Research Article | DOI: https://doi.org/10.31579/2835-8465/012
Comparison of the Effectiveness of the Minimally Invasive Approach with Preserved Piriformis Muscle with the Standard Posterolateral Approach in Total hip Arthroplasty
1 International Orthopedic Scientific Complex "Frank País"cuba.
2 Center for Research in Longevity, Aging and Health, "CITED"cuba.
*Corresponding Author: Horacio Tabares Neyra, Center for Research in Longevity, Aging and Health,
Citation: Tiemure Wu, Luis Oscar Marrero Riverón, Ricardo Jesús Tarragona Reinoso, Horacio Tabares Neyra, (2024), Comparison of The Effectiveness of The Piriformis-Sparing Minimally-Invasive Approach with The Standard Posterolateral Approach in Total Hip Arthroplasty, Orthopaedics Case Reports.3(2); DOI:10.31579/2835-8465/012
Copyright: ©, 2024, Horacio Tabares Neyra. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 12 March 2024 | Accepted: 20 March 2024 | Published: 29 March 2024
Keywords: Total hip arthroplasty; posterolateral approach; minimally invasive surgery; Mis-PLA
Abstract
Target:The purpose of this study is to determine if Mis-PLA is superior to the conventional technique in total hip arthroplasty.
methods:A prospective, randomized study was carried out where the sample constitutes 200 patients who underwent primary THA between September 2019 and March 2021 with a minimum follow-up of one year. Perioperative bleeding, postoperative pain, recovery time, component orientation, size, and fit, complication rate, and functional outcome were evaluated.
Results:No significant differences were found between the groups in terms of perioperative bleeding, operation time. The speed of recovery was significantly higher with the minimally invasive posterolateral approach, as an earlier onset of ambulation and a shorter hospitalization time were detected. In the Mis-PLA group, the acetabular components were more anteversion (p = 0.003), the size of the acetabular component and femoral head was smaller, the fitting technique was predominantly press-fit, the Visual Analogue Scale was significantly lower at 48 hours postoperatively. No differences were found in terms of complication rate or functional outcome at one year.
Introduction
Since it entered the field of orthopedics, total hip arthroplasty has become one of the most successful surgeries due to its good effect on diseases around the hip joint. [1-3]. In an early period of time, the focus of surgery was primarily on the design, material, and fixation of the prosthesis, but in recent decades more and more attention has been paid to the surgical approach [4].
The traditional posterolateral approach has a stable and good effect in hip arthroplasty, in the United States, the posterolateral (Moore/Southern) approach is the most common surgical approach for primary and revision total hip arthroplasty.5This approach provides excellent exposure of the proximal femur and acetabular anatomy, but also carries an increased risk of neurovascular injury and dislocation of the prosthesis [4,6].
Minimally invasive surgeries will become more frequent because their safety has been repeatedly demonstrated with different approaches [7,8]. The pressure for smaller incision surgery is coming from patients, and current studies suggest that patient satisfaction with minimally invasive surgery is high [9A]. small incision gives them more hope that the result they envision will be achieved. Patients want pain relief and they want to achieve their functional goals, but true satisfaction is not achieved without achieving their psychosocial goals, the most important of which is that they do not want to be self-conscious about their hip [10]. They want to regain control of their independence and activities, which their disability limits. Patients intuitively believe that the smaller incision will cause them less injury, allowing for a quicker recovery, they also correlate the smaller incision with less violation of their body, which means a better chance of full recovery. A more aesthetic wound is the objective reference for the subjective expectations of the patient.eleven
The minimally invasive posterolateral approach with preserved piriformis muscle (Piriformis-sparing minimally-invasive approach, Mis-PLA) is an approach rarely reported, according to the author's experience, so far very few articles can be found in Pubmed. In 2006, Khan et al. first reported Mis-PLA.12Compared to the traditional posterior approach, this approach shows a faster restoration of hip function. Biomechanical studies performed by Snijders et al. and Giphart et al [13.14]. demonstrated that the piriformis muscle is important for hip stability and function, and a Khan et al. randomized controlled trial of 89 cases further confirmed the superiority of this procedure in the early postoperative period.fifteenStudies have found that the function and stability of the hip joint is related to the piriformis muscle [16]. Therefore, the minimally invasive posterolateral approach with preserved piriformis muscle is an easy approach to proceed, beneficial for recovery of joint function, andfrequencydislocation is lower [15,17-19].
Despite the novelty of the previous studies mentioned, this study investigated the effectiveness of the minimally invasive posterolateral approach with preserved piriformis muscle and the posterolateral approach, in order to determine whether Mis-PLA is superior to the standard technique in total arthroplasty. Hip.
