Research Article | DOI: https://doi.org/10.31579/2834-8745/014
Pancreatic Diseases and Diabetes
1Riggs Pharmaceuticals, Department of Pharmacy, University of Karachi, Pakistan.
2Fazaia Ruth Pfau Medical College, Shahrahe Faisal Karachi, Pakistan.
3GD Pharmaceutical Inc OPJS University Rajasthan India.
4Assistant Professor, Dow university of Health sciences Karachi Pakistan.
*Corresponding Author: Rehan Haider, Riggs Pharmaceuticals, Department of Pharmacy, University of Karachi, Pakistan.
Citation: Rehan Haider, Asghar Mehdi, Geetha Kumari Das, Zameer Ahmed, (2024), Exploratory Factor Model of Perceived Harassment in the Covid-19 Era,Journal of Scientific Research and Biomedical Informatics, 3(2); DOI: 10.31579/2834-8745/014
Copyright: © 2024, Rehan Haider. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 04 March 2024 | Accepted: 12 March 2024 | Published: 20 March 2024
Keywords: pancreatic disease; diabetes; pancreatitis; pancreatic cancer; pancreatic cysts; type 1 diabetes; type 2 diabetes; gestational diabetes
Abstract
Pancreatic disease and diabetes are health challenges that considerably impact all-encompassing public health. Organ meat, a living organ accompanying endocrine and exocrine functions, plays an important function in maintaining sweet substance equilibrium. Disturbances in pancreatic function can lead to different afflictions, including diabetes mellitus. Diabetes mellitus, characterized by raised levels of glucose in the blood, is a chronic metabolic disorder with deep implications for things and healthcare schemes. Type 1 diabetes results from autoimmune destruction of insulin-bearing being tested containers in the pancreas, while Type 2 diabetes includes insulin opposition and impaired testing container function. Both types contribute to unending obstacles, moving the cardiovascular system, kidneys, eyes, and central nervous system. Pancreatitis, an instigative condition of the pancreas, is another important pancreatic disease. Acute pancreatitis is frequently provoked by gallstones or overdone alcohol use, while incessant pancreatitis results from prolonged swelling and fibrosis. Pancreatic malignancy, a formidable virulence, is a guide to an extreme mortality rate, generally on account of late-stage diagnosis and restricted situational options. The elaborate connection between pancreatic diseases and diabetes is versatile. Chronic pancreatitis concedes the possibility of leading to diabetes on account of the devastation of pancreatic tissue and jeopardized insulin results. Moreover, people with diabetes face a higher risk of developing pancreatic cancer. Understanding latent systems and shared risk determinants is critical for expanding effective stop and administration strategies
Introduction
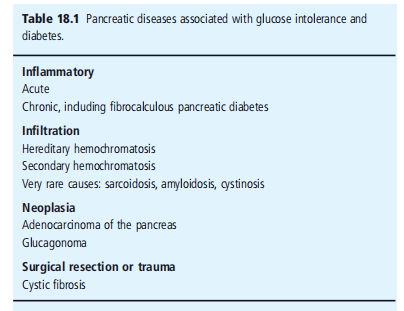
Acute pancreatitis: The consequences of pancreatitis on organ meat can manifest across a range, ranging from temperate sensitivity to hemorrhagic loss [1]. The dispassionate performance changes from mild to harsh, accompanying instances of loss. Notably, intoxicating devouring, specifically in individuals accompanying crapulence, is conspicuous as the ultimate low cause of pancreatitis. Another meaningful cause is gallstone disorder. Further analyses are determined in Table 18.1 [1]
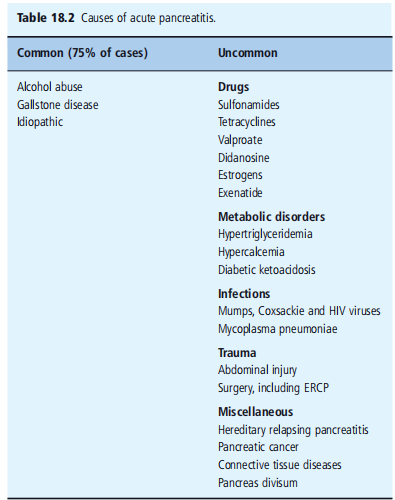
