Research Article | DOI: https://doi.org/10.31579/2835-835X/061
Comparison of Factors Associated with Stillbirth Delivery in a Tertiary and Primary Health Facility in Rivers State, Nigeria
- Foluke Olukemi Adeniji * *
- Ndudim Oluchi Mildred
Department of Preventive and Social Medicine, Faculty of Clinical Sciences, College of Health Sciences, University of Port Harcourt, Port Harcourt, Rivers State, Nigeria.
*Corresponding Author: Foluke Olukemi Adeniji, Department of Preventive and Social Medicine, Faculty of Clinical Sciences, College of Health Sciences, University of Port Harcourt, Port Harcourt, Rivers State, Nigeria.
Citation: Foluke O Adeniji, and Ndudim O Mildred, (2024), Comparison of Factors Associated with Stillbirth Delivery in a Tertiary and Primary Health Facility in Rivers State, Nigeria, Clinical Trials and Case Studies, 3(2); DOI:10.31579/2835-835X/061
Copyright: © 2024, Foluke Olukemi Adeniji. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 29 February 2024 | Accepted: 08 March 2024 | Published: 18 March 2024
Keywords: associated factors of stillbirth; RSUTH; OCH; port harcourt; ante-natal care
Abstract
Background: Globally, policies, program, and investment goals lack coverage of stillbirth, which accounts approximately a half of all mortality during pregnancy. Its detrimental effect on public health, especially in developing nations, has been understated. Nigeria is one of the nations in the world with the greatest incidence of stillbirth. The aim of the study was to identify and compare the associated factors of stillbirth amongst women attending two hospitals in Port Harcourt.
Materials and Methods: This comparative study identified and compared the types, and associated factors of stillbirth amongst women delivering at two hospitals in Port Harcourt. The study adopted a descriptive cross-sectional hospital-based study of all deliveries in a Obio Cottage Hospital (OCH) and Rivers State University Teaching hospital (RSUTH) within a 5-year period. A total population sampling method was adopted using a data extraction tool to obtain data for the study and analyzed using SPSS version 24.0.
Results: A total of 1253 stillbirth cases were obtained. The study showed stillbirth types, use, number and initiation of ANC, booked status and birth order as associated factors of stillbirth. There was more macerated case in OCH compared to RSUTH (ꭓ2=15.440; p<0.001). The use of at least one Ante Natal Care (ANC) in OCH as against RSUTH by delivering mothers was statistically significant (ꭓ2=13.924, p<0.001). Focused ANC in OCH compared to that in RSUTH was statistically significant (ꭓ2=16.194; p<0.001). Ninety-three (64.1%) of mothers in OCH initiated ANC early, 48 (33.1%) initiated intermediate and 4 (2.8%) initiated late, whereas 433 (57.2%) of those in RSUTH initiated ANC early, 212 (28.0%) initiated intermediate and 112 (14.8%) initiated late, and this difference was statistically significant (ꭓ2=15.811; p<0.001). More mothers booked for ANC in OCH than in RSUTH compared (ꭓ2=28.647; p<0.001).
Conclusion: Factors associated with stillbirth delivery in the 2 health facilities may reflect the underlying causes. In spite of access to ANC mothers seem to have a poor health seeking behaviour and delays in seeking care needs to be addressed. Interventions such as community-based health insurance scheme likely increased the utilization and attendance of antenatal care (ANC).
