Case Report | DOI: https://doi.org/10.31579/2835-8295/064
Benign Prostate Hypertrophy: an Educational Ultrasound Images and Pharmacotherapy Mini-Review
*Corresponding Author: Aamir Al-Mosawi. Independent Researcher; No. 18, Haft e Tir 40; Mashhad, Iran.
Citation: Aamir A. Mosawi, (2024), Benign Prostate Hypertrophy: an Educational Ultrasound Images and Pharmacotherapy Mini-Review, International Journal of Clinical Reports and Studies, 3(3); DOI:10.31579/2835-8295/064
Copyright: © 2024, Aamir Al-Mosawi. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 05 April 2024 | Accepted: 29 May 2024 | Published: 13 June 2024
Keywords: benign enlargement of the prostate; ultrasonography; evidenced-based treatment; expert opinion
Abstract
Background: A benign increase in the size of prostate (Enlargement) can be asymptomatic, but it can cause symptoms resulting from pressure on the urethra, including frequency of urination, difficulty in starting urination, poor urine stream, dribbling after urination, and inability to pass urine. Ultrasonography has been used as early as 1971 for the diagnosis of prostatic enlargement.
Patients and methods: This article describes the case of a 53-year-old male with diabetes, hypertension, and refractory psoriasis who developed benign prostatic enlargement. Educational ultrasound images are provided. Treatment for his comorbidities has been detailed in previous publications.
Results: The patient was complaining of dribbling after micturition for few weeks. He was not having difficulty in starting urination nor complained of frequent micturition, and the urine stream was considered normal. The urinary bladder was normal, but with mild hazy wall outline. Pre-voiding volume was 248 ml, and post-voiding volume was 9 ml. Ultrasound of the prostate showed enlarged prostate with homogenous texture. Prostate volume was 36.6 ml (Normal: 25 ml). Therefore, Oral finasteride was started.
Conclusion: Many medications have been used in the treatment of benign enlargement of the prostate during the 1960s, 1970s, and 1980s, including progestational agents, Amino acids, spironolactone, candicidin, nystatin, flutamide, bromocriptine, alpha-adrenergic blockers, Serenoa repens (Saw palmetto extracts), and mepartricin. However, the current evidence-based opinion suggests that benign enlargement of the prostate can be initially treated with medications that can reduce the volume of the prostate such as finasteride and dutasteride. Tamsulosin or alfuzosin can be added to further improve lower urinary symptoms.
Introduction
A benign increase in the size of prostate (Enlargement) can be asymptomatic, but it can cause symptoms resulting from pressure on the urethra, including frequency of urination, difficulty in starting urination, poor urine stream, dribbling after urination, and inability to pass urine. Since as early as 1971, ultrasonography has been utilized for diagnosing prostatic enlargement [1, 2, 3].
Patients and methods
This article describes the case of a 53-year-old male with diabetes, hypertension, and refractory psoriasis who developed benign prostatic enlargement. Educational ultrasound images are provided. Treatment for his comorbidities has been detailed in previous publications [4, 5].
Results
The patient presented with post-micturition dribbling for several weeks, without difficulty initiating urination or increased urinary frequency. Urine stream was deemed normal, and there was no evidence of urinary tract infection. Renal ultrasound revealed a simple renal cyst measuring 23 mm in diameter on the left kidney, with both kidneys otherwise appearing normal. The urinary bladder exhibited a normal appearance, albeit with a mildly hazy wall outline. Pre-voiding volume was measured at 248 ml, with a post-voiding volume of 9 ml. Prostate ultrasound (Figure-1) revealed an enlarged prostate with homogeneous texture and no evidence of space-occupying lesions. Prostate volume was measured at 36.6 ml (normal range: <25>
Discussion
Since 1971, ultrasonography has been pivotal in diagnosing prostatic enlargement [1, 2, 3]. In 1990, Fehr and Knönagel underscored its significance in assessing medical treatments, suggesting a ≥15% reduction in prostate volume post-treatment as clinically significant [3].
