Research Article | DOI: https://doi.org/DOI:10.31579/2835-2882/021
Association Of Dietary Inflammatory Index with Inflammatory Markers Like C-Reactive Protein and Interleukin-6 In Women with And Without Polycystic Ovarian Syndrome: A Comparative Case-Control Study
1 Tarbiat Modares University, Tehran, Iran.
2 Iran University of Medical Sciences, Tehran, Iran.
3 Shahid Beheshti University of Medical Sciences, Tehran, Iran.
*Corresponding Author: Shahideh Jahanian Sadatmahalleh, Tarbiat Modares University, Tehran, Iran.
Citation: Khadijeh Azarbayjani, Shahideh J. Sadatmahalleh, Azadeh Mottaghi, Maliheh Nasiri, (2023), Association Of Dietary Inflammatory Index with Inflammatory Markers Like C-Reactive Protein and Interleukin-6 In Women with And Without Polycystic Ovarian Syndrome: A Comparative Case-Control Study, Clinical Research and Studies, 2(3); DOI:10.31579/2835-2882/021
Copyright: © 2023, Shahideh Jahanian Sadatmahalleh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 24 May 2023 | Accepted: 02 June 2023 | Published: 13 June 2023
Keywords: pcos; diet inflammatory index; inflammation; nutrition
Abstract
Background: Considering that interventions related to lifestyle, especially nutrition have been proposed as the first line of prevention and treatment of Polycystic Ovarian Syndrome (PCOS), and regarding the proven relationship between PCOS and inflammation, the present study was designed to find out the possible association of Diet Inflammatory Index (DII) with the inflammatory markers like C-reactive protein (CRP) and Interleukin-6, and compare the obtained results in women with and without PCOS.
Method: This case-control study was conducted on 45 PCOS women and 40 non-PCOS women. Food intake and DII were measured using a 147-item food frequency questionnaire. All participants were tested for the serum levels of Interleukin-6 and CRP. Finally, the obtained results were compared between the two groups of PCOS and non-PCOS women.
Results: Significant differences were observed between the two groups in terms of age, menstrual status and number of pregnancies (P<0.05). Comparison of DII value showed no significant difference between the two groups (P=0.68), but Interleukin-6 was significantly higher in the PCOS group than in the control group (4.94±1.97 vs. 3.48±1.77, P<0.001). Also, in terms of CRP, no significant difference was observed between the two groups (P>0.05).
Conclusions: Although the difference of DII between the case and control groups and its association with PCOS was not significant in the current study, it seems that diet, especially consumption of more carbohydrates plays a role in causing chronic inflammation and occurrence and exacerbation of PCOS.
Introduction
Polycystic Ovarian Syndrome (PCOS) is the most prevalent female endocrine disorder, which is characterized by various collections of symptoms such as elevated androgen level, menstrual abnormality and morphological manifestations of polycystic ovaries in reproductive-aged women (1). Approximately 4–20% of women of childbearing age are affected by this disorder and its associated complications (2). PCOS is a lifelong disorder in women, and its metabolic and reproductive effects are well known in women's lives (3). PCOS is a condition with chronic mild inflammation, which is associated with an increase in some inflammatory markers such as C-reactive protein (CRP) (4). Diet plays a major role in regulating chronic inflammation, and inflammation caused by diet is the basis for insulin resistance and hyperandrogenism, which are the main component of PCOS (5). It has been shown that some foods like glucose can cause chronic inflammation through oxidative stress (5, 6). Interventions related to lifestyle changes, including nutrition, exercise and weight loss are the first line of treatment for PCOS women (7). Changes in the composition of diet for the management, treatment and even prevention of this disorder have recently gained much research attention. Furthermore, making changes in the composition of diet causes a decrease in androgen hormones that lead to emergent of clinical symptoms of PCOS (8). Therefore, finding the right diet is important, especially for thin women with PCOS. The present study aimed to investigate the possible association of Diet Inflammatory Index (DII) with the inflammatory markers like C-reactive protein (CRP) and Interleukin-6, and compare the obtained results in women with and without PCOS.