Introduction
One of the most underreported tragedies in modern world health is stillbirths, which accounts for approximately 2.6 million deaths annually, 98% of which take place in nations with low- and middle-incomes, [1] with Nigeria, contributing 12% of these cases [2]. Preventable diseases are often the cause of around half of stillbirths that occur after childbirth [3]. Nigeria declared a 15% increase in stillbirths between 2000 and 2009 according to a study by [4], Nigeria was predicted to have 313,700 Stillbirths (SB) in 2015, placing it in the second position globally. The total number of stillbirths in Nigeria in 2019 was 171,428 according to [5]. Surveys carried out around the nation reveal that stillbirth rates in Nigeria range from 39.9 per 1000 births to 180 per 1000 births [2]. According to a study conducted at the University of Port Harcourt Teaching Hospital, there were 45 stillbirths for every 1000 live births in Rivers State [6]. With a population of around 178 million in 2014, Nigeria has financial, cultural, behavioral, and environmental barriers to accessing inexpensive healthcare [7]. According to Lawn et al. [8], there are two types of stillbirths: fresh and macerated. Macerated stillbirths are alternatively expected to have occurred before labour (prepartum) but after 28 weeks of gestation; the death-to-delivery interval is longer and the foetus exhibits skin and soft tissue changes (skin discoloration or obscuring, redness, stripping, and breakdown), all of which are absent in fresh stillbirths. Fresh stillbirths are thought to have a short demise-to-delivery stretch and the death most likely occurred during labour (intrapartum death), the fetus must also be 28 weeks of gestation and above [8, 9]. In addition, earlier studies claimed that the differences between the two groups went beyond outward appearance; new stillbirths are thought to be more preventable as they usually happen during labour, in term pregnancies, and generally do not involve foetal abnormalities [9].While the high rate of perinatal mortality in many parts of Nigeria and indeed other developing countries is worsening due to several unfavourable factors, including high out-of-pocket payments as a result of no organized, functional national health insurance scheme, the decline in perinatal mortality in Western countries has been principally attributed to the health insurance schemes put in place by the government to reduce out-of-pocket payments. It has resulted in more people seeking healthcare services, as seen in the UK [10]. As a result of the high expense of living and poverty in developing countries which includes Nigeria, it is challenging for the vast majority of women to seek proper health care. Stillbirth is a condition of public health importance because its rates are still high and continuing to rise in various parts of the country. Nonetheless, the inappropriately high stillbirth rates that tend to occur in the country could be mitigated with coordinated efforts conducted at the federal, state, local, and individual levels [11]. In terms of limited resources, about 50% of the population pays for healthcare out-of-pocket (OOP). This has led to the recognition of financial incapacity as the main obstacle to care [12]. According to WHO, [13] the majority of women in Port Harcourt who are of reproductive age are either farmers, traders, students, employed, self-employed, or not employed. They may also engage in a variety of health-seeking behaviours to monitor and identify potential risks during pregnancy, which may result in complications like stillbirth or even maternal death. Since women with complications are typically referred to secondary and tertiary care facilities that offer comprehensive emergency obstetric care, referral health hospitals which are less expensive than private specialty ones become the last resort for miracles in the face of these complications and life-threatening situations [14]. However, the majority of people who cannot afford the bills in these referral facilities are often unable to access effective health insurance schemes. This discourages these mothers from seeking care, as they would rather use more easily accessible and less expensive healthcare facilities [13].Multiple studies on stillbirth that have separately accessed these healthcare levels have been conducted in Nigeria and developed nations. Nonetheless, the purpose of the research is to compare the types of stillbirths and its associated factors among women in their reproductive years who give birth at Port Harcourt's Obio Cottage Hospital (OCH), a primary health facility and Rivers State University Teaching Hospital (RSUTH) a tertiary health facility.
Materials and Methods:
Two health facilities a primary health facility, Obio Cottage Hospital (OCH), and Rivers State University Teaching Hospital (RSUTH) a tertiary health facility was randomly selected. Using estimates of the 2006 National Population Commission figures, the State has a population of 5,522,575. Rivers State has an area of approximately 37,000 square kilometers [15]. Maternity and healthcare services in the state are provided at primary, secondary, and tertiary levels.Obio Cottage Hospital (OCH) was founded in 1978 by the Rivers State government. It kicked off as a primary health centre (PHC) offering preventive and curative health care services to mostly indigenes of Obio/Akpor LGA. After two decades or more, Shell Petroleum Development Company (SPDC) began aiding the hospital as a form of its social infrastructure programme. SPDC enhanced and reconstructed the facility remodeling the 4-bed health care centre running on a small twin bungalow structure with 13 staff, to a facility having more than 58 beds and more than 100 staff. Every month, it has approximately a total of 2500 antenatal visits, having about 400 booked and a delivery proportion of about 300. These consistent modifications from what it used to be to its current state probably made the facility to be rated as a secondary health facility according to the study carried out by Okonta et al.[16] despite still being called a cottage hospital. As a result of SPDC's massive reconstruction and reforms, several services became available. By 2010, SPDC had launched the Community Health Insurance Scheme, a groundbreaking initiative that aims to administer effective and qualified healthcare services by pooling funds from scheme members. The insurance system is the first of its kind in the Niger Delta, and it intends to cut (out-of-pocket) healthcare costs for roughly 40, 000 people living in four communities in the Obio-Akpor local government region (Rumuobiokani, Rumuezeolu, Oginigba and Rumuomasi). The plan is aimed primarily at the poor, native (indigenous) residents of the area (about 25% of the sample group), however, non-indigenes are also entitled. According to Okonta et al. [16] shell subsidized 50% of the monthly premium for indigenes, presuming that they would be capable of making the other 50% co-payment. As a result of the facility's accessible, cost-effective, and high-quality health facilities, this scheme has resulted in increased use of the facility's services. The facility offers a structured variety of basic care services as well as a narrow selection of secondary quality healthcare, as well as a modest availability of special secondary services, and strong referral networks for patients needing more specialized care. Generalist medical officers provide obstetric services, which are overseen by a specialist obstetrician on sabbatical with SPDC JV. FHI 360, Rotary Club International, and NHIS, among other organizations have partnered in advancement with the Hospital through SPDC.The Rivers State University Teaching Hospital formerly Braithwaite Memorial Hospital (BMH) then BMSH was established in March 1925. It is one of two tertiary hospitals in Rivers State, Nigeria, among the largest in the Niger Delta, with 375 approved beds and 731 medical personnel. It accepts referrals from all private clinics, maternity homes, primary health centers, and secondary health facilities in the state's 23 local government areas. The hospital is government-funded and managed by the Rivers State Hospital Management Board, but patients are recommended to pay for their treatment (apart from a few who have some form of health insurance) [15].It provides emergency obstetric treatment to women referred from other centers, as well as antenatal care and delivery services to low and high-risk pregnant women who have made an appointment with the hospital. The hospital is well-equipped, with a trained team of obstetricians, pediatricians, and anaesthetists available 24 hours a day, 7 days a week. Referrals are made directly from basic and secondary health care providers without regard to any pattern.This was a comparative cross-sectional study, with data collected retrospectively from the case notes of patients.