The aim of this study was to compare the results obtained using the Mis-PLA and standard posterolateral approaches in terms of perioperative bleeding, postoperative pain, speed of recovery, surgical time, orientation and adjustment of the implanted components,frequencyof complications and functional outcome.
Materials and methods
1.1 General aspects of the study
A prospective, randomized study was carried out where the sample constituted 200 patients who underwent primary uncemented CTA between September 2019 and March 2021 at the Beijing Jishuitan Hospital, with a one-year follow-up from the arthroplasty and who met the following inclusion criteria: 1 - Age over 18 years. 2 - Diagnosis of primary or secondary coxarthrosis such as congenital hip dysplasia, avascular necrosis of the hip, ankylosing spondylitis. The following were excluded from the study: 1- Patients with revision total hip arthroplasty. 2 - Patients with a history of epilepsy, mental retardation, hemiplegia or movement imbalance. 3 - Patients with a history of hip infections. 4 - Suffering from diseases that could seriously affect postoperative functional recovery, such as severe knee arthropathy and severe spinal disease. 5 - Patients with benign or malignant neoplasm of the hip joint. The patients were randomly divided into two groups of 100 patients. The patients were randomly divided into two groups of 100 patients.
1.2 Clinical data
The patients were randomly divided into a posterolateral approach group (standard group) and a minimally invasive posterolateral approach group with preserved piriformis muscle (Mis-PLA Group), there were 100 cases with 100 hips in the standard group, including 43 men and 57 women, and the age was (54.9 ± 11.6) years, among them, there were 31 cases with coxarthrosis, four cases with hip dysplasia, 62 cases with avascular necrosis of the femoral head, and three cases with ankylosing spondylitis. Mis-PLA group consisted of 100 cases with 100 hips, 48 men and 52 women, age (55.4 ± 13.2) years, 41 cases with coxarthrosis and 6 cases with hip dysplasia, 49 cases with avascular necrosis of the femoral head two cases with ankylosing spondylitis (Table 1).
1.3 Surgical methods
All surgeries were randomly performed by the same three physicians. The prostheses used were from DePuy Synthes (The Orthopedics Company of Johnson & Johnson, Warsaw, Indiana, United States).
Preoperative preparation:Complete blood count, urinalysis, blood chemistry, coagulogram, tests for sexually transmitted diseases, C-reactive protein, erythrocyte sedimentation rate, electrocardiogram, chest and pelvic x-ray, scan, cardiogram, lower limb angiogram, and pulmonary function test if applicable necessary (over 60 years). The patient's blood pressure was controlled at (120-135) / (80-90) mm Hg and blood glucose was controlled below 7.9 mmol/L prior to surgery. The skin was prepared, a urethral catheter was placed. The size of the prosthesis was measured according to anteroposterior radiographs of the affected hip. Spinal anesthesia was used, with intravenous infusion of second-generation cephalosporin antimicrobial drug (cefuroxime, 1.5g) 30 minutes before surgery,
1.3.1 Posterolateral approach
Patient in lateral decubitus on the unaffected side, followed by disinfection methods and draping. A 10-14 cm incision was made from the medial portion between the iliac crest and the tip of the greater trochanter in line with the femoral shaft to the distal end of the shaft.
The skin, subcutaneous tissue, and underlying fascia of the tensor fasciae latae were then incised plane by plane and a blunt dissection of the gluteus maximus was performed. The hip was then internally rotated to expose the piriformis muscle, the obturator internus muscle, the superior and inferior gastrocnemius muscles, and the quadratus thigh muscle. The muscle attachments were excised with an electric scalpel and the muscles folded upward to expose the joint capsule. Then, an inverted “T” shaped incision was made to open the joint capsule, the hip was dislocated, and the femoral neck was resected 1 cm above the lesser trochanter. The femoral head was then recovered using a special appliance with the femoral neck trimmed.
After cleaning the acetabular margin, the femoral head ligament was excised and residual soft tissues in the femoral head area were cleaned to expose the bony acetabulum. Trial acetabular prostheses of different sizes were placed to determine the ideal fit and bone coverage. An appropriate prosthesis was selected and placed in the acetabular cup in the position of 45° abduction and 15° anteversion, using screws for fixation if necessary. The affected limb was supported and adducted as much as possible. The proximal end of the femur was slotted and reamed to obtain the ideal size and the trial cast was placed. Lower leg length, range of motion, and hip stability were examined. The final prosthesis was placed for its reduction. A “mixed solution” was injected locally and the soft tissues sutured.
1.3.2 My-PLA
In the Mis-PLA group, after spinal anesthesia, the patient was placed in lateral decubitus on the unaffected side and a disinfection method was performed. A 7-9 cm incision was made from the medial portion between the iliac crest and the tip of the greater trochanter in line with the femoral shaft to the distal end of the shaft.