Methods
Participants: This case-control study was conducted on a total of 85 women in two groups: a case group consisting of women with PCOS (n = 45) and a control group of 40 women without PCOS with the aim of investigating the possible association of Diet Inflammatory Index (DII) with the inflammatory markers like C-reactive protein (CRP) and Interleukin-6, and compare the obtained results in women with and without PCOS. Prior to commencing the study, ethical clearance was sought from The Ethics Committee of Tarbiat Modares University of Medical Sciences (IR.MODARES.REC.1399.177). A random sample of women was recruited from those referring to one of the Obstetrics and Gynecology clinics in Robat Karim City, located in Tehran Province between May 2021 and February 2022. The participants were divided into two groups according to having and not having PCOS based on the Rotterdam criteria and with a physician diagnosis, or having a previous history of PCOS diagnosis based on medical records. Due to lack of similar studies, at first, 20 PCOS women and 20 women without PCOS were selected to conduct a pilot study. The calculation of an adequate sample size was done based on the results of the pilot study and using the following formula:

The observed effect size based on the level of Interleukin-6 in a pilot sample of 40 women (20 women in each group) was equal to 0.73. Considering the obtained 95% confidence interval, 90% power and 0.73 effect size in the pilot sample, the minimum sample size in each group was determined to be 40 women. Figure 1 shows the flow chart of the study.
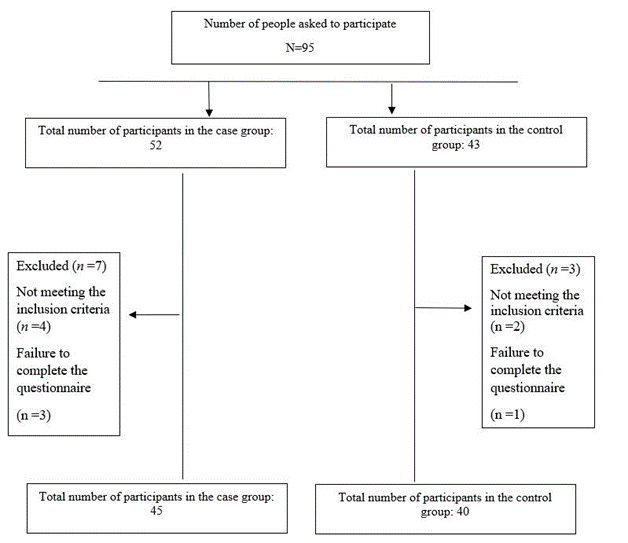
Figure 1: Flow chart of the study
Criteria for selecting the subjects were as follows: women of reproductive age, not having fever and cold symptoms, not suffering from chronic diseases (e.g., diabetes, atherosclerosis, high blood pressure, liver and kidney diseases, rheumatic diseases, etc.) according to medical records and individual reports, absence of other inflammatory diseases like endometriosis and myoma, absence of pregnancy and breastfeeding, not taking drugs that lower blood pressure and sugar and affect appetite, and having PCOS according to the Rotterdam criteria in the case group. If any of the women did not want to participate and continue the research or after completing the questionnaire, their energy intake was more than 4200 or less than 800 kilocalories, they were excluded from the study. Before data collection, the participants received an explanation of the project. And after obtaining written informed consent from the all participants in both groups, a questionnaire of demographic information (including questions about age, marital status, employment status, education, height and weight, history of chronic diseases, history of drug use, and fertility and menstruation information) was completed. Also, all participants were subjected to blood pressure, height and weight measurement and Body Mass Index (BMI) calculation by the researcher.
Dietary assessment
The participants’ nutritional intake was obtained through a 147-item Food Frequency Questionnaire (FFQ) whose validity and reliability were previously evaluated (9). After receiving the necessary training and consultations in the field of completing and interpreting the FFQ from the nutritionist member of the research team, it was completed for all participants in the two groups by the researcher. The information obtained from the questionnaire was entered into the IV Nutritionist software to obtain the exact intake of energy and micronutrients. The participants were asked to report the frequency of consumption of each food item during the last year according to the size of certain portions. The frequency of consumption was manually converted to daily intakes, and then to grams per day using home measurements. Finally, by summing up the values of each nutrient, the total dietary intake of that nutrient was calculated.
Calculation of the Diet Inflammatory Index (DII)
The data related to 31 food items (available in the existing studies), including vitamin B12, vitamin B6, beta-carotene, folic acid, fiber, fats, energy, cholesterol, carbohydrates, caffeine, iron, magnesium, niacin, protein, riboflavin, selenium, thiamin, vitamin A, vitamin C, vitamin D, zinc, trans fatty acids, saturated fatty acids (SFA), mono-unsaturated fatty acids (MUFAs), poly-unsaturated fatty acids (PUFAs), garlic, onion, saffron, turmeric, black tea and pepper were used in order to evaluate the DII. According to whether they increase, decrease, or have no role in inflammation in the diet based on six inflammatory indicators, including IL 10, IL6, IL4, IL1b, TNFa, and CRP, they were given score + 1, -1, or 0, respectively.