Sample Size Determination:
The sample size was determined using the formula adopted from the studies of Araoye, 2003; Naing et al. (2006) for test of difference in proportion between two groups [17].
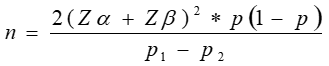
Where;
n = the desired sample size
P1 = Prevalence of tertiary level hospital [9]
P2 = Prevalence of cottage hospital [16]
Zα = value for α error at desired confidence level of 95%. P-value = 0.05 (two-tailed test) in this case zα = 1.96.
Zβ = value of β error which is i-statistical power. At statistical power of 80% and a β error of 20%, (one-tailed test) zβ = 0.84
P = (P1 + P2)/2 is the mean of the two prevalence which were gotten from a previous study = 12.35% = 0.1235.
P1 – P2 = Effect size (difference in prevalence) =7.3% = 0.073
Calculation
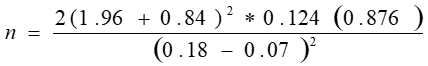
= 140.76 cases
Total sample size (without 10% nonresponse) = 141*2 = 282
10% non-response = 28.2
Total sample size with 10% non-response = 282 + 28.2 = 310.2 =310 cases
That is 155 cases per hospital (including non-response)
Therefore, sample size of cases (155 stillbirth cases in OCH and 155 stillbirth cases in RSUTH) was calculated, minimum required sample size of 310 cases. However, a total population sampling method was adopted so as to get a more comprehensive data.
Study Tool:
A pre-tested data extraction tool adopted from WHO for stillbirth was used [14]. The tool included questions that assessed socio-demographic characteristics, the outcome variable and main explanatory variables (maternal and fetal). All cases were identified through the admission and labour ward register. The folders of the mothers were retrieved from the medical records and statistics department for extraction of relevant information for the study. Data collected were coded, cleaned and analysed using statistical package for social sciences (SPSS)vs 23. Chi-square was used for inferential analysis. Data were reported as descriptive statistics via frequency distribution tables
Results:
In table 1, the socio-demographic characteristics of mothers with still birth foetus was compared between the 2 health facilities studied. One hundred and seventy-one (98.8%) of the mothers in OCH were Christians as compared against 1043 (96.6%) of the mothers in RSUTH who were Christians, and this difference was not shown to be statistically significant (c2=2.548; p=0.110). It was also shown that most of the mothers of the still birth foetus in OCH (90.8%, n=157) and RSUTH (93.5%; n=1010) were residents of urban centres and this was also not shown to be statistically significantly different (c2=1.786; p=0.181). The table also showed that mothers from both health facilities were of comparable age (31.58±5.10 and 31.69±5.24 years for OCH and RSUTH respectively; t=0.255; p=0.799), comparable ethnic groups (c2=3.993; p=0.263), and comparable education (Fishers Exact Test=1.650; p=0.626). One hundred and twenty-three (71.1%) of mothers of still birth foetus in OCH had occupation as against 783 (72.5%) of mothers of still birth foetus in RSUTH, and this was not statistically significantly different (c2=0.146; p=0.702). Also, 78 (45.1%) of mothers in OCH fell into the lower class of household wealth index, 93 (53.8%) fell into the middle class and 2 (1.2%) fell into the upper class of household index. Similarly, 502 (46.5%) of mothers in RSUTH fell into lower class, 563 (52.1%) fell into middle class and 15 (1.4%) fell into the upper class; and this difference was also not statistically significant (c2=0.198; p=0.906). Also, 2 (2.2%) were underweight, 167 (96.5%) were normal and 4 (2.3%) were overweight or obese in OCH while 14 (1.3%) of mothers in RSUTH were underweight, 1051 (97.3%) were normal and 15 (1.4%) were overweight or obese. This difference was not found to be significant (Fishers Exact Test=3.981; p=0.111).
