Research article | DOI: https://doi.org/10.31579/2834-5126/033
Analysis of Cases of Giant Epidural Haemorrhages Underwent Evacuation in the Rural Hospital
- Sajag K. Gupta 1*
Assistant Professor, Neurosurgery Upums Saifai Etawah (u.p), India
*Corresponding Author: Sajag Kumar Gupta, Assistant Professor, Neurosurgery Upums Saifai Etawah (u.p) India.
Citation: Sajag K. Gupta (2023), Analysis of Cases of Giant Epidural Haemorrhages Underwent Evacuation in the Rural Hospital, Clinical Trials and Clinical Research. 2(4); DOI:10.31579/2834-5126/033
Copyright: © 2023, Sajag Kumar Gupta. this is an open access article distributed under the creative commons’ attribution license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 15 June 2023 | Accepted: 26 June 2023 | Published: 03 July 2023
Keywords: clinical trials; Africa; socio-politics; framework; stakeholders
Abstract
This analysis looks at surgical instances with giant epidural haemorrhages that have a significant influence on therapeutic as well as clinical prognosis.
Methods: Between January 1, 2022, and March 31, 2023, 112 peoples were undergone surgery for epidural haemorrhage at the Neurosurgical Department at UPUMS SAIFAI ETAWAH, U.P, a rural hospital. We defined Giant epidural haemorrhage as a quantity of more than 80 cc. The therapeutic and prognostic features of 15 people with giant Epidural haemorrhage with a haematoma amount of 80 cc were studied further.
Results: The most prevalent age grouping varies between the ages of 20 to 40(53.33%). Motor response 2 (60%) represented the much frequent motor movement among giant Epidural haemorrhage victims who underwent surgery. The vast majority of them (86.66%) suffered from serious brain damage. The G.C.S. at the presentation, pupil alterations, motor movement were all associated to the prognosis of giant Epidural haemorrhage surgery.
Conclusion: Gigantic Epidural haemorrhage with an amount of more than 80 cc performs badly. The Glasgow coma scale at presentation, pupil alterations, and motor movement are all markers of the operative prognosis of a large epidural haemorrhage.
Introduction
Epidural Haemorrhage is a haematoma accumulation that form between the dura and bone. It is most commonly produced by a rupture of the M.M.A, but it can also be caused by a rupture of the
A.dural venous sinuses,
B. vein in the meningeal layer,
C. diploic vein
D. fracture line haemorrhage.
It nearly invariably has trauma as aetiology and is generally linked with a skull fracture. [1] Epidural Haemorrhages are responsible for 5-15% of dangerous brain traumas. [2] The CT head is the preferred examination for detecting brain damage following trauma. [3] CT head also detects other factors that influence the surgical outcome, such as
A.M.L.S (midline shift),
B.traumatic SAH (subarachnoid haemorrhage)
C. obliterated of the (basal cisterns)
D. haematoma size
E.volume of clot,
F.contusion, and
G.skull bone fracture. Local ischemia produced by the mass impact, direct head injury, or obstructed venous return is mostly responsible for the related brain impairment. Ischemic brain injury is a significant prognostic indicator in the pathophysiology of Epidural Haemorrhage and may be caused by the hematoma's mass effects and elevated intracerebral pressures (I.C.P), resulting in impaired cerebral perfusion pressures (C.P.P). Apart from Epidural Haemorrhage, the underlying brain damage is responsible for impaired neurology function following trauma. The outcome of Epidural Haemorrhage is mostly determined by the G.C.S. at presentation and neurology state. [4] Gigantic or massive Epidural Haemorrhage [Figures 1 a,b,c,d] is an epidural collection large enough to produce an abrupt M.L.S., brain herniation, and pressure over brainstem, resulting in patient death. It is an emergency that necessitates the immediate removal of Epidural Haemorrhage and stabilisation of the patient. Many comorbidities, concurrent brain impairment, ischemic brain, antiplatelet, anticoagulant medication, and old age people all influence the surgical prognosis of Epidural Haemorrhage. It is critical to correctly identify outcome-predicting markers in order to provide appropriate surgical treatment. In this analysis, we looked at the effect of giant or huge Epidural Haemorrhage, which produces a considerable acute worsening of the neurology condition and a negative prognosis. It also intends to examine large Epidural Haemorrhage peoples who underwent surgery for a therapeutic and prognosis standpoint.