Measuring the inflammatory indices of Interleukin-6 and CRP:
After 12–14 hours of fasting, 5 cc of venous blood samples were taken from all participants to measure their inflammatory markers. Then the samples were centrifuged and the resulting plasmas were stored in a freezer at -20oC until the tests were performed. In this study, the human Interleukin-6 ELISA kit produced by the Zell Bio Company (Germany) was used. The basis of this method is an immunoassay based on sandwich ELISA. Moreover, CRP was measured using the latex agglutination method, and values less than 40 mg/liter were considered as negative and values above 40 mg/liter were considered as positive.
Statistical Analysis:
Statistical analysis was performed using the SPSS software (ver. 20). Independent t-test was used in order to compare the two groups in terms of quantitative variables such as age and BMI. Qualitative variables were compared using the Chi-square test. A P < 0.05 level was chosen for statistical significance. Considering that the two groups were not matched in terms of variables like age and number of children, the analysis of covariance test was used to compare the two groups in terms of DII and other food parameters, as well as the inflammatory marker Interleukin-6.
Results
The present case-control study was conducted on 45 women with PCOS (case group) and 40 non-PCOS women (control group). After the interview, 10 participants (10.5%) were excluded from the study due to not meeting the inclusion criteria and failure to complete the questionnaire (Fig. 1). Mean ± standard deviation was used to describe quantitative variables, and number and percentage were used for qualitative variables. Table 1 presents a comparative analysis of demographic and fertility characteristics in the two groups. The mean age of women in the case and control groups was 27.93 ± 6.64 and 33.02 ± 7.19 years, respectively. A significant difference was observed between the two groups in terms of age, number of pregnancies, and menstrual status (P˂0.05). As shown in Table 1, there was no significant difference between the two groups in terms of other demographic variables such as BMI, education, occupation, marital status, income, housing, smoking, alcohol consumption and the amount of exercise during the week (P˃0.05). Comparison of fertility variables, including menarche age, menstrual pain score, duration of bleeding, history of infertility, type of delivery and contraceptive method showed no statistical difference between the two groups (P˃0.05).
Variable | Case group N = 45 Mean (SD) | Control group N = 40 Mean (SD) | P-value | |
|---|---|---|---|---|
Age* | 27.93 ((6.64 | (7.19)33.02 | 0.001 | |
BMI* | (3.93) 25.24 | (5.07)25.85 | 0.53 | |
Menarche age* | (1.46)13.15 | (1.51)13.57 | 0.19 | |
Score of dysmenorrhea* | (2.59)5.93 | (2.94)5.70 | 0.15 | |
Duration of bleeding* | (1.62)6.24 | (1.89)5.62 | 0.28 | |
Number of pregnancies* | (1.12)0.84 | (2.00)1.70 | 0.04 | |
Menstrual status** | Regular | Number (%) | Number (%) | 0.009 |
20 (44.4) | (72.5)29 | |||
Irregular | (55.6)25 | (27.5)11 | ||
Interval of menstruation** | ˂21 | 12.2)1) | 12.5)1) | 0.07 |
21–35 | (64.4)29 | (85)34 | ||
> 35 | (33.3)15 | (12.5)5 | ||
Dysmenorrhea** | Yes | (68.9)31 | (55)22 | 0.18 |
No | (31.1)14 | (45)18 | ||
Menorrhagia** | Yes | (31.1)14 | (22.5)9 | 0.37 |
No | (68.9)31 | (77.5)31 | ||
History of infertility** | No history of infertility | (93.3)42 | (95)38 | 0.38 |
Primary | 3 (6.7) | (2.5)1 | ||
Secondary | (0)0 | (2.5)1 | ||
Type of delivery** | No history of delivery | (55.6)25 | 20(50) | 0.83 |
NVD | (26.7)12 | (32.5)13 | ||
CS | (17.8)8 | (17.5)7 | ||
Contraception method** | OCP | (6.8)3 | (2.5)1 | 0.33 |
IUD | (2.3)1 | (5)2 | ||
Other | (36.4)16 | (52.5)21 | ||
Without | (54.5)24 | (40)16 | ||
Education** | ≤ 12 | 35(77.8) | 28(70) | 0.27 |
˂12 | 10(22.2) | 12(30) | ||
Occupation** | Housewife | (64.4)29 | (45)18 | 0.12 |
Employed | 16(35.6) | 22(55) | ||
Marital status** | Single | (37.8)17 | (25)10 | 0.26 |
Married | (60)27 | (75)30 | ||
Widow | (2.2)1 | 0(0) | ||
Income** | ˃2.5 | (33.3)15 | (15)6 | 0.10 |
2.5-5 | (42.2)19 | (45)18 | ||
> 5 | (24.4)11 | (40)16 | ||
Housing** | Privet | (71.1)32 | (67.5)27 | 0.71 |
Rental | (28.9)13 | (32.5)13 | ||
Smoking** | Yes | (8.9)4 | (10)4 | 0.86 |
No | (91.1)41 | (90)36 | ||
alcohol consumption ** | Yes | (6.66)3 | (7.5)3 | 0.54 |
No | (93.33)42 | (92.5)37 | ||
Exercise** | ˃1 | (71.2)32 | (77.5)31 | 0.76 |
3 − 1 | (24.4)11 | (20)8 | ||
˂3 | 2(4.4) | (2.5)1 | ||
Table 1: Examining the demographic and fertility characteristics in the case and control groups
* Values are given as Mean ± SD using the independent t-test.