OCH (n=173) | RSUTH (n=1080) | c2 | p-value | |||
Frequency | Percent | Frequency | Percent |
|
| |
| Religion | ||||||
| Christianity | 171 | 98.8 | 1043 | 96.6 | 2.548 | 0.110 |
| Islam | 2 | 1.2 | 37 | 3.4 | ||
| Place of residence | ||||||
| Urban | 157 | 90.8 | 1010 | 93.5 | 1.786 | 0.181 |
| Rural | 16 | 9.2 | 70 | 6.5 | ||
| Ethnicity | ||||||
| Hausa | 0 | 0.0 | 6 | 0.6 | 3.167 | 0.327# |
| Yoruba | 6 | 3.5 | 61 | 5.6 | ||
| Igbo | 50 | 28.9 | 257 | 23.8 | ||
| Others | 117 | 67.6 | 756 | 70.0 | ||
| Maternal age | ||||||
| 15-19 | 1 | 0.6 | 20 | 1.9 | 1.765 | 0.623 |
| 20-29 | 60 | 34.7 | 348 | 32.2 | ||
| 30-39 | 104 | 60.1 | 659 | 61.0 | ||
| 40-49 | 8 | 4.6 | 53 | 4.9 | ||
| Mean ± SD (years) | 31.58±5.10 | 31.69±5.24 | 0.255b | 0.799v | ||
| Mother’s education | ||||||
| None | 1 | 0.6 | 4 | 0.4 | 1.65 | 0.626# |
| Primary | 10 | 5.8 | 46 | 4.3 | ||
| Secondary | 83 | 48 | 516 | 47.8 | ||
| Tertiary | 79 | 45.7 | 514 | 47.6 | ||
| Occupation |
|
|
|
|
|
|
| Has occupation | 123 | 71.1 | 783 | 72.5 | 0.146 | 0.702 |
| No occupation | 50 | 28.9 | 297 | 27.5 |
|
|
| Household wealth index |
|
|
|
|
|
|
| Poor | 78 | 45.1 | 502 | 46.5 | 0.151 | 0.927# |
| Middle | 93 | 53.8 | 563 | 52.1 |
|
|
| Rich | 2 | 1.2 | 15 | 1.4 |
|
|
| BMI status |
|
|
|
|
|
|
| Underweight | 2 | 2.2 | 14 | 1.3 | 3.981 | 0.118# |
| Normal weight | 167 | 96.5 | 1051 | 97.3 |
|
|
| Overweight/Obese | 4 | 2.3 | 15 | 1.4 |
|
|
*Statistically significant (p<0>c2=Chi-Square; α=Fishers Exact p
Table 1: Socio-Demographic characteristics of mothers with stillbirth foetus in Obio Cottage Hospital and Rivers State University Teaching Hospital.
Table 2 shows that half, 50 (28.9%) of the still birth cases reported in OCH were classified as fresh and 123 (71.1%) of the cases were classified as macerated, while 484 (44.8%) of still birth cases reported in RSUTH were classified as fresh and 596 (55.2%) of the cases were classified as macerated. There were significantly more fresh cases in RSUTH compared to OCH, and significantly more macerated case in OCH compared to RSUTH (c2=15.440; p<0>
There is a statistically significant difference in the distribution of mothers’ use of ANC service, number of ANC visits, time of initiation of ANC and ANC booking among mothers of still birth foetus in OCH and RSUTH compared. Among the mothers of the still birth foetus 83.8% (n=145) of those in OCH used at least one ANC as against 70.1% (n=757) of those in RSUTH, and this was statistically significant (ꭓ2=13.924, p<0 n=141) n=643) n=140) N=645)> OCH (n=173) RSUTH (n=1080) ꭓ2 p-value Frequency Percent Frequency Percent 50 28.9 484 44.8 15.44 <0> 123 71.1 596 55.2 28 16.2 323 29.9 13.924 <0> 145 83.8 757 70.1 n=145 n=757 4 2.8 114 15.1 16.194 <0> 141 97.2 643 84.9 93 64.1 433 57.2 15.811 <0> 48 33.1 212 28 4 2.8 112 14.8 n=173 n=1080 140 80.9 645 59.7 28.647 <0> 33 19.1 435 40.3 168 97.1 1007 93.2 5.865 0.046* 3 1.7 19 1.8 2 1.2 54 5 90 52 550 50.9 0.072 0.965 70 40.5 447 41.4 13 7.5 83 7.7 130 75.1 798 73.9 0.122 0.726 43 24.9 282 26.1 132 76.3 854 79.1 0.684 0.408 41 23.7 226 20.9 Type of still birth Fresh Macerated No ANC visit At least one ANC visit Number of ANC visits 1-3 visits >=4 visits Initiation of ANC Early Intermediate Late Booked Yes No Pregnancy desire Wanted Mistimed Unwanted Parity 0-1 child 2-4 children 5 or more children Delivery mode Normal Caesarean section Complication None Yes *=Statistically Significant; #=Fishers Exact Test
Table 2: Comparing clinical characteristics of mothers with stillbirth foetus in OCH and RSUTH
Table 3 shows that there was no statistically significant difference in the gender distribution (61.8% male Vs. 38.2?male, and 59.3% male vs. 40.7?male for OCH and RSUTH respectively; ꭓ2=0.416; p=0.519) and birth weight (44.5% low, 54.9% normal and 0.6% high for deliveries in OCH and 43.1% low, 56.5% normal and 0.4% high for deliveries in RSUTH; ꭓ2=0.745; p=0.652) of still birth foetuses delivered in OCH and RSUTH, but birth order significantly varied between the two facilities compared (ꭓ2=17.287; p=0.004).