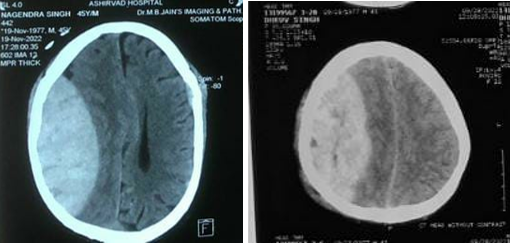
Figure 1: a right-sided Giant EDH of 45-year male Figure 1:b right-sided giant EDH of 26-year male
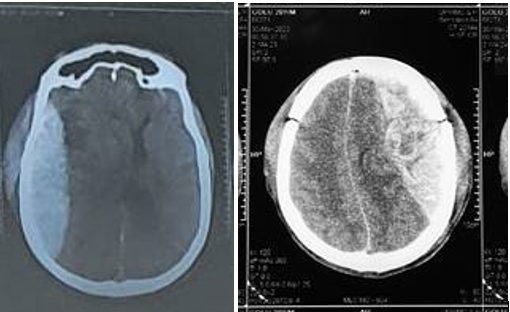
Figure 1:C right sided Giant EDH of 29year male Figure 1: d left-sided giant EDH of 36-year male
Material and Method
This retrospective study between January 1, 2022, and 31st March 2023 including 112 people who underwent surgery for Epidural Haemorrhage in an emergency in the Neurosurgical Department of UPUMS SAIFAI ETAWAH, U.P, a rural hospital. Analysis of 112 people was done for the evaluation of giant Epidural Haemorrhage target amount. We had considered > 80 cc as a target amount to be considered as Giant Epidural Haemorrhage. Based on this data, 15 people with giant Epidural Haemorrhage with haematoma amount of 80 cc were evaluated clinically, surgically, and for outcome in view of Age group, gender, mode of trauma, motor response, severity of injury, location of haemorrhage, presentation, CT findings, amount of clot evacuated, source of bleed, and prognosis at discharge/death were all assessed in each patient with massive Epidural Haemorrhage. All victims admitted to the neurosurgical department at UPUMS Saifai Etawah, U.P, met the criteria of inclusion. Patients with Epidural Haemorrhage amount more than 80 CC who received surgery within the first two hours after arriving at the trauma centre were included in the research. The criteria of exclusion included insufficient data for the research variables, conservatively treated Epidural Haemorrhage patients, and refusal to consent to surgery. Craniotomy with Epidural Haemorrhage evacuation was the surgical procedure employed. Craniectomy was performed in situations with temporal Epidural Haemorrhage or comminuted skull fracture. FFP was utilised to correct the INR in anticoagulation medication patients, while pools of platelets were used in antiplatelet medication patients based on neurosurgeon choice. H.I.C.U care was offered following surgery. All performed cases received informed permission from victims or victim relatives (in cases, in which the patient was not able to consent, namely, low Glasgow coma scale). Dataset were gathered retrospectively by analysing medical, surgical, and radiological data from 112 operated peoples who were submitted to the UPUMS medical record department. Statistical tests were done using GraphPad Prism version 8.3.0 software. P value was taken at 0.05. Null hypothesis of no significant difference in mean and alternative hypothesis of significant difference between means was taken. Outcome analysis of giant EDH was done using Pearson’s Chi-square test and one-way ANOVA test. The Peterson and Espersen equation was used to compute the amount of the Epidural Haemorrhage. [5] Epidural Haemorrhage volume = X Y Z 0.5 Where X, Y, and Z denoted the hematoma's sizes in the sagittal, axial, and coronal planes, respectively.
Results
Analysis of giant Epidural Haemorrhage (amount ≥ 80 CC) Age distribution in this research, the mostly patients who underwent evacuation for giant Epidural Haemorrhage were in the age group of 20–40 (n = 8, 53.33%) follows the age group of 40–60 (n = 3, 20%) [Table 1]
| AGE | <20> | 2 | 13.33% |
| 20-40 | 8 | 53.33% | |
| 40-60 | 3 | 20% | |
| >60 | 2 | 13.33% | |
| SEX | male | 14 | 93.33% |
| female | 1 | 6.66% |
Table 1: Age and sex distribution.