Pancreatitis frequently presents accompanying unexpected and surprising attacks. During physical examinations, accepted manifestations involve inferior turmoil, heart attack, and hypotension. In some cases, jaundice concedes the possibility of further being noticed. Severe pain in the wrist (Karen's sign) or the side of the crowd (Gray Turner's sign) can display the severity of the condition. Metabolic disorders usually associated with pancreatitis contain hyperglycemia, hypocalcemia, hyperlipidemia, hypoalbuminemia, and clotting issues [2] Elevated levels of antitoxin amylase and lipase are repeatedly found, even though their senses and specificities are nearly depressed. Imaging techniques in the way that computed tomography (CT) and magnetic resonance imaging (MRI) can disclose pancreatic redness. The presence of pancreatic loss grants permission to be recorded as a loss of augmentation on active CT scans. It is valuable to notice that patients with pancreatitis frequently experience hyperglycemia, which is attributed to raised glucagon levels. Damage to suspect containers in the pancreas has been further submitted as a donating factor [3]. Hyperglycemia guide pancreatitis is usually temperate and tends to resolve inside the moment of truth or any weeks without insulin healing. Please confer with Table 18.2 for further facts.
Chronic diabetes is exceptional and occasionally happens in cases of fulminant affliction and multi-means deterioration, with an occurrence rate of about 25% [4]. A glucose level above 11.1 mmol/L (200 mg/dL) following in position or time 24 hours frequently indicates a remote possibility [5]. In diabetic ketoacidosis, there may be non-particular elevations in antitoxin amylase and lipase levels [6]. It is worth noticing that pancreatitis can still influence up to 11% of subjects accompanying ketoacidosis, generally accompanying gentle or no abdominal pain.
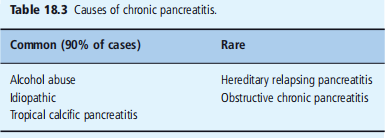
Chronic pancreatitis: This condition is a growing and irreversible devastation of the exocrine pancreatic fabric, happening in exocrine pancreatic insufficiency and variable points of glucose prejudice, frequently requiring insulin. The causes of never-ending pancreatitis can change based on the terrestrial area (see Fig. 18.3)
Etiological Factors:
Alcohol abuse remains the ruling cause of chronic pancreatitis in Western communities, accounting for over 85% of cases. Prolonged intoxicating consumption can change pancreatic secretions, resulting in the composition of proteinaceous plugs that obstruct ducts and serve as sites for mass in gallbladder composition. It's still noteworthy that lush pancreatitis is an additional condition not always connected to overdone intoxicating intake and is widespread everywhere [7].
Hereditary Chronic Pancreatitis:
An interesting condition inherited in autosomal main conduct, hereditary incessant pancreatitis includes mutations in various genes, including PRSS1 (cationic trypsinogen), SPINK1 (serine protease prevention, Kazal type 1), and cystic fibrosis transmembrane conveyance manager (CFTR) [8–11].
Obstructive Chronic Pancreatitis:
A rare condition results from pancreatic channel obstruction due to tumors, hurting, fake cysts, or inborn anomalies. Stones cannot arrive in specific cases, and treatment usually includes a surgical attack and endoscopic dilation for curative purposes.
Idiopathic Pancreatitis:
Accounting for 10–20% of all cases, basic pancreatitis can influence individuals of indifferent age groups. Two apparent age ranges are usually associated with allure attacks: 15–25 years and 55–65 years.Cigarette hot is a perilous determinant, and certain deoxyribonucleic acid mutations have existed projected as potential subscribers [11, 13-14].
Epidemiology:
Chronic pancreatitis is a widespread global condition, affecting nearly four cases per 100,000 people in Western countries. Chronic sultry pancreatitis is mainly about equatorial and subtropical domains worldwide.