OCH (n=173) | RSUTH (n=1080) | ꭓ2 | p-value | |||
Frequency | Percent | Frequency | Percent |
|
| |
| Foetal sex | ||||||
| Male | 107 | 61.8 | 640 | 59.3 | 0.416 | 0.519 |
| Female | 66 | 38.2 | 440 | 40.7 | ||
| Birth weight | ||||||
| Low | 77 | 44.5 | 466 | 43.1 | 0.745 | 0.652 |
| Normal | 95 | 54.9 | 610 | 56.5 | ||
| High | 1 | 0.6 | 4 | 0.4 | ||
| Birth order | ||||||
| First | 66 | 38.2 | 496 | 45.9 | 17.287 | 0.004* |
| Second | 34 | 19.7 | 258 | 23.9 | ||
| Third | 29 | 16.8 | 160 | 14.8 | ||
| Fourth | 27 | 15.6 | 76 | 7.0 | ||
| Fifth | 11 | 6.4 | 56 | 5.2 | ||
| Sixth or more | 6 | 3.5 | 34 | 3.1 | ||
*=Statistically Significant
Table 3: Comparing characteristics of still birth fetuses in Obio Cottage Hospital and Rivers State University Teaching Hospital.
Discussion
Stillbirth delivery among women is a public health concern. The goal of this study was to identify and compare types and associated factors of stillbirth among reproductive-aged women delivering at hospitals in a primary and tertiary health facility in Port Harcourt (OCH and RSUTH).
The study revealed that the socio-demographic characteristics of mothers with stillbirth foetus showed no statistically significant difference among the primary and tertiary health facilities (OCH and RSUTH). This implies that the socio-demographic characteristics of the mothers who had stillborn played no significant role in the occurrence of stillbirth both health facilities. The findings of this study contradict a previous study by Bhusal et al. which identified maternal socio-demographics such as age, occupation, tobacco use, education, and place of residence as associated factors of stillbirth among pregnant women in Nepal [18]. Some studies identified maternal socio-demographics such as low maternal education as an associated factor of stillbirth [19, 20]. Similarly, Dahiru et al. Niger Delta area of Nigeria revealed increased maternal age (> 35 years), lack of or low maternal education, socio-economic status, use of solid fuels, residence, and BMI status as factors associated with stillbirth [21]
The present study however corroborates the findings of Okonofua et al. in a multi-centre study and Ugboma et al. in a retrospective study, Niger Area of Nigeria [2, 6]. The results also reveal that mothers from both facilities were of comparable age, education, and ethnic groups.
The type of stillbirth was significantly associated with the type of health facility. In both facilities, the macerated stillbirth was most prevalent indicating death during the antepartum period. This has serious implications for both the health care providers and the patients alike. It implies that the cause of the stillbirth occurred before labour, and also may imply other factors such as delay in seeking care or getting to the facility by the patient as well as delay in receiving help at the facilities which are well-identified causes of poor pregnancy outcomes [22, 2].
In addition, these findings suggest that there are underlying factors accountable for the disparities in the frequencies and percentages of stillbirth types. The current findings are consistent with those of Ntuli et al. in South Africa and Njoku et al. from a tertiary hospital in Nigeria's Niger Delta [20, 23]. On the other hand, Okonofua et al. in a multi-center study in Nigeria demonstrated that a higher percentage of intrapartum deaths (fresh stillbirth) occurred during the intrapartum period. They also revealed that the timing and procedure of birth may not have followed established obstetric procedures due to hospital delays during delivery [2].