Many medications have been used in the treatment of benign enlargement of the prostate during the 1960s, 1970s, and 1980s, including progestational agents, Amino acids, spironolactone, candicidin, nystatin, flutamide, bromocriptine, alpha-adrenergic blockers, Serenoa repens (Saw palmetto extracts), and mepartricin [6-15].
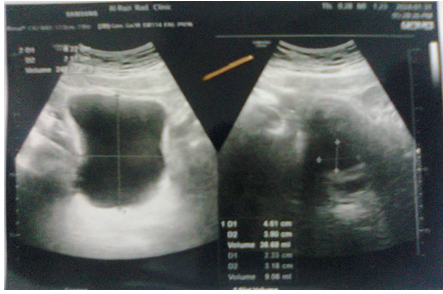
Figure-1A: Ultrasound of the prostate showed enlarged prostate
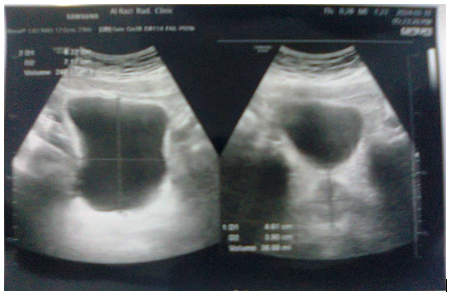
Figure-1B: Ultrasound of the prostate showed enlarged prostate
Finasteride, a 5-alpha-reductase inhibitor, has gained prominence since the early 1990s for treating benign prostatic enlargement [16]. Stoner (1990) highlighted its efficacy in reducing prostate volume by 28% over six months without significant adverse effects. Stoner emphasized that oral finasteride can considerably reduce the elevated level of dihydrotestosterone in the prostate which is the main androgen responsible for prostate enlargement without decreasing testosterone levels. Stoner reviewed the literature and found that finasteride can reduce the volume of prostate by 28% over six months, and without important adverse effects [16].
In 1998, Roehrborn et al. from the United States conducted a meta-analytic study demonstrating the symptomatic improvement and enhanced urinary flow rate associated with finasteride treatment, especially in patients with larger prostates. The meta-analysis included six placebo-controlled studies involving patients with benign hypertrophy patients treated with either 5 mg oral finasteride for at least one year or placebo. The meta-analysis showed that finasteride treatment was associated with symptomatic improvement and improved urinary flow rate, and it was effective in patients with larger prostates [17].
Tamsulosin, the first prostate-selective alpha 1A-adrenoceptor blocker, was evaluated by Chapple et al. from the United Kingdom in 1996; they found it to be safe, well-tolerated, and effective in improving symptoms and urinary flow rate. Chapple et al. conducted a meta-analytic study which included two
placebo-controlled studies that included patients with benign hypertrophy of the prostate. 382 patients with treated with 0.4 mg modified-release tamsulosin (The first prostate-selective alpha 1A-adrenoceptor blocker) one time daily for 12 weeks, and 193 patients who received placebo. The meta-analysis showed that tamsulosin treatment was safe and was well-tolerated. Tamsulosin treatment was associated with symptomatic improvement and improved urinary flow rate. Treatment was not associated with important changes in blood pressure or pulse rate in hypertensive and non-hypertensive patients [18].
In 1998, Wilt et al. from the United States conducted a systematic review which included 18 controlled studies involving 2939 patients with benign hypertrophy of the prostate. Wilt et al found that when compared with finasteride, Serenoa repens (Saw palmetto extracts) can result in similar improvement in urinary flow and urinary tract symptoms. Serenoa repens was associated with less adverse effects [19].
In 1999, Djavan and Marberger conducted meta-analysis which included patients with benign hypertrophy of the prostate associated with obstructive symptoms. They found that alpha1-adrenoceptor blockers had similar beneficial effects in improving symptoms and flow. However, alfuzosin and tamsulosin were better tolerated than doxazosin, terazosin and prazosin, and tamsulosin had less effect hypotensive effect than alfuzosin particularly in older patients [20].