Pathologic Features:
In Western nations, over 95% of never-ending pancreatitis cases exhibit characteristic pathologic changes expressed as "never-ending calcific pancreatitis." The pancreatic ducts and acini are suffused with proteinaceous plugs that withstand hardening and form narrow minerals, primarily calcium carbonate or calcite. A microscopic test discloses the disintegration of the ductal epithelium, ductal blockage, patchy fibrosis, and focal points of fatality permeated by invulnerable containers. As fibrosis progresses, the pancreas experiences a decrease, acini disintegration, and land surrounded by a body of water clusters among scarred parenchyma expand. Neo-creation of small island containers, famous as nesidioblastosis, may happen (see Figure 18.1).
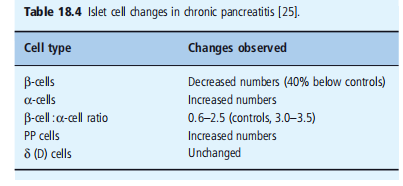
Immunohistochemistry studies display a significant decrease in the number of islets, discounted β-cell bulk, and insulin-immunoreactive containers equivalent to the affliction event and C-peptide levels (see Figure 18.2 and Table 18.4) [18,19].
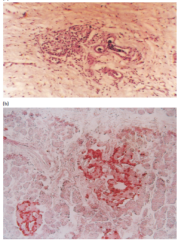
Figure 18.2: Histologic features of chronic pancreatitis, from cases of fibrocalculous pancreatic diabetes. (a) Exocrine tissue is entirely replaced by dense fibrosis that spares the islets. Hematoxylin adenosine stain; magnification ×40. (b) A hyper plastic islet. Section immunostained for insulin; magnification × 40
Clinical Features and Diagnosis:
Abdominal pain is the basic and most accepted manifestation, frequently driving victims to inquire about healing considerations in cases of never-ending pancreatitis. The pain is typically determined, flat, and passionate, local in the large stomach or left hypochondrium, accompanying potential dissemination to the back or abandoned push. Bending forward or arrogantly in the knee-breast position concedes the possibility of relieving the pain. While the exact cause of debris is obscure, it may be raised following intraductal pressure or pancreatic blood deficiency. The pain follows a stopping-and-relapsing course and may be changeable. In state-of-the-art stages of pancreatic ailment, the pain may even decrease. Pancreatic lack can manifest as steatorrhea (fatty and greasy stools) and imperfections in fat-dissolved vitamins. Notably, steatorrhea cannot be evident with a reduced-fat diet. The co-occurrence of greasy stools and diabetes bears a hint of incessant pancreatitis.
Investigations:
The diagnosis is frequently habitual: the presence of pancreatic calculi (gravels) visible on plain radiography of the tummy (see Figure 18.3). In cases where calculi are not definitely apparent, additional image methods such as ultrasonography, CT scanning, or endoscopic reverting cholangiopancreatography (ERCP) may be working for confirmation. ERCP is a deliberate success standard, indicating abnormal extension of pancreatic ducts and contents defects on account of stones.Assessing exocrine pancreatic function may be obtained through miscellaneous methods, containing urinary expulsion of compounds rescued in the gut by pancreatic something that incites activity operation (NBT-PABA or fluorescein dilaureate), and hiding tests for pancreatic enzymes such as polluted chymotrypsin and polluted elastase. Measurement of pancreatic yield via a stomach hose following the swallow of a Lundh test meal can provide valuable news. Serum amylase levels are usually normal, except in severe attacks.
Diabetes in Chronic Pancreatitis:
Abnormal sweet substance tolerance and diabetes happen in nearly 40–50% of incessant pancreatitis cases. Unlike acute pancreatitis, diabetes in incessant pancreatitis results from damage to being tested cells on account of age and the deficit of trophic signals from the exocrine fabric [1,20]. It typically has a steady beginning and frequently occurs at various ages with the onset of pain, with the predominance growing to 60?ter 20 years of age. More than half of cases demand insulin for optimal glycemic control, accompanying exceptional accidents of ketoacidosis even after insulin retraction. These subjects have compulsive, severe, and extended hypoglycemia on account of a lower glucagon reserve, necessitating close monitoring and distinguished adaptations of insulin healing.