According to Lawn et al., a macerated stillborn foetus exhibits skin and soft-tissue alterations, such as skin discoloration, peeling, redness, and breakdown, which may indicate that the foetus died well before delivery, or prepartum [8]. The higher proportion of macerated cases in OCH compared to RSUTH indicated that the majority of stillbirths occurred 24 hours before delivery, OCH has a pooled insurance program eliminating the financial constraint of receiving medical care and facilitating simple enrollment for focused ANC. This is possibly associated with issues relating to childbirth, pregnancy-related malaria, syphilis, obstetric hemorrhage, preeclampsia, diseases of the mother, or congenital anomalies that may have gone unnoticed or unsupervised in the antenatal period before delivery [2]. Furthermore, because RSUTH is a referral health facility and is probably more equipped than OCH in terms of facilities and obstetric expertise, it might be able to lower the likelihood of a macerated stillbirth because of the presence of specialists. Thirdly, some people may be undermining free services; even if they are registered for ANC, they may not consistently attend the visits because they spend nothing or little on fundamental healthcare. Additionally, some patients may have sought out prayer houses or traditional birth attendants for massages and womb repositioning in an attempt to secure their pregnancies, or they may have been inconsistent in seeking healthcare [19]. Due to cultural preconceptions, when most women are scheduled for surgery, they occasionally look for spiritual alternatives, which may cause the unborn child to pass away before delivery. This is because, even though medical personnel initially informed them that their case was normal, they saw surgery as being against their beliefs or unnecessary [24]. Comparably, the low percentages of fresh stillbirths relative to macerated stillbirths indicate that fewer stillbirth instances occur in the hospitals that are the subject of the investigation during deliveries. This may be explained by the hospitals understudied responding effectively to obstetric emergency cases.
Amongst the clinical characteristics associated with mothers who had a stillbirth, the comparison showed a statistically significant difference of p<0>
The present findings do not corroborate with other studies in Nigeria [25, 26], Malawi [27], and Jamaica [28], that have shown a link between poor antenatal attendance and stillbirth, indicating that moms who did not receive antenatal care had tendencies of having a stillbirth than mothers who did [29].
The reason for this early inclusion of a greater proportion of women in OCH for ANC is likely because OCH is closer to the patients and it is the primary place of contact for health care services compared to RSUTH [3]. Secondly, the fact that RSUTH is a government-owned hospital primarily funded by the state government where patients mostly pay out-of-pocket may be a problem limiting early ANC participation and effective medical care, particularly in emergencies. Whereas OCH is primarily funded by SPDC in partnership with the state government and other ventures, where the efficient implementation of the community health insurance program has removed the financial barrier to seeking medical care and receiving much-needed obstetric treatment in all forms [30].
The findings from this study showed the sex of the foetus predominant in stillbirth from both facilities studies was males recording a proportion of more than half though not statistically significant. The present study corroborates the findings of Shiaa et al. [31]. The reason for this similarity as reported in the present study with previous findings is not known but could be associated with developmental differences in the growth and function of the placenta, or as a result of increased sensitivity of male foetuses to various environmental factors experienced by the mother, which includes advanced maternal age, social deprivation, obesity and smoking [32]. Furthermore, this study also corroborates the findings of Njoku et al. [20] on prevalence and risk factors for stillbirth. The study also revealed that the birth order of foetus was a significant related factor to the occurrence of stillbirth, which corroborates with the findings on stillbirth and birth order [33]. However, there have been controversies as to whether birth order contributes to the chances of having a stillbirth, saying that the more births the more chances of risk of having a stillbirth
Conclusion
Following the findings of the present study, it was deduced that variables such as type of stillbirth, use of ANC, number of ANC visits, initiation of ANC, booked status, and birth order were possible factors associated with stillbirth in OCH and RSUTH in Port Harcourt. This could be a result of the benefit of the community health insurance scheme available at OCH which enabled the majority of the mothers to be enrolled for ANC compared to RSUTH. From the findings, it could also be said that the women attending hospitals have a poor attitude towards seeking health care since most of the stillbirth types appeared macerated showing delay from the mom or infection not detected during ANC. As a result, this study highlights how urgent it is to improve the infrastructure of healthcare institutions as well as the services available to mothers and children, and it also highlights how dire the situation is in this respect. To help with the development of interventions, more comprehension of some of the data and investigation of correlations as well as a qualitative assessment of factors associated with stillbirth delivery are needed. Additionally, utilizing such initiatives as a community-based health insurance system at the PHC will likely enhance the utilization and attendance of prenatal care (ANC) despite expertise-based interventions meant to ensure safe pregnancy outcomes. Hence, the study proposes that the government may reduce the financial burden of out-of-pocket expenses by enrolment in the national health insurance program. This would encourage people to seek medical attention, which would mitigate the incidence of stillbirths. Additionally, there is a critical need for increased sensitization among women on pregnancy danger signs and the importance of timely ante-natal care at a standard healthcare facility by healthcare professionals.