Sex distribution in this research, mostly patients who underwent surgery for giant Epidural Haemorrhage were males (n = 14, 93.33%). Male-to-female ratio was 14:1 [Table 1]. Mode of injury in this research, mostly mode of injury was RTA (n = 10, 66.66%) followed by assault (n = 4, 26.66%) and fall from height (n = 1, 6.66%). motor response (M status) In this research, mostly M status was M2 (n = 9, 60 %) followed by M3 (n = 4, 26.66 %) and M4 (n = 2, 13.33%), respectively. The severity of injury In this research, victims with giant Epidural Haemorrhage were having moderate, G.C.S 9–13, (n = 2, 13.33%) and severe, G.C.S ≤ 8 (n = 13, 86.66 %). No patient was having a mild head injury, GCS 14–15. Clinical signs in this research, pupil alteration (bilateral) were present in 8 patients (53.33%), pupil alteration (unilateral) was present in 5 patients (33.33%), and bradycardia was present in 7 patients (46.66%). Site of giant EDH In this research, the most common site of giant Epidural Haemorrhage was frontotemporoparietal (n=10, 66.66%) follows frontoparietal (n = 4, 26.66%) and parietal (n = 1, 6.66%) [Table 2].
Side of giant Epidural Haemorrhage In this research, the right-sided giant Epidural Haemorrhage was present in 7 victims (46.66%), left-sided giant Epidural Haemorrhage in 6 victims (40%), and bilateral giant Epidural Haemorrhage was seen in 2 victims (13.33%)
| Bilateral | 2 | 13.33% |
| Right | 7 | 46.66% |
| Left | 6 | 40% |
| Front temporoparietal | 10 | 66.66% |
| Frontoparietal | 4 | 26.66% |
| Parietal | 1 | 6.66% |
Table 2: Site and side of giant Epidural Haemorrhage
Source of bleeding in giant Epidural Haemorrhage In this research, the source of bleed was dural venous sinus bleed in 12 patients (80%) followed by middle meningeal arterial bleed in 3 patients (20%) [Table 3]. The amount of haematoma evacuated during surgery Intraoperative clot evacuated was >140 cc in 7 patients (46.66%), 120–140 cc in 5 patients (33.33%), 100–120 cc in 2 patients (13.33%), and 80–90 cc in 1 patient (6.66%). CT findings In all patients, M.L.S and brain herniation were present. G.O.S In this study, G.O.S of 1 was observed in 8 patients (53.33%), G.O.S of 2 was seen in 3 patients (20%), G.O.S of 3 was seen in 2 patients (13.33%), G.O.S of 4 was seen in 1 patient (6.66%), and G.O.S of 5 was seen in 1 patient (6.66 %). In this study, we found that G.C.S at presentation, pupil alteration and motor response was significantly associated with outcome following surgery for giant Epidural Haemorrhage. In contrast, age, gender of patients, and severity of injury were not found to be associated with outcomes following surgery [Table 4].
| dural venous sinus bleeding | 12 | 80% |
| middle meningeal arterial bleeding | 3 | 20% |
Table 3: Source of bleed in giant Epidural Haemorrhage.
| characteristics | G.O.S 1 (n=8) | G.O.S 2 (n=3) | G.O.S 3 (n=2) | G.O.S 4 (n=1) | G.O.S 5 (n=1) | P VALUE | |
| Age | 43.1 | 31 | 31.2 | 34 | 20 | 0.4217 | |
| Gender (%) | Male Female | 8 0 | 2 1 | 2 0 | 1 0 | 1 0 | 0.3955 |
| Mode of injury | RTA=10 FFH=1 Assault=4 | 6 1 1 | 2 0 1 | 1 0 1 | 0 0 1 | 1 0 0 | 0.5777 |
| motor response | 1.8 | 2.8 | 3.5 | 4 | 5 | <0> | |
| Pupil changes | 8 | 3 | 2 | 0 | 0 | 0.0021 | |
| Severity of trauma | Mild Moderate severe | 0 0 8 | 0 0 3 | 0 0 2 | 0 1 0 | 0 1 0 | 0.8242 |
| G.C.S at presentation | 3.8 | 4.5 | 5.7 | 11 | 13 | <0> |
Statistically significant p<0>
Table 4: Variables of operated giant Epidural Haemorrhage cases – Glasgow outcome score
Discussion
Epidural Haemorrhage are commonly found in the region a skull fracture. Epidural Haemorrhage generation is normally quick within a few hours damage, although it might have a delayed course that is diagnosed days later. [6] Giant Epidural Haemorrhage, also known as massive Epidural Haemorrhage EDH, is an epidural collection large enough to induce sudden midline displacement, brain herniation, and pressure over brainstem, ultimately resulting to the victim’s death. This is an emergency that necessitates the immediate evacuation of the Epidural Haemorrhage and stabilisation of the patient. The ages of victims who had massive Epidural Haemorrhage surgery ranges from 6 to 75 years. The 20–40-year age group (n = 8, 53.33%) had the largest number of casualties, following the 40 to 60-year age group (n = 3, 20%). There is a scarcity of datasets in the scientific evidence on the age distribution patterns of giant Epidural Haemorrhage. However, in the published studies that included all Epidural Haemorrhages, the most of Epidural Haemorrhage was in the second decades, and the mean ages of victims with Epidural Haemorrhage were between 20 to 30 years old. [7,8] With giant Epidural Haemorrhage victims, we have a similar trend of age distribution. The M:F ratio of 14:1 in the current research reflects our social milieu, in which most ladies are not exposed to outside jobs. In individuals with giant Epidural Haemorrhage, we discovered male predominance (n = 14, 93.33%) over female victims (n = 1, 6.66%). There is a scarcity of research on sex predominance in patients with giant Epidural Haemorrhage. Male predominance over females is identified in the documented series of all Epidural Haemorrhage cases. [9] We see a similar type of male predominance in our giant Epidural Haemorrhage research groups.