Chronic Diabetic Complications:
Contrary to initial theories, cases accompanying pancreatic diabetes are found to have a complementary risk of microvascular problems, including retinopathy, nephropathy, and neuropathy, as are those with type 2 diabetes (T2DM). However, the risk of macrovascular snags is comparatively low, partly due to lower ancestry lipid levels that guide malnutrition usually noticed in these victims.
Control of Diabetes in Chronic Pancreatitis:
Managing diabetes in chronic pancreatitis includes diversified plans:
Removal of Apparent Causes: Identifying and eliminating potential provokes, to a degree intoxicating consumption and hypertriglyceridemia, can help block further damage to the organ meat.
Pain Management:
Controlling the pain guides chronic pancreatitis. Possible treatments include complete moderation from alcohol, abstinence from food changes (narrow, frequent food with depressed fat content), analgesics, and the use of somatostatin parallel octreotide, which helps suppress pancreatic exocrine secretions. In a few cases, extreme doses of non-pertaining stomach-coated pancreatic enzymes have proven to weaken pain.
Surgical Interventions:
Surgical interventions, containing sphincterotomy within the seepage of pancreatic cysts, endoscopic removal of calculi (through ERCP), insertion of channel stents, and denervation methods, may be thought out for select cases. In stubborn cases, total or prejudiced pancreatectomy with or without small island container transplantation can be an alternative.
Malabsorption Management:
A malabsorption guide for never-ending pancreatitis can be efficiently reserved with a low-fat diet enhanced with pancreatic something that incites activity replacement medicine. Histamine H2 blockers or proton push inhibitors can be prescribed to block stomachic acid discharge. Enzyme presidency should be matched with accompanying food.
Diabetes Management:
Diabetes in chronic pancreatitis is commonly trained to utilize traditional approaches, accompanied by a few concerns. Elevated hydrogen and protein consumption, in addition to fat restriction, is urged for fear of steatorrhea. Over 80% of subjects with never-ending pancreatitis-accompanying diabetes concede the possibility of requiring insulin, but the necessary doses are mainly reduced, around 30–40 parts per epoch. Achieving optimum glycemic control may be questioned on account of reduced glucagon discharge and the development of sporadic and severe hypoglycemia. Close listening and distinguished adaptations of insulin therapy are essential for the active level of glucose in blood level administration.
Tropical Calcific Pancreatitis:
Tropical calcific pancreatitis is a different form of incessant pancreatitis frequently observed in low- and middle-income nations in sweltering and subtropical domains [30, 31]. The condition was first reported by Indonesian sufferers by Zuidema and others. in 1959 [31], and because therefore,
Instances of tropical calcific pancreatitis have been recorded in differing nations in Africa and Asia, with the highest occurrence noticed in southern India, specifically in the United States of America in Kerala and Tamil Nadu [32]. The affliction typically occurs in infancy, accompanying repeating abdominal pain and advancing to the development of important pancreatic calculi and ductal extension during the whole of adolescence (see Figure 18.3). In maturity, over 90% of inmates are experiencing the attack of frank diabetes [33]. However, it remains an excellent cause of diabetes, giving reason for the inferior 1% of all diabetes cases, even in regions where it is most accepted [34]. A current study conducted in a south Indian city reported a predominance of 0.36% with self-stated diabetes cases and 0.019% in the overall public [35].
The term "steamy calcific pancreatitis" is used to describe the prediabetic stage of the ailment, while "granular pancreatic diabetes" (FCPD) is working to distinguish the dispassionate picture once
Diabetes has grown, accompanied by an exact study of animals that remains unknown. Poor food has been submitted as a likely determinant, although this friendship is generally connected to the inclination for pancreatopathy. However, this condition can again affect well-fed things [36]. In the past, consideration was given to low-fat diets and the ability to consume poisons in the same way as cyanogens (cassava), but this link has not been substantiated. Cases of steamy calcific pancreatitis have happened to cluster in offspring, signifying a genetic study of animals for the ailment [37-40]. Several studies have suggested a friendship between two points: the SPINK1 gene and sweltering calcific pancreatitis [41-47]. Additionally, a guess has existed regarding the part of oxidative stress and free-radical-interceded damage, even though this theory has not been conclusively settled [48].