** Values are given as number and percentage using the Chi square test.
As shown in Table 2, no significant difference was observed between the two groups in terms of calorie intake, dietary macronutrients and some micronutrients (P˃0.05), but there was a significant difference in daily food intake (in grams) between the two groups, which was higher in the control group (P˂0.05).
Variable | Case group (N = 45) Mean (SD) | Control group (N = 40) Mean (SD) | P-value* |
|---|---|---|---|
Daily food intake (in grams) | 2094.72(691.55) | 2546.83(539.66) | 0.02 |
Daily calorie intake (in kilocalories) | 2324.42(719.79) | 2687.70(709.53) | 0.11 |
Daily intake of protein | 80.74(27.47) | 96.46(28.57) | 0.77 |
Daily intake of carbohydrates | 342.39(115.07) | 387.16(109.69) | 0.26 |
Daily intake of total fat | 77.03(28.26) | 91.92(28.63) | 0.74 |
Daily intake of fiber | 57.97(26.75) | 68.17(27.00) | 0.20 |
Daily intake of cholesterol | 209.32(96.12) | 247.01(101.57) | 0.27 |
Daily intake of beta-carotene | 3425.18(2204.14) | 3862.22(2077.04) | 0.96 |
Daily intake of Vitamin C | 121.11(59.07) | 141.97(56.07) | 0.28 |
Daily intake of Vitamin E | 11.55(6.16) | 13.17(6.65) | 0.41 |
Daily intake of zinc | 11.74(4.5) | 14.20(4.3) | 0.11 |
Daily intake of glucose | 14.7(6.49) | 16.50(5.95) | 0.60 |
Daily intake of selenium | 129.50(64.26) | 148.98(54.64) | 0.32 |
Table 2: Examination of dietary intake and dietary macronutrients and micronutrients in the case and control groups
* Values are given as Mean ± SD using the analyze covariance test.
Table 3 illustrates comparative investigation of DII in the case and controls groups. As shown, no significant difference was observed between the two groups in terms of DII (P˃ 0.05).
Variable | Case group (N = 45) Mean (SD) | Control group (N = 40) Mean (SD) | P-value* |
|---|---|---|---|
DII | 4.11(1.51) | 4.36(0.44) | 0.68 |
Table 3: Examination of Dietary Inflammatory Index (DII) in the case and control groups
* Values are given as Mean ± SD using the analyze covariance test.
As displayed in Table 4, the serum level of Interleukin-6 was significantly higher in the case group than in the control group (P˂0.05); however, the difference between the two groups was not significant in terms of CRP.
Variable | Case group (N = 45) Mean (SD) | Control group (N = 40) Mean (SD) | P-value |
|---|---|---|---|
IL-6* | 4.94(1.97) | 3.48(1.77) | 0.001< |
CRP** |
|
| 0.62 |
Positive | (4.5)2 | (2.5 )1 | |
Negative | (95.5)43 | (97.5)39 | |
CRP; C - reactive protein | |||
Table 4: Comparison of the serum levels of Interleukin-6 and CRP between the case and control groups
* Values are given as Mean ± SD using the analyze covariance test.
* Values are given as number and percentage using the Chi square test
Pearson’s correlation test was used to investigate the relationship between DII and the inflammatory marker Interleukin-6. The results showed no significant correlation between these two parameters (P˃ 0.05).