Road traffic accidents (RTAs) were the much prevalent source of trauma in this research (n = 10, 66.66%), follows assault (n = 4, 26.66%), resulting in the development of giant Epidural Haemorrhage. It is comparable to several other published datasets [8,9] that cover all Epidural Haemorrhage patients. As compared to other places, Epidural Haemorrhage is more commonly seen in the temporoparietal and temporal regions in diverse reported series. [10,11] There is a scarcity of material about the location of the giant Epidural Haemorrhage. According to our data, giant Epidural Haemorrhage is most common in the front temporoparietal area (n = 10, 66.66%), follows the frontoparietal (n = 4, 26.66%) then parietal regions (n = 1, 6.66%). In the temporal area, Epidural Haemorrhage has been linked to a high rate of death.
[11] In this investigation, the motor response of M2 was reported in 9 patients (60%) followed by M3 (n = 4, 26.66%) and M4 (n = 2, 13.33%). Poor outcomes were seen in operated patients with low M status. In Epidural Haemorrhage patients, the best motor response at presentation has been found as a crucial determinant affecting outcome. [12,13] The majority of the head injury patients leading to giant Epidural Haemorrhage in our investigation were severe (n = 13, 86.66%), followed by moderate (n = 2, 13.33%) head injuries. Bilateral pupil alterations (n = 8, 53.33%) along with unilateral pupil alteration (n = 5, 33.33%) in victims of giant Epidural Haemorrhage suggest brain herniation as well as pressure over the brainstem caused by the giant Epidural Haemorrhage. Bradycardias were found in 7 (46.66%) of the victims and were also suggestive of brainstems compressions. In our research, the most prevalent source of bleed resulting from a large Epidural Haemorrhage was a Dural venous sinues bleed (n = 12, 80%), follows by MMA middle meningeal arterial bleed (n = 3, 20%). In recent research of 102 paediatric victims along with 387 adults with Epidural Haemorrhage, arterial bleed was found as the cause of Epidural Haemorrhage in 36% of adults and 18% of children. [11] According to research, low GCS, concomitant cerebral lesions, pupil alteration, and elevated I.C.P are independent indicators of low outcome. [3,14] G.C.S prior to surgery is a significant predictor of operative outcome. [3,14] Age, haematoma size, and Epidural Haemorrhage location were all important variables in other studies. It was discovered that pupil alteration and a lower GCS score (9) were connected with a bad prognosis. [15] In this research, the important clinical factors linked with a poor outcome were G.C.S at presentation, motor response, and pupil state. Age, sex, severity of damage was not shown to be substantially linked with treatment outcomes giant Epidural Haemorrhage surgery.
The single most important predictor of prognosis in patients with Epidural Haemorrhage
receiving surgery is G.C.S at presentation or G.C.S prior to surgery.[16] There were 8 deaths (53.33%) in this trial, with a Glasgow outcome scale of 1. These findings point to bad outcomes and increased death in victims with large Epidural Haemorrhage (>80 cc). There is a scarcity of research on the postoperative expiry of giant Epidural Haemorrhage. One of the patients got an infarct after surgery and died (Figure 2)
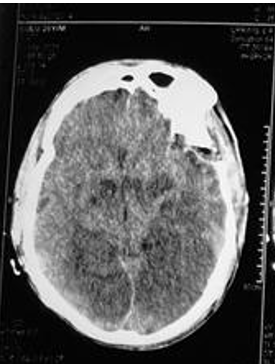
Figure 2: postoperatively CT head showing infarct
Conclusion
We concluded that this research that a giant Epidural Haemorrhage with amount of more than >80 cc produces instantaneous M.L.S, brain herniation, along with pressure over brainstem, resulting in a higher proportion of death. Early removal of a giant Epidural Haemorrhage is associated with a good result. In victims with giant Epidural Haemorrhage, poor Glasgow coma scale at presentation, poor motor response, and pupil alterations are related to bad outcomes. Some notable characteristics include male predominance with a M: F ratio of 14:1 and mostly in the active aged group 20 to 40 years.