Next, the subcutaneous tissue and the underlying fascia of the tensor fasciae lata were incised, the sciatic nerve and gluteus medius were protected, and the special retractor was used to retract the piriformis muscle upwards (Fig. 1), they were resected. the quadratus muscle, the superior gastrocnemius muscle, the obturator internus muscle, and the inferior gastrocnemius muscle. A vertical "L" shaped incision was made in the joint capsule. The tendon of the piriformis muscle and the posterior superior joint capsule were preserved. (Fig.2) A hip dislocation was then performed using internal rotation, hip flexion, and knee flexion.
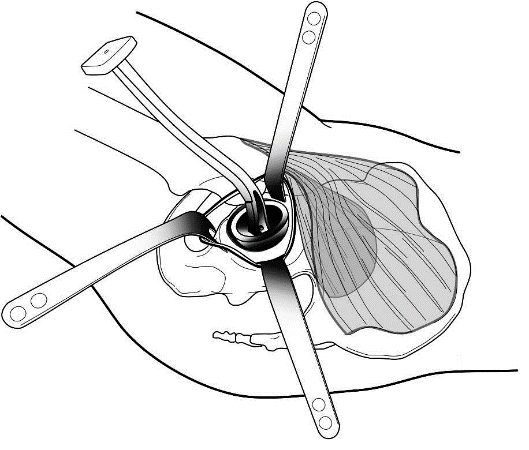
Figure1: the special retractor was used to retract the piriformis muscle upwards
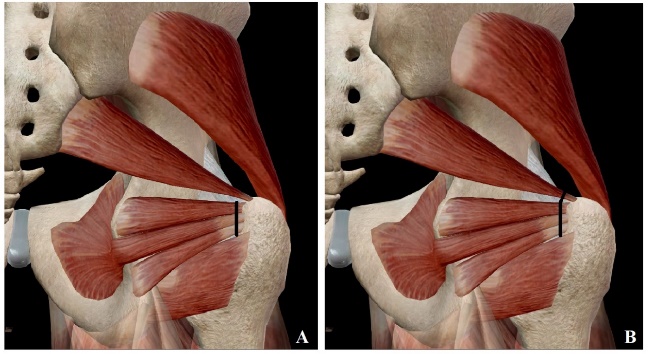
Figure2: A hip dislocation was then performed using internal rotation, hip flexion, and knee flexion.
Femoral neck osteotomy was performed, and the femoral head was recovered with a special apparatus. The soft tissues of the acetabular socket and round ligament were resected, and the acetabular margin was cleaned to expose the bony acetabulum. Trial acetabular prostheses were implanted to determine ideal compatibility. An appropriate prosthesis was selected and placed in the acetabular cup and screws were used for fixation, if necessary.
The affected limb was held and adducted as much as possible, the proximal end of the femur was reamed to obtain the ideal size. Then, the test cast was placed. Both lower limb length, range of motion, and hip stability were examined. The mixed solution was injected locally, the soft tissue around the bottom of the acetabulum was sutured. It was closed by plans. (Fig. 3)
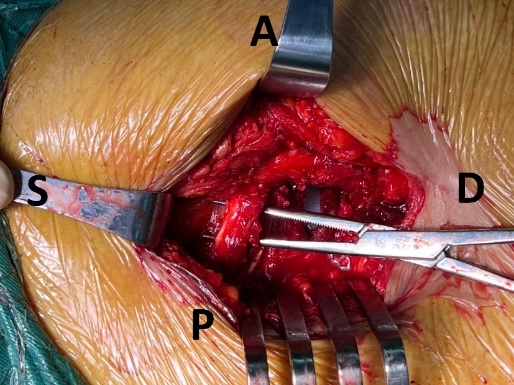
Figure3: the soft tissue around the bottom of the acetabulum was sutured
Postoperative treatment, for both groups: General treatment: Both groups received analgesic pump for pain relief within 24 hours after the operation, and then switched to oxycodone and acetaminophen tablets(5mg+325mg) orally every day for one week after 24 hours with a dose of one tablet every 6 or 8 hours. Antibiotics were administered intravenously within 24 hours after surgery. Mis-PLA group: the affected limb was kept in a neutral position with slight abduction, and a pad was placed between the two legs to prevent adduction and internal rotation of the hip.
1.4 Data collection and monitoring
A Primary Data Collection Model (MPRD) was designed where the data provided in the interrogation and all the examinations performed on the patient in the pre, trans and postoperative period were collected. Harris Hip Score (HHS) and pain severity were assessed at preoperative visits. In the transoperative period, the measurement of surgical time, perioperative bleeding, and the size of the acetabular components and the femoral head were taken into account. In the postoperative period, pain was evaluated using the Visual Analogue Scale (VAS) at 48 hours and 12 months, speed of recovery, orientation of the acetabular component, frequency of complications, and the postoperative Harris Hip Score. the 12 months.