Variable | IL6 |
|---|---|
DII | 0.96* |
* Values are given by Pearson’s correlation test | |
Table 5: Investigating the correlation between Interleukin-6 and DII
Discussion
This study was set out with the aim of investigating the possible association of Diet Inflammatory Index (DII) with the inflammatory markers like C-reactive protein (CRP) and Interleukin-6, and compare the obtained results in women with and without PCOS. Various studies have assessed the diet in women with PCOS; however, to the best of our knowledge, no study has assessed the association between DII and inflammatory markers in women with and without PCOS. According to the obtained results, the amount of daily food intake was significantly higher in non-PCOS women than in women with PCOS; however, the two groups of women did not have significant differences in daily calorie intake, protein, carbohydrate and total fat intake; this finding is consistent with the results of several other studies. Wright et al. (10) reported that no significant difference was observed between the case and control groups in food intake and physical activity. This finding also accords with the results of Alvarez et al. (11), who also reported that there was no significant difference in daily food intake and the intake of macronutrients and micronutrients in the diet of women with and without PCOS but the intake of white bread (with a higher glycemic index) was significantly higher in the PCOS group. Contrarily, in the study of Barr et al. (12), a higher amount of daily food intake was observed in women with PCOS compared to healthy women. There are several explanations for these conflicting results:
A) Studies evaluating the diet and physical activity of women with and without PCOS have used broad definitions of PCOS, which makes interpretation and comparison of different results challenging, because the group of women with PCOS consists of several distinct clinical phenotypes. Most of these studies have used the Rotterdam criteria. This may lead to creation of various and heterogeneous PCOS phenotypes; there are hormonal and metabolic differences among these clinical phenotypes, which may act as a confounding factor. These results are in agreement with the findings of Graff et al. (13), who reported certain differences in dietary intake among the clinical phenotypes of PCOS. As a matter of fact, women with mild phenotype of PCOS have different metabolic status and health risks compared to more severe phenotypes of PCOS (14). This fact pinpoints the need to make distinction between the different phenotypes of PCOS in order to accurately compare lifestyle habits, including nutrition between PCOS and non- PCOS women.
B) Energy balance is an important determinant of weight and has not been adequately addressed in the literature. To our knowledge, few studies have simultaneously assessed physical activity while examining diet in women with PCOS (15). Evidence suggests that depression or low self-esteem in PCOS women increases the risk of eating disorders and reduced physical activity (16). Therefore, one of the factors that can affect the relationship between diet and PCOS is mental health status in women.
One unanticipated finding in the present study was that there was no significant difference between the case and control groups in terms of DII. Contrary to this, Zirak Sharkesh et al. (17) found a higher DII score associated with a higher incidence of PCOS. Likewise, Whang et al. (18) reported that higher DII score had a positive correlation with the risk of PCOS. In accordance with the present research results, Zheng et al. (19) observed no significant difference in daily food intake and eating habits of obese and infertile PCOS women and obese non-PCOS women. The possible explanation for this finding might be that high carbohydrate intake, low-grade inflammation and hyperandrogenism interact to affect the pathophysiology of PCOS. In fact, higher carbohydrate consumption increases DII, and thus, increases the incidence of PCOS, (20) while, according to the of the present study results, the two groups did not differ in terms of carbohydrate intake. Gonzalez et al. (21, 22) outlined the key role of food ingredients such as glucose and saturated fatty acids in causing inflammation and production of androgens, even independent of obesity and insulin resistance. Based on the findings of Barrea et al. (23), the Mediterranean diet has been proposed as an anti-inflammatory food pattern that includes complex carbohydrates, fiber and fatty acids with a saturated chain. They found that patients with PCOS had higher consumption of simple carbohydrates, total fat and fatty acids. In addition, testosterone levels in patients with PCOS had a significant negative relationship with the intake of protein and complex carbohydrates. Moreover, a significant positive relationship was observed between CRP levels and the intake of simple carbohydrates. Gonzalez et al. (24) found evidence of increase in TNFa and Interleukin-6 in women with PCOS under both conditions of increased glucose consumption in vivo and exposure to glucose in vitro, which was associated with insulin resistance and shows that inflammation caused by diet in PCOS patients is probably related to glucose consumption and insulin resistance.
Diet is a key determinant of overweight and the relationship between diet and PCOS is influenced by geographical factors and various dietary patterns (25). The current research results support evidence from previous observations that reported no significant relationship between various dietary patterns, including the Mediterranean diet with PCOS, whereas, according to some other research results, it was expected that the Mediterranean diet, which has an inverse relationship with DII, would have a significant relationship with PCOS (26). In summary, one can conclude that a healthy diet with a sufficient ratio of complex to simple carbohydrates should be appropriate to end with weight loss and improve metabolic, hormonal and reproductive homeostasis in women with PCOS.