In 2004, Boyle et al. from Italy reported an updated meta-analysis which included 17 placebo-controlled studies involving 4280 patients with benign hypertrophy of the prostate. The meta-analysis showed that treatment with Serenoa repens extract was associated with symptomatic improvement, marked reduction in nocturia and improved peak urine flow [21]. In 2014, Park and Choi from the United States reported a systematic review and meta-analysis which showed that dutasteride, another 5α-reductase inhibitor had a beneficial effect in benign prostate enlargement similar to that of finasteride, and both were associated with a similar rate of adverse effects [22]. In 2016, Kosilov et al. from Russia evaluated the combination of anti-muscarinic medications with tamsulosin, concluding that it improved symptoms of overactive bladder without compromising safety. They conducted a study which included 338 patients with benign prostate enlargement who have significant symptoms of overactive bladder with dribbling. Patients were treated with zamifenacin 5 mg plus tropism 5 mg (Anti-muscarinic medications) plus tamsulosin 0.4 mg daily or tamsulosin 0.4 mg (Control patients). The addition of anti-muscarinic medications to tamsulosin improved symptoms of overactive bladder and was considered safe [23].
Conclusion
Current evidence supports the initial use of medications like finasteride and dutasteride to reduce prostate volume in benign prostatic enlargement. Additionally, drugs like tamsulosin or alfuzosin can be added to further alleviate lower urinary symptoms.
Conflict of interest: None.
References
- Watanabe H, Kaiho H, Tanaka M, Terasawa Y. (1971). Diagnostic application of ultrasonotomography to the prostate. Invest Urol Mar; 8(5):548-559.
View at Publisher | View at Google Scholar - Abdurasulov DM, Fazylov AA, Egamberdyev AIu. (1972). Metodika ul'trazvukovogo issledovaniia pri zabolevaniiakh predstatel'noĭ zhelezy [A method of ultrasound study of prostate gland diseases]. Med Tekh Jan-Feb; 1:46-48. [Article in Russian].
View at Publisher | View at Google Scholar - Fehr JL, Knönagel H. (1990). Importance of prostatic sonography in the evaluation of conservative therapy of prostatic hyperplasia. Urol Int; 45(4):231-233.
View at Publisher | View at Google Scholar - Al-Mosawi AJ. (2023). The Use of Mycophenolate Mofetil in Psoriasis: An Educational Article and Expert Opinion. International Journal of Clinical Epidemiology (ISSN: 2835-9232) May 29; 2(3):1-4.
View at Publisher | View at Google Scholar - Al-Mosawi AJ. (2023). The Therapeutic Challenge of Treating Refractory Psoriasis: An Educational Article and Expert Opinion. Journal of Dermatology and Dermatitis (ISSN: 2578-8949) July 25; 8 (4): 1-3.
View at Publisher | View at Google Scholar - Wolf H, Madsen PO. (1968). Treatment of benign prostatic hypertrophy with progestational agents: a preliminary report. J Urol Jun; 99(6):780-785.
View at Publisher | View at Google Scholar - Shiga H, Kumamoto E, Imamura A. (1968). [Amino acid therapy for hypertrophy of the prostate]. Hinyokika Kiyo. Aug; 14(8):625-632
View at Publisher | View at Google Scholar - Castro JE, Griffiths HJ, Edwards DE, Shackman R. (1969). A controlled clinical trial of aldactone-A in the treatment of benign prostatic hyperplasia. Br J Surg Aug; 56(8):632.
View at Publisher | View at Google Scholar - Orkin LA. (1974). Efficacy of candicidin in benign prostatic hypertrophy. Urology Jul; 4 (1):80-84.
View at Publisher | View at Google Scholar - Bourke JB, Griffin JP, Theodorides P. A (1974). double blind trial of a polyene macrolide: nystatin in the treatment of benign prostatic hyperplasia in man. Br J Urol. Aug; 46(4):463-466.
