Research Article | DOI: https://doi.org/10.31579/2835-9232/039
Chronic Comorbidities Trend in Covid-19 Patients: Comparison Among 2020, 2021, 2022 And 2023 Years in A General Medicine Office in Toledo, Spain
- Jose Luis Turabian *
Health Center Santa Maria de Benquerencia. Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain.
*Corresponding Author: Jose Luis Turabian, Health Center Santa Maria de Benquerencia. Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain
Citation: Jose Luis Turabian (2023) Chronic Comorbidities Trend in Covid-19 Patients: Comparison Among 2020, 2021, 2022 And 2023 Years in A General Medicine Office in Toledo, Spain, International journal of clinical epidemiology, 2(6); Doi: 10.31579/2835-9232/039
Copyright: © 2023, Jose Luis Turabian. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 10 November 2023 | Accepted: 24 November 2023 | Published: 07 December 2023
Keywords: COVID-19; SARS-CoV-2; chronic conditions; comorbidity; epidemiological characteristic; secondary analysis; general practice
Abstract
Background: It is not clear that chronic comorbidities are risk factors for Covid-19 infection, nor how they havevaried throughout the pandemic and endemic time.
Objective: To compare chronic diseases between cases of covid-19 in 2020, 2021, 2022 and 2023 years in the same population in general medicine.
Methodology: Comparison of secondary data among covid-19 cases in 2020, 2021, 2022 and 2023 years of previous studies, all of them carried out in the same population of patients treated in a general medicine office in Toledo, Spain.
Results:100 covid-19 cases were included in 2020, 42 in 2021, 46 in 2022, and 76 in 2023. The chronic comorbidities general trend was decrease towards the year 2023, except in Circulatory system and genitourinary. No statistically significant differences were found between the prevalence of chronic diseases between the years 2020, 2021, 2022 and 2023, except in the Musculoskeletal group, which was more frequent in 2021.
Conclusions:In the context of general medicine in Toledo (Spain), where Omicron is currently the dominant variant and there are high rates of vaccine coverage, the presence of comorbidity of chronic diseases tends to decrease in patients with covid-19 except in the Circulatory system. Consequently, chronic comorbidities may be risk factors for poor prognosis in Covid-19, but it is not clear that they are risk factors for having covid-19 infection. These results should be taken with caution and their direct application to other different contexts may not be appropriate.
Introduction
The coronavirus disease 2019 (covid-19) has presented mortality rates that largely depended on an individual's comorbidity, so an important risk factor for the severity of covid-19 is the patient's health status in the time of covid-19 infection [1].
Since the beginning of the Covid-19 pandemic, numerous studies have focused on specific chronic diseases and identified comorbidities [2]. It has been shown that SARS-CoV-2 affects the health of infected patients in a way that sometimes depends on pre-existing comorbidities, since it can make covid-19 more severe due to the exacerbation of previous diseases and lead to poor clinical outcomes or mortality [3].
It is known that patients at risk are people who suffer from multiple diseases, or are immunocompromised. The association of infection with comorbidities (diabetes mellitus, arterial hypertension, obesity, chronic kidney disease and chronic obstructive pulmonary disease) darkens the prognosis and causes complications [4-8].
Covid-19 is a disease that is characterized by presenting a very varied clinical picture, with a predominance of respiratory symptoms and symptoms of other organs and systems, of variable intensity, but which can be exacerbated when there is comorbidity. Presentations of covid-19 in unvaccinated people in this first period of the pandemic (In 2020 there were still no vaccines against covid-19) have ranged from mild/asymptomatic symptoms to severe disease and mortality. Thus, the most frequently reported initial signs or symptoms in the first 12 US patients confirmed with covid-19 from January 20 to February 5, 2020, were cough and fever; During the course of the disease reported cough, fever, diarrhea, and vomiting. The symptoms of covid-19 change for those vaccinated: fever is no longer the most permanent symptom, neither is the loss of taste and smell, and rhinorrhea, sore throat or dry cough and headache appear as very frequent symptoms in people with the vaccine. Among vaccinated adults’ symptoms are more closely related to the common cold; there are coughing, but also a higher prevalence of runny noses and sneezes; Headaches and sore throats are other top complaints. Fever and loss of taste and smell are being reported to a lesser extent. From 2022 when the omicron variant is prevalent, and that it appears to replicate rapidly in the upper respiratory tract, its main symptoms included a runny nose, headache, fatigue, sneezing, and sore throat and generally other mild symptoms such as cough, congestion and fatigue [9].