1.5 Statistical analysis
The SPSS 25.0 program (IBM, Armonk, NY, USA) was used for statistical analysis. The Kolmogorov-Smirnov test verified the normality of continuous variables. Normally distributed continuous data from the two groups were analyzed using the t-test. For continuous data that were not normally distributed, the Mann-Whitney U Test was performed. To determine the association of qualitative variables, the Chi square test (χ2) was used. To determine the association of qualitative variables, Fisher's exact test was used in the case of expected frequencies less than 5. Primary follow-up results such as VAS were analyzed using repeated measures analysis of variance (ANOVA). P < 0>
Results
In the present study, 200 patients with hip arthropathy who underwent THA were analyzed using different approaches, the sample was divided into two groups according to the approach modality. The control group underwent a posterolateral approach and the Mis-PLA study group, each consisting of 100 hips from 100 patients.
The value of the average age was 54.9 ± 11.6 years and the patients with the left side that occupies 52.0% in those treated with the classic posterolateral approach predominated. In the group treated with Mis-PLA, the mean age value was 55.4 ± 13.2 years and the right side predominated, occupying 52.0%. There was no significant difference in the mean age between the two treatment groups. Regarding BMI, the mean value in the standard group was20.7 ± 3.7, and to the Mis-PLA group: 20.6 ± 3.2. When comparing both groups, no significant difference was observed.
In both groups there was a predominance of female patients. In the group of patients treated with the standard posterolateral approach, these represented 57.0%, and in those treated with Mis-PLA, 52.0%. When comparing both groups, no significant difference was observed.
Regarding the preoperative diagnosis for the standard group, avascular necrosis of the hip represents the main cause that occupies 62.0%, coxarthrosis (31.0%), congenital dysplasia of the hip (4.0%), spondylitis ankylosing (3.0%). This is similar in the Mis-PLA group, with a predominance of hip avascular necrosis (52.0%), coxarthrosis (40.0%), decisive congenital dysplasia (6.0%) and ankylosing spondylitis. (2.0%). According toAmerican Society of Anesthesiologist Physical Status (ASA) classification, the two groups present a similar distribution: group one at 61.0%, group two at 31.0% and group three at 2.0% in the standard group, group one at 65 0.0%, group two at 32.0% and group three at 3.0% in the Mis-PLA group. When comparing both groups, no significant difference was observed.
Variable | Statistics/Categories | standard group | Mis-PLA Group | p |
Age | Half of | 54.9 ± 11.6 | 55.4 ± 13.2 | 0.755* |
Sex | Male (N/%) | 43/43,0 | 48/48,0 | 0.478** |
Female (N/%) | 57/57,0 | 52/52,0 | ||
BMI | Half of | 20.7 ± 3.7 | 20.6 ± 3.2 | 0.959* |
Side | Left (N/%) | 52/52,0 | 48/48,0 | 0.572** |
Right (N/%) | 48/48,0 | 52/52,0 | ||
Prooperative diagnosis | Congenital hip dysplasia (N/%) | 4/4,0 | 6/6,0 | 0.454*** |
Avascular necrosis of the hip (N/%) | 62/62,0 | 52/52,0 | ||
Coxarthrosis (N/%) | 31/31,0 | 40/40,0 | ||
Ankylosing spondylitis (N/%) | 3/3,0 | 2/2,0 | ||
HANDLE | 1 (N/%) | 61/61,0 | 65/65,0 | 0.708*** |
2 (N/%) | 37/37,0 | 32/32,0 | ||
3 (N/%) | 2/2,0 | 3/3,0 |
Source: Clinical History. BMI: Body Mass Index; ASA: American Society of Anesthesiologists Scale; SD: standard deviation; N: number of patients; p*: independent sample t-test; p**: Chi square test; p***: Fisher's exact test;
Table 1. Exposure and comparison of the preoperative variables of both groups.
The exposure and comparison of the intraoperative and postoperative variables of both groups is presented in Table 2. The size of the acetabular component for Mis-PLA (49.8 ± 3mm) was smaller than for the standard group (52.3 ± 3.7mm). ) (p < 0 xss=removed>
Regarding the prosthesis position, the anteversion angle showed a significant difference in both groups. It was noticed that the Mis-PLA group presents a significantly higher degree of anteversion than the standard group (P = 0.020, Mann-Whitney U test). . The median grade was 17.4 (range 25-75%, 12.7-23.1) in the standard group and 21.6 (range 25-75%, 14.9-23.4) in the Mis-PLA group (Table 2, Fig.4). But regarding the abduction angle, the difference was not significant (p = 0.515).