Inclusion criteria
All cases of stillbirth within the period of research, those which occurred at 28 weeks of gestation and above during a 5-year period from January 2015 to December 2019.
Exclusion criteria
Case files that lacked adequate information were excluded from the study.
Ethical Consideration
Ethical approval was sought and obtained from the Research and Ethics Review Committee of the University of Port Harcourt. Permission was obtained from the management of the hospitals before the commencement of the study.
Study Limitations
This is a descriptive study and causality cannot be established.
Conflict of interest
The authors have no conflict of interest to declare for this study
Funding
None.
References
- Aminu, M., Bar-Zeev, S., White, S., Mathai, M., & van den Broek, N. (2019). Understanding cause of stillbirth: a prospective observational multi-country study from sub-Saharan Africa. BMC pregnancy and childbirth, 19(1), 1-10.
View at Publisher | View at Google Scholar - Okonofua, F. E., Ntoimo, L. F. C., Ogu, R., Galadanci, H., Mohammed, G., Adetoye, D., ... & Randawa, A. (2019). Prevalence and determinants of stillbirth in Nigerian referral hospitals: A multicentre study. BMC pregnancy and childbirth, 19(1), 1-9.
View at Publisher | View at Google Scholar - World Health Organization (WHO) (2016). Technical consultation on newborn health indicators. http://www.who.int/maternal_child_adolescent/documents/newborn-health-indicators/en/ (accessed Oct 23, 2018).
View at Publisher | View at Google Scholar - Lawn, J. E., Blencowe, H., Waiswa, P., Amouzou, A., Mathers, C., & Hogan, D., et al. (2016). For the lancet ending preventable stillbirths series study group with the lancet ending preventable stillbirths series advisory group (2016) still-births: Ending preventable mdeaths by 2030. Lancet, 387, 587-603.
View at Publisher | View at Google Scholar - UNICEF (2020). Statistics on women: The state of the world’s children. New York: UNICEF, 2020.
View at Publisher | View at Google Scholar - Ugboma, H. A. A., & Onyearugha, C. N. (2012). Still births in a tertiary hospital, Niger delta area of Nigeria; less than a decade to the millennium developmental goals. International Journal of Tropical Disease & Health, 16-23.
View at Publisher | View at Google Scholar - Adedini, S. A. (2014). Contextual determinants of infant and child mortality in Nigeria (Doctoral dissertation, University of the Witwatersrand, Faculty of Humanities).
View at Publisher | View at Google Scholar - Lawn, J. E., Gravett, M. G., Nunes, T. M., Rubens, C. E., & Stanton, C. (2010). Global report on preterm birth and stillbirth (1 of 7): Definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth, 10(2010), S1.
View at Publisher | View at Google Scholar - Okeudo. C., Ezem, B., & Ojiyi, E. (2012). Stillbirth rate in a teaching hospital in South-eastern Nigeria: a silent tragedy. Ann Med Health Sci Res, 2(2), 176-9.
View at Publisher | View at Google Scholar - Adimora, G. N., Odetunde, I. O. (2007). Perinatal mortality in University of Nigeria Teaching Hospital, Enugu at the end of the last millennium. Niger Journal Clinical Practice, 10(1), 19-23.
View at Publisher | View at Google Scholar - Udoma, E. J., Ekanem, A. D., Abasiattai, A. M., & Bassey, E. A. (2008). Reasons for preference of delivery in spiritual church-based clinics by women of South-South Nigeria. Nigerian Journal of Clinical Practice, 11(2), 100-103.
View at Publisher | View at Google Scholar - WHO, UNICEF, UNFPA, World Bank Group, UN Population Division (2016). Trends in Maternal Mortality: 1990 to 2015. Accessed June 15,2018
View at Publisher | View at Google Scholar - World Health Organization (WHO) (2018). Technical consultation on newborn health indicators. (accessed June 14, 2018).
View at Publisher | View at Google Scholar - National Primary Health Care Development Agency (NPHCDA) (2012). Minimum standards for primary health care in Nigeria. Abuja. Department of Planning, Research and Statistics, National Primary Health Care Development Agency. Available from: www.nphcda.gov.ng.
View at Publisher | View at Google Scholar - Rivers State Ministry of Health. (2020) State Strategic Health Development Plan 2010-2015. Port Harcourt.
View at Publisher | View at Google Scholar - Okonta, P. I., Orimadegun, A. E., Umejiego, C., & Fajola, A. (2020). An Analysis of Still-births from a Busy Cottage Hospital using the Re-Code Classification. Tropical Journal of Obstetrics and Gynaecology, 37(2), 233-242.
View at Publisher | View at Google Scholar - Rivers State Ministry of Health. (2020) State Strategic Health Development Plan 2010-2015. Port Harcourt.