In the present study, a significant difference was observed in terms of Interleukin-6 inflammatory marker between the two groups of PCOS and non-PCOS women, which was higher in the PCOS women. This finding reflects those of Artimani et al., who also found that the level of the inflammatory marker Interleukin-6 was higher in PCOS patients compared to non-PCOS women (27). The study conducted by Zanganeh et al. showed that the serum levels of IL1a and IL1B in women with PCOS were higher, but IL17 levels in PCOS women were significantly lower than in the non-PCOS control group (28). This finding is contrary to the findings of Mohlig et al. in which the hypothesis of the relationship between PCOS and chronic inflammation was rejected. They found that neither CRP nor Interleukin-6 in obese and thin women with PCOS was different from their counterpart non-PCOS women (29). Obesity acts as a potential confounding factor of CRP increase, which can affect the process of inflammation and the level of inflammatory markers (30). Studies that assess the relationship between PCOS and inflammation and inflammatory markers might have several limitations. Most of these studies have small sample size and only women with approved diagnosis of PCOS based on the Rotterdam criteria are included in the study, which is the reason for the diversity in the study population due to the inclusion of different PCO phenotypes. The effect of obesity, especially visceral fat on inflammation is well known, and the results of most of these studies are not adjusted for the effect of obesity and other diseases affecting inflammation.
Our data demonstrated that there was no correlation between DII and Interleukin-6. Similarly, Kotemori et al. did not observe a relationship between DII and the level of CRP (31). Also, in a study conducted in the USA, despite the high level of CRP, no significant relationship was observed between CRP concentration and DII (32). Contrary to these results, some other studies in western societies have reported a positive and significant relationship between inflammatory markers and DII (33, 34). The diversity in habits and diet as well as the different spectrum of inflammatory status in different societies can be one of the reasons for reporting different results in these studies. Moreover, the drugs used by the subjects in some of these studies have been responsible for the positive relationship observed between DII and inflammatory markers (31).
There were several limitations with this study. The sample size was small and phenotypic division was not done in the PCOS group; so, it is suggested that future studies be conducted with larger sample sizes and create a clear distinction between the different phenotypes of PCOS. It would have been better if we had evaluated variables such as mental health status of participants as well as metabolic parameters.
Conclusions
Diet, especially carbohydrates and glucose are capable to trigger an inflammatory response, and thus, affect the incidence and severity of PCOS; however, as discussed earlier, this relationship is influenced by various factors such as clinical phenotypes of PCOS and mental health status. Therefore, in order to better examine and provide a suitable diet according to the conditions of each person, these factors should be taken into consideration in future studies.
Abbreviations
PCOS: Polycystic Ovary Syndrome PCO: Polycystic Ovaries CRP: C-Reactive Protein DII: Diet Inflammatory Index PI: Phytochemical Index FFQ: Food Frequency Questionnaire TNF: Tumor Necrosis Factor BMI: Body Mass Index
Declarations
Ethics approval and consent to participate:
Ethical clearance was sought from The Ethics Committee of Tarbiat Modares University of Medical Sciences (IR.MODARES.REC.1399.177). All study protocols were in accordance with the ethical standards of the Regional Research Committee, as well as the Declaration of Helsinki 1964 and its later amendments. After explaining the research purposes, informed written consent and verbal assent were obtained from all participants. They were also informed that their participation was voluntary, confidential, and anonymous and that they had the right to withdraw from the research at any time.
Consent for publication:
Not applicable
Availability of data and materials
The data sets used and analyzed for the current study are available upon reasonable request from the corresponding author, Dr. Shahideh Jahanian (shahideh.jahanian@modares.ac.ir).
Competing interests
The authors declare no conflicts of interest.
Funding
None.
Authors' contributions
Kh.A and Sh.JS contributed to the conception and design of the study; Kh.A, Sh.JS and A.M did the literature search; Sh.JS and M.N performed the statistical analysis; Kh.A, Sh.JS, M.N and A.M wrote the first draft of the manuscript. All authors contributed to the manuscript revision, and read and approved the submitted version.
Acknowledgments:
This study was carried out with the kind collaboration of the participants. It is a part of a research work done in Tarbiat Modares University, Tehran, Iran. We also appreciate Mr. Ebrahim Parvin for editing and proof-reading the final manuscript. There were no conflicts of interest.