Conflicts of Interest
The author declares no conflicts of interest regarding the publication of
Funding and support: No
Ethical consideration- approval was taken from institutional ethical committee code EC 23-008 for this paper.
References
- Rengachary SS, Ellenbogen RG. (2004). Principles in Neurosurgery. 2nd ed. India: Elsevier, Mosby, 2081.
View at Publisher | View at Google Scholar - McCrory P, Meeuwisse W, Johnston K, Dvorak J, Aubry M, Molloy M, et al. (2009). Consensus statement on concussion in sport: The 3rd international conference on concussion in sport held in Zurich, 2008. Br J Sports Med, 43 1:6-90.
View at Publisher | View at Google Scholar - Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, et al. (2006). Surgical management of acute epidural haematomas. Neurosurgery,58:52-57.
View at Publisher | View at Google Scholar - Haselsberger K, Pucher R, Auer L. (1988). Prognosis after acute subdural or epidural haemorrhage. Acta Neurochir (Wien), 90:111-116.
View at Publisher | View at Google Scholar - Petersen OF, Espersen JO. (1984). Extradural hematomas: Measurement of size by volume summation on CT scanning. Neuroradiology, 26:363-367
View at Publisher | View at Google Scholar - Carlos UP, Joas DB, Carneiro L, Antonio R, Egmond ASS, Joas TSM. (2005). Epidural haematoma: Analysis of 30 cases. Internet J Emerg Med, 2:44-47.
View at Publisher | View at Google Scholar - Haselsberger K, Pucher R, Auer L. (1988). Prognosis after acute subdural or epidural haemorrhage. Acta Neurochir (Wien), 90:111-116.
View at Publisher | View at Google Scholar - Jones N, Molloy C, Kloeden C, North J, Simpson D. (1993). Extradural haematoma: Trends in outcome over 35 years. Br J Neurosurg, 7:465-471.
View at Publisher | View at Google Scholar - Joom AJ. (1997). The difference in the outcome of surgery for traumatic extradural haematoma between patients who are admitted directly to the neurosurgical unit and those referred from another hospital. Neurosurg Rev, 20:227-230
View at Publisher | View at Google Scholar - Chowdhury NK, Raihan MZ, Chowdhury FH, Ashadullah AT, Sarkar MH, Hossain SS. (2008). Surgical management of traumatic extradural haematoma: Experiences with 610 patients and prospective analysis. Indian J Neurotrauma ,5:75-79.
View at Publisher | View at Google Scholar - Mohanty A, Kolluri VR, Subbakrishna DK, Satish S, Chandramouli BA, Das BS. (1995). Prognosis of extradural haematomas in children. Pediatr Neurosurg, 23:57-63.
View at Publisher | View at Google Scholar - Ersahin Y, Mutluer S, Guzelbag E. (1993). Extradural Haematoma analysis of 146 cases. Childs Nerv Syst ,9:96-97.
View at Publisher | View at Google Scholar - Faheem M, Jaiswal M, Ojha BK, Chandra A, Singh SK, Srivastava C. (2019). Traumatic pediatric extradural hematoma: An institutional study of 228 patients in tertiary care center. Pediatr Neurosurg ,54:237-244.
View at Publisher | View at Google Scholar - Lee EJ, Hung YC, Wang LC, Chung KC, Chen HH. (1998). Factors influencing the functional outcome of patients with acute epidural haematomas: Analysis of 200 patients undergoing surgery. J Trauma, 45:946-952
View at Publisher | View at Google Scholar - Dubey A, Pillai SV, Kolluri SV. (2004). Does volume of extradural hematoma influence management strategy and outcome? Neurology India,52:443-445.
View at Publisher | View at Google Scholar - Uzkan U, Kemaloglu S, Ozates M, Guzel A, Tath M. (2007). Analyzing extradural haematomas: A retrospective clinical investigation. Dicle Med J, 34:14-19.
View at Publisher | View at Google Scholar

 Clinic
Clinic