It is evident that identifying comorbidities that can be risk factors for severe cases and also in mild-moderate cases can be useful to guide public health interventions to protect the most vulnerable groups of the population against covid-19. For example, information on risk comorbidities for covid-19 can be used to design risk stratification tools and clinical pathways, thereby establishing more effective early intervention strategies and resource allocation policies.
However, although existing data suggest that these chronic conditions or comorbidities may be risk factors for poor prognosis in covid-19, it is not clear whether or not they are risk factors for developing covid-19. The evolution of the frequency of chronic diseases/comorbidities of covid-19 cases during the pandemic and subsequently in the endemic phase is also unknown, and data is especially lacking in non-hospitalized patients and even more its evolution over time in specific geographic areas [10].
In this context, we present a comparative study based on previously published data, to evaluate the frequency and variation of chronic diseases/comorbidities of covid-19 cases in 2020 (without vaccination), 2021 (with 1 or 2 dose vaccination), 2022 (with first booster), and 2023 (with second booster), from the same population attended in a general medicine consultation in these time periods
Material and Methods
Design and emplacement
This study compares data from previous observational, longitudinal and prospective studies of covid-19 infections from March, 2020 to October, 2023, already published:
1. A study that included unvaccinated covid-19 cases in 2020 (11).
2. Two studies of covid-19 cases in vaccinated people in 2021 (11, 12).
3. A study of covid-19 breakthrough infections in vaccinated people with vaccine booster in 2022 (13)
4. And a study of covid-19 infections in 2023 (14).
All studies were conducted on the same population: patients saw in a general medicine office in Toledo, Spain, which has a list of 2,000 patients > 14 years of age (in Spain, GPs care for people > 14 years of age, except for exceptions). The GPs in Spain work within the National Health System, which is public in nature, and are the gateway for all patients to the system, and each person is assigned a GP (15). The methodology of all studies has been previously published and here only the main elements will be repeated for the current
study [11-14].
Outcome of interest
Evaluation of variation of chronic diseases of covid-19 cases in 2020, 2021, 2022 and 2023.
Definition of chronic diseases
It was defined as "any alteration or deviation from normal that has one or more of the following characteristics: is permanent, leaves residual impairment, is caused by a non-reversible pathological alteration, requires special training of the patient for rehabilitation, and / or can be expected to require a long period of control, observation or treatment [16-18]. And they were classified according to the International Statistical Classification of Diseases and Health-Related Problems, CD-10 Version: 2019 [19].
Statistical analysis
The comparisons were performed using the Chi Square test (X2) or test of Kruskal-Wallis, both with degrees freedom= 3.
Ethical issues
No personal data of the patients were used, but only group results, which were taken from the clinical history.
Results
100 covid-19 cases were included in 2020, 42 in 2021, 46 in 2022, and 76 in 2023. The frequency of chronic comorbidities increased in 2021 and for
some group in 2022, but the general trend was to decrease in the evolution towards 2023. The exception was the tendency to increase towards 2023
in Circulatory system and less strikingly in Genitourinary (FIGURE 1).