References
- Lin LH, Baracat MC, Maciel GA, Soares Jr JM, Baracat EC. (2013), Androgen receptor gene polymorphism and polycystic ovary syndrome. International Journal of Gynecology & Obstetrics. 120(2):115-118.
View at Publisher | View at Google Scholar - Deswal R, Narwal V, Dang A, Pundir CS. (2020), The Prevalence of Polycystic Ovary Syndrome: A Brief Systematic Review. J Hum Reprod Sci. 13(4):261-271.
View at Publisher | View at Google Scholar - Palomba S, Santagni S, Falbo A, La Sala GB. (2015), Complications and challenges associated with polycystic ovary syndrome: current perspectives. Int J Womens Health. 7:745-763.
View at Publisher | View at Google Scholar - Aboeldalyl S, James C, Seyam E, Ibrahim EM, Shawki HE, et al. (2021), The Role of Chronic Inflammation in Polycystic Ovarian Syndrome-A Systematic Review and Meta-Analysis. Int J Mol Sci. 22(5).
View at Publisher | View at Google Scholar - González F. (2012), Inflammation in Polycystic Ovary Syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids. 77(4):300-305.
View at Publisher | View at Google Scholar - González F, Minium J, Rote NS, Kirwan JP. (2005), Hyperglycemia alters tumor necrosis factor-alpha release from mononuclear cells in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 90(9):5336-5342.
View at Publisher | View at Google Scholar - Lass N, Kleber M, Winkel K, Wunsch R, Reinehr T. (2011), Effect of lifestyle intervention on features of polycystic ovarian syndrome, metabolic syndrome, and intima-media thickness in obese adolescent girls. J Clin Endocrinol Metab. 96(11):3533-3540.
View at Publisher | View at Google Scholar - Berrino F, Bellati C, Secreto G, Camerini E, Pala V, et al. (2001), Reducing bioavailable sex hormones through a comprehensive change in diet: the diet and androgens (DIANA) randomized trial. Cancer Epidemiol Biomarkers Prev. 10(1):25-33.
View at Publisher | View at Google Scholar - Asghari G, Rezazadeh A, Hosseini-Esfahani F, Mehrabi Y, Mirmiran P, et al. (2012), Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br J Nutr. 108(6):1109-1117.
View at Publisher | View at Google Scholar - Wright CE, Zborowski JV, Talbott EO, McHugh-Pemu K, Youk A. (2004), Dietary intake, physical activity, and obesity in women with polycystic ovary syndrome. Int J Obes Relat Metab Disord. 28(8):1026-1032.
View at Publisher | View at Google Scholar - Álvarez-Blasco F, Luque-Ramírez M, Escobar-Morreale HF. (2011), Diet composition and physical activity in overweight and obese premenopausal women with or without polycystic ovary syndrome. Gynecol Endocrinol. 27(12):978-981.
View at Publisher | View at Google Scholar - Barr S, Hart K, Reeves S, Sharp K, Jeanes Y. (2011), Habitual dietary intake, eating pattern and physical activity of women with polycystic ovary syndrome. European Journal of Clinical Nutrition. 65(10):1126-1132.
View at Publisher | View at Google Scholar - Graff SK, Mário FM, Alves BC, Spritzer PM. (2013), Dietary glycemic index is associated with less favorable anthropometric and metabolic profiles in polycystic ovary syndrome women with different phenotypes. Fertility and Sterility. 100(4):1081-1088.
View at Publisher | View at Google Scholar - Pikee S, Shivani S, Jayshree B. (2016), Endocrine and metabolic profile of different phenotypes of polycystic ovarian syndrome. The Journal of Obstetrics and Gynecology of India. 66:560-566.
View at Publisher | View at Google Scholar - Lin AW, Lujan ME. (2014), Comparison of dietary intake and physical activity between women with and without polycystic ovary syndrome: a review. Advances in Nutrition. 5(5):486-496.
View at Publisher | View at Google Scholar - Lee I, Cooney LG, Saini S, Sammel MD, Allison KC, et al. (2019), Increased odds of disordered eating in polycystic ovary syndrome: a systematic review and meta-analysis. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 24:787-797.
View at Publisher | View at Google Scholar - Zirak Sharkesh E, Keshavarz SA, Nazari L, Abbasi B. (2022), The dietary inflammatory index is directly associated with polycystic ovary syndrome: A case‐control study. Clinical Endocrinology. 96(5):698-706.