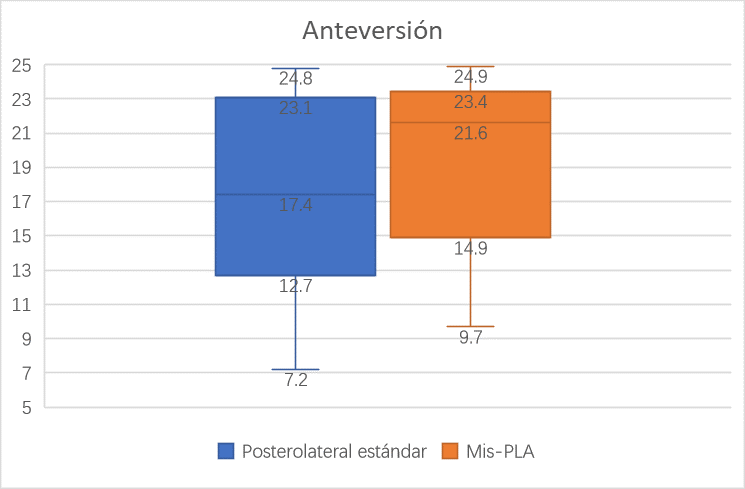
Figure 4: regarding the abduction angle, the difference was not significant
In the postoperative period, as can be seen in Table 3, the start of ambulation (day on which the patients were able to walk 10 continuous steps) was significantly better in the group of patients operated on using a minimally invasive approach (3.1 ± 2 .1) than the group with the classic posterolateral approach (3.9 ± 1.8) (p = 0.042). Hospitalization time (days) was significantly longer in the standard group (3.9 ± 0.9) than in the Mis-PLA group (3.3 ± 0.5) (p < 0 xss=removed xss=removed xss=removed>
Regarding complications, the following complications occurred in the standard group: one case of dislocation after epileptic seizures and it was reduced under anesthesia, one case of hip bursitis that was alleviated when receiving conservative treatment. On the other hand, in the group of patients who underwent surgery using the Mis-PLA approach, a case was detected with hip dislocation after a fall, which was resolved conservatively without recurrence, one case suffered from sciatic pain that was controlled with analgesics and other conservative treatments, one case also suffered hip bursitis is improving at last moment to investigation by conservative treatment. After analyzing these data, no significant difference was found (p = 0.659).
Variable | Statistics/Categories | standard group | Mis-PLA Group | p | |
Operation time(min) | Half of | 73 ± 23.6 | 67.9 ± 30.1 | 0.221* | |
Intraoperative bleeding (mL) | Half of | 166.4 ± 92.7 | 156.5 ± 58.7 | 0.423* | |
Anteversion Angle (Degree) | Median (p25-p75) | 17.4 /12.7-23.1) | 21.6/14.9-23.4) | 0.020** | |
Abduction Angle/Degree) | Median (p25-p75)) | 41.9 /36.4-46.4) | 40.1 /37.2-43.3) | 0.515** | |
Acetabular component size (mm) | Half of | 52.3 ± 3.7 | 49.8 ± 3 | <0> | |
|
|
|
|
| |
Femoral Head Component Size (mm) | Half of | 34.5 ± 2.8 | 33.3 ± 2.8 | 0.005* | |
Acetabular component adjustment techniques | Pressure fit (N/%) | 25/25,0 | 66/66,0 | <0> | |
Screw adjustment (N/%) | 75/75,0 | 34/34,0 | |||
No, of Screws | Half of | 1.86 ± 0.42 | 1.81 ± 0.49 | 0.652* | |
Postoperative |
| ||||
Walking time (days) | Half of | 3.9 ± 1.8 | 3.1 ± 2.1 | 0.042* | |
Hospitalization time (days) | Half of | 3.9 ± 0.9 | 3.3 ± 0.5 | <0> | |
complications | Dislocation (N/%) | 1/1,0 | 1/1,0 | 0.553**** | |
Nerve injury or sciatic pain (N/%) | 0/0,0 | 1/1,0 | |||
Hip bursitis (N/%) | 1/1,0 | 1/1,0 | |||
SD: standard deviation; N: number of patients; p*: independent sample t-test; p**: Mann-Whitney U test; p***: Chi-square test; p**** Fisher's exact test.
Table 2 Exposure and comparison of the intraoperative and postoperative variables of both groups.