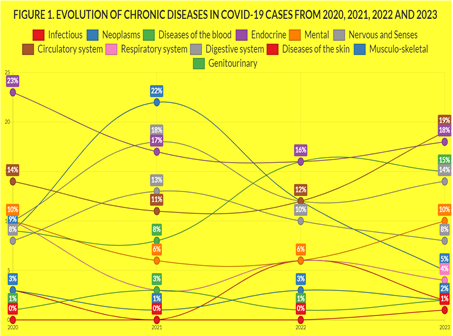
Figure 1: Evolution of Chronic Diseases in Covid-19 Cases From 2020, 2021, 2022 And 2023
No statistically significant differences were found between the prevalence of chronic diseases according to WHO, ICD-10 groups, between the years 2020, 2021, 2022 and 2023, except in the Musculoskeletal group, which was more frequent in 2021 (TABLE 1, FIGURE 1). TABLE 1
CHRONIC DISEASES ACCORDING TO WHO, ICD-10 GROUPS | COVID-19 CASES IN 2020 N=100 | COVID-19 CASES IN 2021 N=42 | COVID-19 CASES IN 2022 N=46 | COVID-19 CASES IN 2023 N=76 | STATISTICAL SIGNIFICANCE
|
-I Infectious | 0 | 0 | 0 | 1 (1) | Kruskal-Wallis (df=3): H= 1.225 p= .747. NS |
-II Neoplasms | 3 (3) | 1 (1) | 5 (3) | 4 (2) | Kruskal-Wallis (df=3): H= 1.5. p= .6823. NS |
-III Diseases of the blood | 1 (1) | 3 (3) | 1 (1) | 3 (2) | Kruskal-Wallis (df=3): H= .77. p= .857. NS |
-IV Endocrine | 26 (23) | 15 (17) | 24 (16) | 28 (18) | X2 (3) = 2.1346. p= .544943. NS |
-V Mental | 11 (10) | 5 (6) | 8 (6) | 15 (10) | X2 (3) = 2.8709. p= .411963. NS |
-VI-VIII Nervous and Senses | 9 (8) | 11 (13) | 14 (10) | 13 (8) | X2 (3) = 1.4889. p= .684826. NS |
-IX Circulatory system | 16 (14) | 10 (11) | 18 (12) | 30 (19) | X2 (3) = 3.7686. p= .287559. NS |
-X Respiratory system | 12 (10) | 3 (3) | 8 (6) | 6 (4) | X2 (3) = 7.0248. p= .071111. NS |
-XI Digestive system | 11 (10) | 14 (16) | 18 (12) | 22 (14) | X2 (3) = 1.836. p= .607133. NS |
-XII Diseases of the skin | 3 (3) | 0 | 8 (6) | 3 (2) | Kruskal-Wallis (df=3): H= 1.31. p= .727. NS |
-XIII Musculo-skeletal | 10 (9) | 19 (22) | 17 (12) | 8 (5) | X2 (3) = 16.5271. p= .000884. Significant at p < .05. |
-XIV Genitourinary | 10 (9) | 7 (8) | 23 (16) | 24 (15) | X2 (3) = 5.5322. p=-.136727. NS |
TOTAL* | 112 (100) | 88 (100) | 144 (100) | 157 (100) | --- |
COMPARISON OF CHRONIC DISEASES IN COVID-19 CASES FROM 2020, 2021, 2022 AND 2023
( ): Denotes percentages; NS: Not significant;* Patients could have more than one chronic disease; the percentages of chronic diseases are over the total of chronic diseases
Discussion
1. Main findings
Our main findings were:
1. There was a tendency for covid-19 cases in 2023 to present fewer chronic diseases by WHO groups, except in the Circulatory system, which tends to increase.
2. No clinically significant differences were found between the prevalence of chronic diseases according to WHO, ICD-10 groups, between the years 2020, 2021, 2022 and 2023.
Two fundamental factors must be taken into account to correctly evaluate our data:
a) On the one hand, the evolution of the variants in the at-risk population studied.
From March to April 2020, in Spain, the A lineage of the coronavirus predominated, especially the SEC7 and SEC8, and from summer to December, 2020, the 20E (EU1) variant [20-21]. From January 2021 the alpha variant predominated, from the summer-autumn of 2021 the delta variant [22-23], and finally Omicron [24]. From the first months of 2022, the Omicron variant was the dominant variant in Spain after having displaced the Delta variant [25]. The predominant variants in Spain during 2023 were those of the XBB family. The XBB.1.5 lineage became dominant globally in February 2023 and in March in Spain. The “Eris” variant (EG.5), a descendant of the omicron, also of the XBB family, has spread rapidly since the end of July 2023 throughout the United States, Europe (including Spain) and Asia [26-30].
b) The vaccination situation. Our study compares chronic comorbidity data in 2020 (without vaccination), 2021 (with 1 or 2 dose vaccination), 2022 (with first booster), and 2023 (with second booster). In Spain, in November 2022, more than 60% of people over 80 years of age, and 37% of people over 60 years of age, already had the second booster dose of the covid-19 vaccine. 92% of the population over 60 years of age with the first booster dose, 93% of people over 12 years of age with the complete regimen and 80% of people over 40 years of age with a booster dose against covid-19 [31-32].
