heart failure, fistula rupture, and endocarditis. A classic physical finding in some cases of CAF is a continuous murmur. The main pathophysiological cause of ischemia in symptomatic patients with coronary-pulmonary artery fistulas (CPAFs) is coronary steal syndrome, where blood is diverted to a low-resistance area such as the pulmonary vessels, reducing blood flow to higher-resistance regions and resulting in ischemia. Electrocardiogram (EKG), echocardiography, cardiac stress testing, multidetector computed tomography (MDCT), and cardiac magnetic resonance imaging are the preferred non-invasive diagnostic tools for evaluating symptomatic patients with suspected coronary-pulmonary artery fistulas (CPAFs). However, coronary angiography remains the gold standard, offering precise anatomical details regarding the fistula’s size, origin, path, drainage site, and any coexisting coronary artery disease (CAD) (5). A myocardial perfusion scan is a useful diagnostic tool for patients with small coronary-pulmonary artery fistulas (CPAFs), helping to identify those who may benefit from either invasive intervention or conservative medical therapy. Myocardial perfusion positron emission tomography (PET) offers enhanced spatial resolution and sensitivity compared to SPECT imaging. When myocardial ischemia is limited, conservative treatment is often sufficient (6–8). There are no standardized guidelines for the management of coronary-pulmonary artery fistulas (CPAFs); however, treatment approaches typically depend on whether symptoms are present. According to the 2018 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for adult congenital heart disease, closure is recommended for all large coronary artery fistulas (CAFs), regardless of symptomatology (9). Similarly, closure is recommended for symptomatic patients even when the fistulas are small. For asymptomatic individuals, conservative management is appropriate, with follow-up echocardiography every three to five years to monitor changes in the size of the fistulas over time (10,11). Treatment options include medical therapy, surgical ligation, and transcatheter coil embolization. In patients with small CPAFs and minimal shunting, antianginal medications have been shown to improve symptoms. Although no comparative studies between transcatheter closure and surgical correction have been conducted, transcatheter closure is now the preferred treatment for patients with a proximal fistula origin, a single drainage site, and no other underlying cardiac conditions.(9) Surgical ligation is needed in patients with multiple drainage sites, distal fistula origin, tortuosity of the vessels, significant aneurysms, pulmonary-systemic flow ratio exceeding 1.5:1, and associated cardiac diseases (12).
Patients with CPAFs who undergo closure have an excellent prognosis; recurrence rates are as low as 9%-19% in transcatheter closure and 25% with surgical ligation. The prognosis depends upon the shunt's severity, associated complications, pulmonary hypertension, heart failure, and bacterial endocarditis (9).
Conclusion
Coronary-pulmonary artery fistulas (CPAFs) are an uncommon form of coronary artery fistulas (CAFs). In most cases, individuals with CPAFs show no symptoms and don't need targeted treatment. However, in younger patients and athletes, the risk of serious complications—such as irregular heart rhythms, heart attacks, or sudden cardiac death—makes early intervention important. Those who do experience symptoms often report repeated chest pain or arrhythmias. Because CPAFs are so rare, there are no established treatment guidelines that distinguish between managing symptomatic and asymptomatic cases. Though rare, CAFs may be an overlooked cause of angina or breathlessness linked to heart conditions. Once diagnosed, they should be closely monitored, and closure should be considered to avoid potential complications. Patients who undergo either catheter-based or surgical correction usually have a favourable outcome and can expect a normal life span.
References
- Kardos A, Babai L, Rudas L, Gaál T, Horváth T, Tálosi L, et al. Epidemiology of congenital coronary artery anomalies: a coronary arteriography study on a central European population. Cathet Cardiovasc Diagn. 1997 Nov;42(3):270–5.
View at Publisher | View at Google Scholar - Fernandes ED, Kadivar H, Hallman GL, Reul GJ, Ott DA, Cooley DA. Congenital malformations of the coronary arteries: the Texas Heart Institute experience. Ann Thorac Surg. 1992 Oct;54(4):732–40.
View at Publisher | View at Google Scholar - Said SA, Landman GH. Coronary-pulmonary fistula: long-term follow-up in operated and non-operated patients. Int J Cardiol. 1990 May;27(2):203–10.
View at Publisher | View at Google Scholar - Dadkhah-Tirani H, Salari A, Shafighnia S, Hosseini SF, Naghdipoor M. Coronary artery to pulmonary artery fistula. Am J Case Rep. 2013;14:486–8.
View at Publisher | View at Google Scholar - Coronary artery fistulas: How to manage them - Latson - 2007 - Catheterization and Cardiovascular Interventions - Wiley Online Library [Internet]. [cited 2025 May 17]. Available from: https://onlinelibrary.wiley.com/doi/10.1002/ccd.21125
View at Publisher | View at Google Scholar - Lee SK, Jung JI, O JH, Kim HW, Youn HJ. Coronary-to-pulmonary artery fistula in adults: Evaluation with thallium-201 myocardial perfusion SPECT. PLOS ONE. 2017 Dec 7;12(12):e0189269.
View at Publisher | View at Google Scholar - Saboo SS, Juan YH, Khandelwal A, George E, Steigner ML, Landzberg M, et al. MDCT of Congenital Coronary Artery Fistulas. Am J Roentgenol. 2014 Sep;203(3):W244–52.
View at Publisher | View at Google Scholar - Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation. 2007 Mar 1;115(10):1296–305.
View at Publisher | View at Google Scholar - Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019 Apr 2;73(12):1494–563.
View at Publisher | View at Google Scholar - Gowda RM, Vasavada BC, Khan IA. Coronary artery fistulas: Clinical and therapeutic considerations. Int J Cardiol. 2006 Feb 8;107(1):7–10.
View at Publisher | View at Google Scholar - Raju MG, Goyal SK, Punnam SR, Shah DO, Smith GF, Abela GS. Coronary artery fistula: A case series with review of the literature. J Cardiol. 2009 Jun 1;53(3):467–72.
View at Publisher | View at Google Scholar - Saeed A, Ghumman GM, Mir D, Khan AA, Sivarama K, Saeed A, et al. Left Coronary Artery to Pulmonary Trunk Fistula: Two Case Reports With Literature Review. Cureus [Internet]. 2023 Aug 17 [cited 2025 May 17];15. Available from: https://www.cureus.com/articles/167574-left-coronary-artery-to-pulmonary-trunk-fistula-two-case-reports-with-literature-review
View at Publisher | View at Google Scholar

 Clinic
Clinic