Table 3. In the evaluation of the functional result, the pre-surgical HHS was used and 12 months after the surgical intervention, a great improvement in joint function was observed, no difference was found between the two groups after 12 months. Regarding the VAS score, pain relief is observed in 48 hours and 12 months compared to the preoperative assessment. Regarding the intergroup comparison, it shows better pain relief in 48 postoperative hours in the Mis-PLA group (p < 0>
variables | Statistics/Categories | standard group | Mis-PLA Group | p* |
Harris Score | ||||
Pre. | Half of | 59.0 ± 19.7 | 56.1 ± 17.5 | 0.264 |
Post to 12 months | Half of | 90 ± 8.7 | 90.2 ± 10.0 | 0.906 |
| p** | <0> | <0> | - |
VAS score | ||||
Pre. | Half of | 7.1 ± 1.7 | 7.3 ± 1.8 | 0.449 |
Post 48 hours | Half of | 3.0 ± 0.8 | 2.4 ± 1.0 | <0> |
|
|
|
|
|
Post to 12 months | Half of | 0.6 ± 1.3 | 0.8 ± 1.2 | 0.125 |
p*** | <0> | <0> | - | |
SD: standard deviation; N: number of patients; p*: independent sample t-test; p**: Paired sample t-test; p***: Analysis of variance (ANOVA) with repeated measures (MR), two-way ANOVA. Pre: Preoperative. Pos: Postoperative
Table 3, Comparison of hip joint functions between two groups
Discussion
Total hip arthroplasty is one of the most successful surgical procedures for relieving hip pain and improving quality of life and has been called "the operation of the 20th century." Despite this success, early and late complications have been reported, and dislocation remains one of the most common early complications after THA.
Historically, the posterior approach has been associated with a higher risk of dislocation compared to a lateral or anterior approach. Careful reconstruction of the capsule and short external rotators may decrease the risk of postoperative dislocation. Kwon et al performed a meta-analysis to determine thefrequencyof dislocations using a posterior approach with and without posterior soft tissue repair and found an eight-fold increased relative risk of dislocation when soft tissue repair was not performed.twenty
The rotator muscles are important for the stability of the hip joint, Roche et al.16 in their study of cadavers, they report that the piriformis muscle seems to act as a posterior stabilizer of the joint in 90° flexion and, therefore, leaving the tendon intact may decrease the risk of dislocation and should not compromise access to the intramedullary canal through of the posterior approach in ATC. In a two-year study by Khan et al., twenty-onein patients receiving CTA through the standard posterolateral approach and Mis-PLA, who underwent magnetic resonance imaging three months and two years after surgery to determine the degree of deterioration of the piriformis muscle. The study determines that patients who undergo THA with the Mis-PLA approach have much less muscle deterioration, therefore, they conclude that the Mis-PLA approach damages the piriformis muscle less compared to the standard posterolateral approach. However, the cadaveric study carried out by Amanatullah et al. demonstrates, during the THA procedure using the Mis-PLA approach, the soft tissue damage that occurs outside the surgical field during the retraction of the unreleased muscles, such as the muscle piriformis is common, it is considered as an uncontrolled surgical variable.22Amanatullah's assessment22is in human cadavers, while the study by Khan et al.twenty-oneTHA is performed on living patients, therefore there are obvious differences in muscle physiology with respect to the strength and laxity of the piriformis muscle during each procedure.
In this study, age, sex, BMI, side, operation time, bleeding did not present a significant difference. According to the study by Roche et al., the confusion between the trochanteric fossa and the piriformis fossa is what has led to the misunderstanding regarding the insertion of the piriformis tendon, and the erroneous opinion that adequate access for CTA is not possible without resection. the piriformis tendon.16Actually, when comparing the Mis-PLA approach with the posterolateral approach, the surgical procedures are similar, so it is considered an easy technique to familiarize with and the learning curve is shorter, special retractors with long handles that form a 90° angle with the blade. These instruments keep the assistants' hands off the field and place less stress on the soft tissues. In an unusual situation, without the use of special instruments, the purpose can also be achieved by placing a sharp Hohmann retractor under the posterior border of the gluteus medius and proximal to the piriformis tendon, which can be easily identified under visualization or by palpation. Therefore, for an experienced surgeon, the cost of time and perioperative bleeding may not make much of a difference. A similar result is also reported by Varela et al [17].
In the prosthesis position, the anteversion angle comparison presents a significant difference and is larger in the Mis-PLA group. The converse was not found in the abduction angle comparison. However, in both groups the mean positions of the components were within the Lewinnek safe zone.23. In the work of Khan et al, it is reported that the acetabular components were less anteverted and had a lower mean angle of inclination in the Mis-PLA group. On the contrary, the study by Wang et al. demonstrates in their study that no significant difference was found in the angle of abduction or anteversions.24The author considers that due to the different technical details of the surgical operation and the different surgical tools, there may be some differences in the results, the most important being that they are within the Lewinnek safe zone.
When comparing the size of the acetabular component and the femoral head component, it is observed that the size of the prosthesis was significantly reduced in the Mis-PLA group. The author wants to argue that the patients are randomly distributed, and by this division, by chance, the size of the components is smaller in the Mis-PLA group. Regarding the adjustment techniques of acetabular components, the Mis-PLA group prefers pressure adjustment over screws. The authors of this research consider that the reduced surgical field affects the surgeon's decision to some extent.