2. Comparison with other studies
The analysis of comorbidities in patients with covid-19 can be done from two different aspects: pre-existing comorbidities in cases of covid-19 as a risk factor for the severity of the disease, and pre-existing comorbidities as a risk factor for having covid-19 disease.
2.1. Pre-existing comorbidities in cases of covid-19 as a risk factor for the severity of the disease.
Vaccination status, viral load, underlying medical conditions, and autoimmune diseases can affect the severity of symptoms. People with comorbidities such as obesity, diabetes or heart disease tend to have a lower physiological reserve to deal with infections, not only coronavirus infections but also other infections (29).
Covid-19 patients with chronic illnesses are more likely to experience severe symptoms and ICU admission and faced a higher risk of mortality. The CDC has listed the conditions that are at highest risk for severe illness from covid-19. These would be: Bronchiectasis, COPD, Interstitial lung disease, Pulmonary hypertension and pulmonary embolism, Cystic fibrosis, Cancer, Cerebrovascular disease, chronic kidney disease, Chronic liver disease (cirrhosis, non-alcoholic fatty liver disease, alcoholic liver disease, autoimmune hepatitis) , Diabetes mellitus type 1 and type 2, Disabilities, including Down syndrome, Heart conditions (such as heart failure, coronary artery disease, or cardiomyopathies), HIV, Tuberculosis, Mental health conditions (such as mood disorders, including depression and schizophrenia spectrum disorders), Neurological conditions (dementia), Obesity, Primary Immunodeficiencies, Solid organ or blood stem cell transplantation [33-38].
According to some statistics, it has been observed that 75% of patients hospitalized with covid-19 have, at least, one comorbidity. The most common are hypertension, diabetes, cancer, neurodegenerative diseases, cardiovascular diseases, and obesity and kidney diseases (3). Thus, a study showed that high blood pressure (46%) and type 2 diabetes mellitus (27%) were the main comorbidities; these, along with other pathologies such as chronic obstructive pulmonary disease, neurological pathology, prostration and immunosuppression, increased the risk of death [39]. A systematic review and meta-analysis indicate that chronic kidney disease, cardiovascular disease, high blood pressure and diabetes mellitus are among the comorbidities that can aggravate the clinical picture and evolution of patients with covid-19 [40].
Likewise, 3 patient phenotypes have been identified: “low morbidity” (58% of patients) with few comorbidities; “high morbidity” (35% of patients) with many comorbidities; and “renal morbidity” (7% of patients), patients with chronic kidney disease regardless of their comorbidity burden. Patients with the “renal morbidity” or “high morbidity” phenotypes had more in-hospital complications and a higher risk of mortality [41].
2.2. Pre-existing comorbidities as a risk factor for having covid-19.
Our results coincide with previous communications regarding the frequency of comorbidities in patients with covid-19. Thus, it has been reported that the most frequent comorbidities among patients with covid-19 were obesity (33%), high blood pressure (32%) and diabetes mellitus (22%) [42]. Another study has reported for 2021 that 30% of covid-19 patients showed comorbidity; cardiovascular disease being the most frequent comorbidity (65%) followed by diabetes mellitus (14) and bronchial asthma (12%) [43]. Other authors have published that the most frequent comorbidity was arterial hypertension [44]. Another study showed that the most common were hypertension, diabetes, obesity and cardiovascular diseases [45]. In another study, it was found that among patients with covid-19, hypertension was a very common condition (37).
But on the other hand, other authors have reported that the covid-19 prevalence is similar in those with or without chronic diseases. Thus, in a study it was published that the prevalence of chronic diseases was high and the covid-19 pandemic affected carriers and non-carriers of chronic diseases in a similar way (38). In another study, it was estimated that compared to adults in the general population, those with covid-19 had a higher prevalence of diabetes and COPD, but a lower prevalence of cardiovascular disease (10).
In a study in the same at-risk population as the current study, we found a higher prevalence of chronic diseases in the reference population in 2016 than in the covid-19 cases considered together from 2020 to 2022, and for all groups of diseases. These results suggested that, in this population, the presence of chronic comorbidities did not seem to be, in themselves, risk factors for developing covid-19 [46].