View at Publisher | View at Google Scholar - Wang Q, Sun Y, Xu Q, Liu W, Wang P, et al. (2022), Higher dietary inflammation potential and certain dietary patterns are associated with polycystic ovary syndrome risk in China: A case-control study. Nutrition Research. 100:1-18.
View at Publisher | View at Google Scholar - Wang Z, Groen H, Cantineau AE, van Elten TM, Karsten MD, et al. (2021), Dietary intake, eating behavior, physical activity, and quality of life in infertile women with PCOS and obesity compared with non-PCOS obese controls. Nutrients. 13(10):3526.
View at Publisher | View at Google Scholar - Barrea L, Marzullo P, Muscogiuri G, Di Somma C, Scacchi M, et al. (2018), Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutrition Research Reviews. 31(2):291-301.
View at Publisher | View at Google Scholar - Gonzalez F, (2015), editor Nutrient-induced inflammation in polycystic ovary syndrome: role in the development of metabolic aberration and ovarian dysfunction. Seminars in reproductive medicine; Thieme Medical Publishers.
View at Publisher | View at Google Scholar - González F, Sia CL, Shepard MK, Rote NS, Minium J. (2014), The altered mononuclear cell-derived cytokine response to glucose ingestion is not regulated by excess adiposity in polycystic ovary syndrome. The Journal of Clinical Endocrinology & Metabolism. 99(11): E2244-E51.
View at Publisher | View at Google Scholar - Barrea L, Arnone A, Annunziata G, Muscogiuri G, Laudisio D, et al. (2019), Adherence to the mediterranean diet, dietary patterns and body composition in women with polycystic ovary syndrome (PCOS). Nutrients. 11(10):2278.
View at Publisher | View at Google Scholar - González F. (2012), Inflammation in polycystic ovary syndrome: underpinning of insulin resistance and ovarian dysfunction. Steroids. 77(4):300-305.
View at Publisher | View at Google Scholar - Merkin SS, Phy JL, Sites CK, Yang D. (2016), Environmental determinants of polycystic ovary syndrome. Fertility and Sterility. 106(1):16-24.
View at Publisher | View at Google Scholar - Hodge A, Bassett J, Shivappa N, Hébert J, English D, et al. (2016), Dietary inflammatory index, Mediterranean diet score, and lung cancer: a prospective study. Cancer Causes & Control. 27:907-917.
View at Publisher | View at Google Scholar - Artimani T, Karimi J, Mehdizadeh M, Yavangi M, Khanlarzadeh E, et al. (2018), Evaluation of pro-oxidant-antioxidant balance (PAB) and its association with inflammatory cytokines in polycystic ovary syndrome (PCOS). Gynecological Endocrinology. 34(2):148-152.
View at Publisher | View at Google Scholar - Zangeneh FZ, Naghizadeh MM, Masoumi M. (2017), Polycystic ovary syndrome and circulating inflammatory markers. International Journal of Reproductive BioMedicine. 15(6):375.
View at Publisher | View at Google Scholar - Möhlig M, Spranger J, Osterhoff M, Ristow M, Pfeiffer A, et al. (2004), The polycystic ovary syndrome per se is not associated with increased chronic inflammation. European Journal of Endocrinology. 150(4):525-532.
View at Publisher | View at Google Scholar - Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. (2017), Obesity and inflammation: the linking mechanism and the complications. Archives of Medical Science. 13(4):851-863.
View at Publisher | View at Google Scholar - Kotemori A, Sawada N, Iwasaki M, Yamaji T, Shivappa N, et al. (2021), Dietary inflammatory index is associated with inflammation in Japanese men. Frontiers in Nutrition. 8:604296.
View at Publisher | View at Google Scholar - Tabung FK, Steck SE, Zhang J, Ma Y, Liese AD, et al. (2015), Construct validation of the dietary inflammatory index among postmenopausal women. Annals of Epidemiology. 25(6):398-405.
View at Publisher | View at Google Scholar - Shivappa N, Steck SE, Hurley TG, Hussey JR, Ma Y, et al. (2014), A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutrition. 17(8):1825-1833.
View at Publisher | View at Google Scholar - Shivappa N, Wirth MD, Hurley TG, Hébert JR. (2017), Association between the dietary inflammatory index (DII) and telomere length and C‐reactive protein from the National Health and Nutrition Examination Survey‐1999–2002. Molecular Nutrition & Food Research. 61(4):1600630.
View at Publisher | View at Google Scholar

 Clinic
Clinic