In the present investigation, the authors did not find significant differences in the functional result 12 months after surgery, having assessed the Harris Hip Score and VAS, but the VAS score at 48 postoperative hours was significantly lower in the group My-PLA. Although there are authors who demonstrate a better functional result, such as Wang et al., they reported that at three postoperative weeks a significant improvement is observed in hip functional assessment, but at eight weeks they found no significant difference.24Varela et al. made a comparison in three months and 12 months and did not find a significant difference either.17The study by Brady et al. with a 10-year follow-up concluded that the Mis-PLA approach offered the same long-term functional benefits as the standard posterolateral approach. Therefore, the authors of this study consider that this procedure does not provide significant functional improvement in the long term [15,25,26]. but it is beneficial for the short term. This short-term effect is also observed in walking time, and hospitalization time, which were significantly better in the group of patients operated using a minimally invasive approach. The authors of this research believe that the less soft tissue damage, the faster the patient's recovery after surgery. Similar results are also reported by Varela et al. and Wang et al [17.24].
As stated in the results chapter, no significant differences were found in thefrequencynone of the complications found between the Mis-PLA and conventional approaches. None of the surveyed studies detected a greaterfrequencyof complications with Mis-PLA surgery [15,17,24,27].
Conclusion
The use of the minimally invasive posterior approach when performing primary total hip arthroplasty has been able to accelerate early recovery, decrease hospitalization time, and alleviate early postoperative pain compared to the standard posterolateral approach without compromising surgical time, surgical bleeding., nor increase thefrequencyof complications, with a similar functional result in both approaches when evaluating the patients at 12 weeks.
References
- Graves SE, de Steiger R, Davidson D, Donnelly W, Rainbird S, Lorimer MF, et al. (2017). The use of femoral stems with exchangeable necks in primary total hip arthroplasty increases the rate of revision. Bone Joint J. [Access: 11/25/2022]; 99-(6):766-773.
View at Publisher | View at Google Scholar - Markatos K, Savvidou OD, Foteinou A, Kosmadaki S, Trikoupis I, Goumenos SD, et al. (2020). Hallmarks in the history and development of total hip arthroplasty. Surg Innov. [Access: 11/25/2022]; 27(6): 691-694.
View at Publisher | View at Google Scholar - Meek R, Treacy R, Manktelow A, Timperley JA, Haddad FS. (2020). Sport after total hip arthroplasty: progress undoubted but still some unknowns. Bone Joint J. [Access: 11/25/2022]; 102-B (6): 661-663.
View at Publisher | View at Google Scholar - Aggarwal VK, Iorio R, Zuckerman JD, Long WJ. (2020). Surgical approaches for primary total hip arthroplasty from charnley to now: the quest for the best approach. JBJS Rev. [Access: 11/25/2022]; 8(1):58.
View at Publisher | View at Google Scholar - Khanduja V. (2017). Total hip arthroplasty in 2017 - current concepts and recent advances. Indian J Orthop. [Access: 11/25/2022]; 51(4): 357-358.
View at Publisher | View at Google Scholar - Ries MD. Relationship between functional anatomy of the hip and surgical approaches in total hip arthroplasty. Orthopedics. 2019 [Access: 11/25/2022]; 42(4): 356-363.
View at Publisher | View at Google Scholar - Xiao C, Gao Z, Zhang S, Long N, Yao K, Cai P, et al. (2021). Comparative prospective randomized study of minimally invasive transpiriformis approach versus conventional posterolateral approach in total hip arthroplasty as measured by biology markers. Int Orthop. 2021 [Access: 11/25/2022]; 45(7): 1707-1717.
View at Publisher | View at Google Scholar - Kolodziej L, Bohatyrewicz A, Jurewicz A, Szczypior-Piasecka K, Przybyl K. (2020). Simultaneous bilateral minimally invasive direct anterior approach total hip arthroplasty with fast-track protocol. Ortop Traumatol Rehabil. [Access: 11/25/2022]; 22(1):17-24.
View at Publisher | View at Google Scholar - Vuckovic M, Ruzic L, Tudor A, Sutic I. (2021). Difference in patient quality of life after hip arthroplasty with a minimally invasive approach or classic approach. Clin Croat Act. 2021 [Access: 11/25/2022]; 60(1):89-95.
View at Publisher | View at Google Scholar - Hudak PL, Mckeever PD, Wright JG. (2004). Understanding the meaning of satisfaction with treatment outcome. Medical Care. [Access: 11/25/2022]; 42(8):718-725.