Strengths and weaknesses of the study
1. The use of databases collected for specific purposes in the primary analysis, other than the secondary analysis, limits the analysis and interpretation of results.
2. Number of covid-19 cases were small; thus, the statistical significance of some variables could be obscured.
3. A strength is that studies carried out on the same risk population are compared; the diagnosis of chronic disease was made with the same criteria, in the same general medicine practice, and carried out by the same researcher, which gives coherence to the results.
Conclusions
According to the results of our study, in our population, it can be said that the frequency of chronic comorbidities according to WHO, ICD-10 groups, in patients with covid-19, increased in 2021 and for some group in 2022, but the general trend It was to decrease in the evolution towards the year 2023. The exception was the tendency to increase towards 2023 in Circulatory system and less strikingly in Genitourinary. No statistically significant differences were found between the prevalence of chronic diseases between the years 2020, 2021, 2022 and 2023, except in the Musculoskeletal group, which was more frequent in 2021. It can be thought that the modifications of the predominant SARS-CoV-2 variants throughout the years 2020 to 2023, and the high level of immunization in 2022 and 2023 in the population under study may have influenced these results.
Consequently, in the context of general medicine in Toledo (Spain), chronic comorbidities may be risk factors for poor prognosis in covid-19, but it is not clear that they are risk factors for having covid-19 infection. In any case, these conclusions must be taken with caution, given the relatively small number of cases, and that they refer to a specific population with a specific evolution of the predominant variants of SARS-CoV-2 throughout the years 2020 to 2023, and with a high level of immunization, so they may not be suitable for other populations.
References
- Raghul Gandhi V, Bagavandas MǤ (2021). Identification of Comorbidity Patterns in Covid-19 Deceased Patients: A Social Network Approach. Epidemol Int: 5(3):000197.
View at Publisher | View at Google Scholar - Carmona-Pírez J, Gimeno-Miguel A, Bliek-Bueno K, et al. (2022) Identifying multimorbidity profiles associated with COVID-19 severity in chronic patients using network analysis in the PRECOVID Study. Sci Rep; 12: 2831
View at Publisher | View at Google Scholar - Silaghi-Dumitrescu R, Patrascu I, Lehene M, Bercea I (2023) Comorbidities of COVID-19 Patients. Medicina (Kaunas); 59(8):1393.
View at Publisher | View at Google Scholar - Serra VMA (2020) [COVID-19. From pathogenesis to high mortality in older adults and those with comorbidities]. Rev Haban Cienc Méd; 19-3379.
View at Publisher | View at Google Scholar - Rearte A, Baldani AEM, Barcena BP, et al. (2020) [Epidemiological characteristics of the first 116,974 cases of covid-19 in Argentina, 2020]. Rev Argent Salud Publica; 12 Suppl COVID-19-5.
View at Publisher | View at Google Scholar - Giralt-Herrera A, Rojas-Velázquez JM, Leiva-Enríquez J (2020) [Relationship between COVID-19 and High Blood Pressure]. Rev Haban Cienc Méd; 19:3246.
View at Publisher | View at Google Scholar - COVID-19, a study from primary care]. Rev Electron Zoilo; 45: 2390.
View at Publisher | View at Google Scholar - Suárez Díaz T, Acosta Piedra Y, Piedra Herrera BC (2021) [COVID-19 in the elderly: review of cases with favorable evolution]. Med Gen Fam; 10(5): 242-6.
View at Publisher | View at Google Scholar - Turabian JL (2023) Covid-19 symptoms time trend: comparison between 2020, 2021, 2022 and 2023 years in a general medicine office in Toledo, Spain. Journal of Infectious Diseases & Treatments. In Press.
View at Publisher | View at Google Scholar - Fang M, Wang D, Tang O, Selvin E (2020) Prevalence of Chronic Disease in Laboratory-Confirmed COVID-19 Cases and U.S. Adults (2017–2018). Diabetes Care; 43 (10):127-8.