View at Publisher | View at Google Scholar - Araoye, M. O. (2003). Epidemiology of infertility: social problems of the infertile couples. West African journal of medicine, 22(2), 190-196.
View at Publisher | View at Google Scholar - Bhusal M, Gautam N, Lim A, Tongkumchum P. (2019) Factors Associated With Stillbirth Among Pregnant Women in Nepal. J Prev Med Public Health,52(3):154-160. doi: 10.3961/jpmph.18.270. PMID: 31163950; PMCID: PMC6549008.
View at Publisher | View at Google Scholar - Anyichie, N. E., & Nwagu, E. N. (2019). Prevalence and maternal socio-demographic factors associated with stillbirth in health facilities in Anambra, South-East Nigeria. African health sciences, 19(4), 3055-3062.
View at Publisher | View at Google Scholar - Njoku, C. O., Emechebe, C. I., Eyong, E. M., Ukaga, J. T., & Anachuna, K. C. (2016). Prevalence and risk factors for stillbirths in a tertiary hospital in Niger Delta area of Nigeria: a ten-year review. International journal of Medicine and Biomedical research, 5(3), 106-113.
View at Publisher | View at Google Scholar - Dahiru, T., & Aliyu, A. A. (2016). Stillbirth in Nigeria: Rates and risk factors based on 2013 Nigeria DHS. Open Access Library Journal, 3, e2747.
View at Publisher | View at Google Scholar - Banke-Thomas A,Avoka CK, Gwacham-Anisiobi et al. ( 2021) Influence of travel time and distance to the hospital of care on stillbirths: a retrospective facility-based cross-sectional study in Lagos, Nigeria. BMJ Global Health. 2;6:e007052. doi:10.1136/bmjgh-2021-007052
View at Publisher | View at Google Scholar - Ntuli, S. T., & Malangu, N. (2012). An investigation of the stillbirths at a tertiary hospital in Limpopo province of South Africa. Global journal of health science, 4(6), 141.
View at Publisher | View at Google Scholar - Zakar, M. Z., Zakar, R., Mustafa, M., Jalil, A., & Fischer, F. (2018). Underreporting of stillbirths in Pakistan: perspectives of the parents, community and healthcare providers. BMC pregnancy and childbirth, 18(1), 1-9.
View at Publisher | View at Google Scholar - Olusanya, B. O., & Solanke, O. A. (2009). Maternal and neonatal factors associated with mode of delivery under a universal newborn hearing screening programme in Lagos, Nigeria. BMC pregnancy and childbirth, 9, 1-11.
View at Publisher | View at Google Scholar - Olusanya, B. O., Afe, A. J., & Solanke, O. A. (2009). Are risk factors for stillbirths in low-income countries associated with sensorineural hearing loss in survivors? The Journal of Maternal-Fetal & Neonatal Medicine, 22(7), 576-583.
View at Publisher | View at Google Scholar - Kalanda, G. C., Hill, J., Verhoeff, F. H., & Brabin, B. J. (2006). Comparative efficacy of chloroquine and sulphadoxine–pyrimethamine in pregnant women and children: a meta‐analysis. Tropical Medicine & International Health, 11(5), 569-577.
View at Publisher | View at Google Scholar - Del Rosario González Ovalle, M., Alvarado Márquez, J. A., & Martínez Salomón, S. D. (2004). A compilation of resources on knowledge cities and knowledge‐based development. Journal of knowledge management, 8(5), 107-127.
View at Publisher | View at Google Scholar - McClure, E. M., Pasha, O., Goudar, S. S., Chomba, E., Garces, A., Tshefu, A., et al. (2011). Epidemiology of stillbirth in low-middle income countries: A global network study. Acta Obstet Gynecol Scand, 90(12), 1379–85.
View at Publisher | View at Google Scholar - Fakunle, B., Okunlola, M. A., Fajola, A., Ottih, U., & Ilesanmi, A. O. (2014). Community health insurance as a catalyst for uptake of family planning and reproductive health services: the Obio Cottage Hospital experience. Journal of Obstetrics and Gynaecology, 34(6), 501-503.
View at Publisher | View at Google Scholar - Shiaa, N. R., Issa, S. S., & Subber, K. H. (2019). Maternal and Fetal Determinants of Stillbirth among Women Who Attending Maternity Departments of Basra Central Hospitals. Indian Journal of Public Health Research & Development, 10(9).
View at Publisher | View at Google Scholar - Mondal, D., Galloway, T. S., Bailey, T. C., & Mathews, F. (2014). Elevated risk of stillbirth in males: systematic review and meta-analysis of more than 30 million births. BMC medicine, 12(1), 1-11.
View at Publisher | View at Google Scholar - James, W. H. (1968). Stillbirth and birth order. Annals of human genetics, 32(2), 151-162.
View at Publisher | View at Google Scholar

 Clinic
Clinic