View at Publisher | View at Google Scholar - Bonard M, de Almeida S, (1976). von Niederhäusern W. Placebo-controlled double-blind study in human benign obstructive prostatic hypertrophy with flutamide. Eur Urol; 2(1):24-28.
View at Publisher | View at Google Scholar - Farrar DJ, Pryor JS. (1976). The effect of bromocriptine in patients with benign prostatic hypertrophy. Br J Urol Feb; 48 (1):73-75.
View at Publisher | View at Google Scholar - Boreham PF, Braithwaite P, Milewski P, Pearson H. (1977). Alpha-adrenergic blockers in prostatism. Br J Surg Oct; 64(10):756-757.
View at Publisher | View at Google Scholar - Champault G, Patel JC, Bonnard AM. (1984). A double-blind trial of an extract of the plant Serenoa repens in benign prostatic hyperplasia. Br J Clin Pharmacal Sep; 18(3):461-462.
View at Publisher | View at Google Scholar - Cortecchia V, Scarano P, D'Amato G, Soli M, Rusconi R, Buli P. (1988). Valutazione clinica sull'uso della mepartricina nella terapia dell'ipertrofia prostatica. Studio in doppio cieco [Clinical evaluation of the use of mepartricin in the therapy of prostatic hypertrophy. Double-blind study]. Minerva Urol Nefrol Apr-Jun; 40(2 Suppl):44-6 [Article in Italian].
View at Publisher | View at Google Scholar - Stoner E. (1990). The clinical development of a 5 alpha-reductase inhibitor, finasteride. J Steroid Biochem Mol Biol Nov 20; 37(3):375-378.
View at Publisher | View at Google Scholar - Roehrborn CG. (1998). Meta-analysis of randomized clinical trials of finasteride. Urology. Apr; 51(4A Suppl):46-49.
View at Publisher | View at Google Scholar - Chapple CR, Wyndaele JJ, Nordling J, Boeminghaus F, Ypma AF, Abrams P. (1996). Tamsulosin, the first prostate-selective alpha 1A-adrenoceptor antagonist. A meta-analysis of two randomized, placebo-controlled, multicentre studies in patients with benign prostatic obstruction (symptomatic BPH). European Tamsulosin Study Group. Eur Urol; 29(2):155-167.
View at Publisher | View at Google Scholar - Wilt TJ, Ishani A, Stark G, MacDonald R, Lau J, Mulrow C. (1998). Saw palmetto extracts for treatment of benign prostatic hyperplasia: a systematic review. JAMA Nov 11; 280(18):1604-1609.
View at Publisher | View at Google Scholar - Djavan B, Marberger M. (1999). A meta-analysis on the efficacy and tolerability of alpha1-adrenoceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic obstruction. Eur Urol; 36(1):1-13.
View at Publisher | View at Google Scholar - Boyle P, Robertson C, Lowe F, Roehrborn C. (2004). Updated meta-analysis of clinical trials of Serenoa repens extract in the treatment of symptomatic benign prostatic hyperplasia. BJU Int. Apr; 93(6):751-756.
View at Publisher | View at Google Scholar - Park T, Choi JY. (2014). Efficacy and safety of dutasteride for the treatment of symptomatic benign prostatic hyperplasia (BPH): a systematic review and meta-analysis. World J Urol. Aug; 32(4):1093-105. Doi: 10.1007/s00345-014-1258-1259.
View at Publisher | View at Google Scholar - Kosilov KV, Loparev SA, Ivanovskaya MA, Kosilova LV. (2016). Effectiveness of Solifenacin and Trospium for Managing of Severe Symptoms of Overactive Bladder in Patients with Benign Prostatic Hyperplasia. Am J Mens Health Mar; 10(2):157-163.
View at Publisher | View at Google Scholar

 Clinic
Clinic