View at Publisher | View at Google Scholar - Turabian JL (2022) Sars-Cov-2 Dependent Variables are most important in Epidemiological Triad during Covid-19 Pandemic Evolution. A Comparison Study of Unvaccinated Covid-19 Cases in 2020 with Not Fully Vaccinated Covid-19 Cases in 2021. Archives of Health Science; 6(1).
View at Publisher | View at Google Scholar - Epidemiological Characteristics in a General Medicine Practice in Toledo (Spain). J Community Prev Med; 4(2):23-31.
View at Publisher | View at Google Scholar - Turabian JL (2022) Covid-19 Breakthrough Infections in Vaccinated People with Vaccine Booster In 2022 Versus Covid-19 Cases in Unvaccinated People In 2020: A New Disease Whose Clinic We Should Know or Another Cause of The Old Symptoms of The Common Cold? J General medicine and Clinical Practice; 5(2).
View at Publisher | View at Google Scholar - Turabian JL (2023) Clinical-Epidemiological Covid-19 Case Series Study in Endemic Period, from October 2022 to October 2023, in a General Medicine Office, in Toledo (Spain): Mild Symptoms should not Imply Mild Epidemiological Surveillance. Int Jr Infect Dis & Epidemlgy; 4(2):1-6.
View at Publisher | View at Google Scholar - Turabian JL (1995) [Notebooks of Family and Community Medicine. An introduction to the principles of Family Medicine]. Madrid: Díaz de Santos.
View at Publisher | View at Google Scholar - Strauss AL (1984) Chronic illness and the quality of life. St Louis: The C.V. Mosby Company.
View at Publisher | View at Google Scholar - Gill M (2017) Augmented care: An alternative model of care for people with chronic disease. Int J Care Coord; 20 (1-2): 5-7.
View at Publisher | View at Google Scholar - Gerontol a Biol Sci Med; 72(10):1417-23.
View at Publisher | View at Google Scholar - WHO. (2019) International Statistical Classification of Diseases and Health-Related Problems. ICD-10 Version.
View at Publisher | View at Google Scholar - dominating genetic variant. Nature Genetics.
View at Publisher | View at Google Scholar - Hodcroft EB, Zuber M, Nadeau S, et al. (2020) Spread of a SARS-CoV-2 variant through Europe in the summer of 2020, Nature.
View at Publisher | View at Google Scholar - Centro de Coordinación de Alertas y Emergencias Sanitarias (2021) [Update on the epidemiological situation of variant B.1.1.7 of SARS-CoV-2 and other variants of interest. February 08, 2021]. Ministerio de sanidad. Gobierno de España.
View at Publisher | View at Google Scholar - García Marín AM, Chiner Oms A, González Candelas F, Comas Espadas I, López MG, Coscolla Devis M (2021) [What genomic epidemiology teaches us about the waves of COVID-19 in Spain (and how to avoid a new wave)]. The Conversation; 11 de Julio.
View at Publisher | View at Google Scholar - de Sanidad. Gobierno de España.
View at Publisher | View at Google Scholar - Centro de Coordinación de Alertas y Emergencias Sanitarias (2022) [Update of the epidemiological situation of SARS-CoV-2 variants in Spain. May 03, 2022]. Ministerio de sanidad. España.
View at Publisher | View at Google Scholar - Centro de Coordinación de Alertas y Emergencias Sanitarias (2023) [May 22, 2023 Update on the epidemiological situation of SARS-CoV-2 variants in Spain]. Ministry of Health. Spain
View at Publisher | View at Google Scholar - Viciosa M (2023) [If you have covid today, the new variant O EG.5 or 'Eris' may have something to do with it (and it is not more serious)]. Newtral; 11 agosto.
View at Publisher | View at Google Scholar - Pérez B (2023) [The new eris variant, more contagious, already alerts doctors to the rebound in covid]. El Periódico; 10 de agosto.
View at Publisher | View at Google Scholar - Looi M (2023) Covid-19: Hospital admissions rise in England amid fears of new variant and waning immunity. BMJ; 382-1833.
View at Publisher | View at Google Scholar - Smith DG (2023) What to Know About the New Dominant Covid Variant. EG.5 is spreading quickly, but experts say it’s no more dangerous than previous versions. Another new variant, called BA.2.86, is being closely watched because of its mutations. The New York Times; Aug. 11.