View at Publisher | View at Google Scholar - Dorr LD, Thomas D, Long WT, Polatin PB, Sirianni LE. (2007). Psychological reasons for patients preferring minimally invasive total hip arthroplasty. Clin Orthop Report Res. 2007 [Access: 11/25/2022]; 458:94-100.
View at Publisher | View at Google Scholar - Khan RJ, Fick D, Khoo P, Yao F, Nivbrant B, Wood D. (2006). Less invasive total hip arthroplasty: description of a new technique. J Arthroplasty. [Access: 11/25/2022]; 21(7):1038-1046.
View at Publisher | View at Google Scholar - Snijders CJ, Hermans PF, Kleinrensink GJ. (2006). Functional aspects of cross-legged sitting with special attention to piriformis muscles and sacroiliac joints. Clin Biomech (Bristol, Avon). 2006 [Access: 11/25/2022]; 21(2):116-121.
View at Publisher | View at Google Scholar - Giphart JE, Stull JD, Laprade RF, Wahoff MS, Philippon MJ. (2012). Recruitment and activity of the pectineus and piriformis muscles during hip rehabilitation exercises: an electromyography study. Am J Sports Med. 2012 [Access: 11/25/2022]; 40(7):1654-1663.
View at Publisher | View at Google Scholar - Khan RJ, Maor D, Hofmann M, Haebich S. (2012). A comparison of a less invasive piriformis-sparing approach versus the standard posterior approach to the hip: a randomized controlled trial. J Bone Joint Surg Br. [Access: 11/25/2022]; 94(1):43-50.
View at Publisher | View at Google Scholar - Roche JJ, Jones CD, Khan RJ, Yates PJ. (2013). The surgical anatomy of the piriformis tendon, with particular reference to total hip replacement: a cadaver study. Bone Joint J. [Access: 11/25/2022]; 95-B (6):764-769.
View at Publisher | View at Google Scholar - Varela EJ, Suarez-Suarez MA, Fernandez-Villan M, Gonzalez-Sastre V, Varela-Gomez J, Murcia-Mazon A. (2010). [Minimally invasive posterior approach in total hip arthroplasty. Prospective randomized trial]. An Sist Sanit Navar. [Access: 11/25/2022]; 33(2):133-143.
View at Publisher | View at Google Scholar - Tan B, Khan R, Haebich SJ, Maor D, Blake EL, Breidahl WH. (2019). Piriformis-sparing minimally invasive versus the standard posterior approach for total hip arthroplasty: a 10-year follow-up of a randomized control trial. J Arthroplasty. 2019 [Access: 11/25/2022]; 34(2):319-326.
View at Publisher | View at Google Scholar - Siddappa VH, Meftah M. (2020). Piriformis-sparing technique in total hip arthroplasty with posterolateral approach. Surg Technol Int. 2020 [Access: 11/25/2022]; 3:360-363.
View at Publisher | View at Google Scholar - Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ. (2006). Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Report Res. 2006 [Access: 11/25/2022]; 447:34-38.
View at Publisher | View at Google Scholar - Khan RJ, Lam LO, Breidahl W, Blakeney WG. (2012). Magnetic resonance imaging features of preserved vs divided and repaired piriformis during total hip arthroplasty: a randomized controlled trial. J Arthroplasty. 2012 [Access: 11/25/2022]; 27(4):551-558.
View at Publisher | View at Google Scholar - Amanatullah DF, Shah HN, Barrett AA, Storaci HW. A small amount of retraction force results in inadvertent piriformis muscle damage during a piriformis-sparing approach to the hip. J Bone Joint Surg Am. 2020 [Access: 11/25/2022]; 102(19):1687-1693.
View at Publisher | View at Google Scholar - Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978 [Access: 11/25/2022]; 60(2):217-220.
View at Publisher | View at Google Scholar - Wang T, Zhou Y, Li X, Gao S, Yang Q. (2021). Comparison of postoperative effectiveness of less invasive short external rotator sparing approach versus standard posterior approach for total hip arthroplasty. J Orthop Surg Res. [Access: 11/25/2022]; 16(1):46.
View at Publisher | View at Google Scholar - Herrera A. (2006). Effectiveness of minimally invasive surgery with a single posterolateral incision in total hip arthroplasty. [Access: 11/25/2022].
View at Publisher | View at Google Scholar - Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. (2007). Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. A prospective, randomized, blinded study. J Bone Joint Surg Am. 2007 [Access: 11/25/2022]; 89(6):1153-1160.
View at Publisher | View at Google Scholar - Aggarwal VK, Elbuluk A, Dundon J, Herrero C, Hernandez C, Vigdorchik JM, et al. (2019). Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Joint J. 2019 [Access: 11/25/2022]; 101- (6): 646-651.
View at Publisher | View at Google Scholar

 Clinic
Clinic