View at Publisher | View at Google Scholar - Vacuna Covid-19 (2021) [Covid-19 vaccination strategy in Spain]. Ministerio de sanidad.
View at Publisher | View at Google Scholar - Notas de Prensa (2022) [More than 60% of people over 80 years of age now have a second booster dose against COVID-19]. Ministerio de Sanidad. España; 11-11.
View at Publisher | View at Google Scholar - National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases (2022) Science Brief: Evidence Used to Update the List of Underlying Medical Conditions Associated with Higher Risk for Severe COVID-19. CDC; Updated Feb. 15.
View at Publisher | View at Google Scholar - Tisminetzky M, Delude C, Hebert T, Carr C, Goldberg RJ, Gurwitz JH (2022) Age, Multiple Chronic Conditions, and COVID-19: A Literature Review. J Gerontol A Biol Sci Med Sci; 77(4): 872-8.
View at Publisher | View at Google Scholar - Gimeno-Miguel A, Bliek-Bueno K, Poblador-Plou B, et al. (2021) Chronic diseases associated with increased likelihood of hospitalization and mortality in 68,913 COVID-19 confirmed cases in Spain: A population-based cohort study. PLOS ONE 16(11): 0259822.
View at Publisher | View at Google Scholar - Semenzato L, Botton J, Drouin J, et al. (2021) Chronic diseases, health conditions and risk of COVID-19-related hospitalization and in-hospital mortality during the first wave of the epidemic in France: a cohort study of 66 million people. Lancet Reg Health Eur; 8: 100158.
View at Publisher | View at Google Scholar - JinSong G, XiaoLan Y, HaiNi B, et al (2021) Chronic Diseases as a Predictor for Severity and Mortality of COVID-19: A Systematic Review with Cumulative Meta-Analysis. Front Med; 8.
View at Publisher | View at Google Scholar - Mesenburg MA, Hallal PC, Menezes AMB, et al. (2021) Chronic non-communicable diseases and COVID-19: EPICOVID-19 Brazil results. Rev Saude Publica; 55-38.
View at Publisher | View at Google Scholar - Balboa CT, Lopez J, Muñoz NS, Concha C, Oñat M, Briones J (2021) Comorbidities associated with the risk of dying from COVID-19 in a cohort of patients admitted to a high complexity hospital. Medwave; 21(2):25.
View at Publisher | View at Google Scholar - Plasencia-Urizarri TM, Aguilera-Rodríguez R, Almaguer Mederos LE (2020) [Comorbidities and clinical severity of COVID-19: systematic review and meta-analysis]. Rev Haban Cienc Méd; 19-3389.
View at Publisher | View at Google Scholar - Benítez ID, de Batlle J, Torres G, et al. (2022) Prognostic implications of comorbidity patterns in critically ill COVID-19 patients: A multicenter, observational study. Lancet Reg.
View at Publisher | View at Google Scholar - Villagrán-Olivas K, Torrontegui-Zazueta L,Entzana-Galindo A (2020) [Clinical-epidemiological characteristics of COVID-19 patients in a Sinaloa Hospital, México]. Rev Med UAS; 10 (2): 65-79.
View at Publisher | View at Google Scholar - Ríos Goicochea E, Córdova Paz Soldán OM, Gómez Goicochea NI, Vicuña Villacorta J (2022) Post-infection sequelae of COVID 19 among patients of Hospital I Florencia de Mora. Trujillo - Peru. Rev. Fac. Med. Hum; 22(4): 754-64.
View at Publisher | View at Google Scholar - ESSALUD-La Libertad, 2020]. REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo Palma; 21(4).
View at Publisher | View at Google Scholar - Romero-Nájera DE, Puertas-Santana N, Rivera-Martínez M, Badillo-Alviter G, Rivera-Vázquez P (2021) [Covid-19 and chronic diseases, an analysis in Mexico]. Rev MedUAS; 11(1).
View at Publisher | View at Google Scholar - Turabian J L (2022) Frequency and Variation of Chronic Diseases of Covid-19 Cases from 2020 to 2022 in General Medicine and Comparison with Baseline Data from the Same Population in 2017, in Toledo (Spain). J Community Prev Med 2022;5(2):01-7.
View at Publisher | View at Google Scholar

 Clinic
Clinic