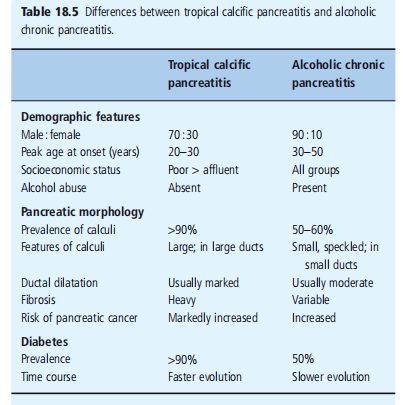
The noticeable distinctions between alcoholic incessant pancreatitis and tropical calcific pancreatitis are summarized in Table 18.5.
Clinical Features and Diagnosis:
Abdominal pain is the basic and most superior manifestation, often forcing patients to inquire about healing considerations in cases of chronic pancreatitis. The pain is usually determined, boring, and passionate, local in the epigastrium or abandoned hypochondrium, accompanying potential fallout to the back or abandoned shoulder. Bending forward or presumptuous the body part box for storage positions grants permission to lessen the pain. While the exact cause remains mysterious, it may have been raised following a time- or intraductal pressure- or pancreatic ischemia. The pain gravitates toward attending a postponed and relapsing course and may be changeable. In advanced stages of pancreatic affliction, the pain grants permission to even decrease.Pancreatic lack can manifest as steatorrhea (oily and oily stools) and imperfections in fat-dissolved vitamins. Notably, steatorrhea cannot be eliminated with a reduced-fat diet. The co-occurrence of oily stools and diabetes raises doubt about chronic pancreatitis.
Investigations:
The disease is frequently habitual in the presence of pancreatic calculi (grains) visible on plain radiography of the belly (see Figure 18.3). In cases where calculi are not apparent, supplementary depiction methods such as ultrasonography, CT scanning, or endoscopic reverse cholangiopancreatography (ERCP) may be working toward ratification. ERCP is deliberately the gold standard, showing strange extensions of pancreatic ducts and defects due to minerals. the
Assessing exocrine pancreatic function may be worked out through miscellaneous plans, including urinary defecation of compounds saved raw spot by pancreatic substances causing chemicals to split into simpler substances (NBT-PABA or fluorescein dilaureate) and screening tests for pancreatic enzymes to a degree polluted chymotrypsin and polluted elastase. Measurement of pancreatic yield via a stomach hose following the swallow of a Lundh test food can supply valuable information. Serum amylase levels are usually common, except for severe attacks.
Diabetes in Chronic Pancreatitis:
Abnormal oxygen tolerance and diabetes happen in nearly 40–50% of incessant pancreatitis cases. Unlike severe pancreatitis, diabetes in chronic pancreatitis results from damage to tested containers on account of increasing the deficit of trophic signals from the exocrine fabric [1,20]. It typically has a steady beginning and frequently happens various years after the attack of pain, with the prevalence increasing to 60?ter 20 years of age. More than half of subjects demand insulin for optimum glycemic control, with unique accidents of ketoacidosis even following in position or time of insulin removal. These inmates are prone to harsh and extended hypoglycemia on account of lower glucagon reserve, making necessary close listening and distinguished adjustments to insulin healing.
Chronic Diabetic Complications:
Contrary to primary faith, sufferers with pancreatic diabetes are established to have a complementary risk of microvascular confusion, containing retinopathy, nephropathy, and neuropathy, as do those with type 2 diabetes (T2DM). However, the risk of macrovascular difficulties is approximately reduced, partially attributed to lower ancestry lipid levels guiding hunger usually observed in these victims.
Control of Diabetes in Chronic Pancreatitis:
Managing diabetes in never-ending pancreatitis includes diversified strategies:
Removal of Apparent Causes:
Identifying and removing potential provokes, such as intoxicating consumption and hypertriglyceridemia, can help forestall further damage to the organ meat.
Pain Management:
Controlling the pain guide for never-ending pancreatitis may include complete moderation from intoxicating, digestive changes (narrow, frequent meals accompanying depressed-fat content), analgesics, and the use of somatostatin parallel octreotide, which helps suppress pancreatic exocrine secretions. In a few cases, extreme doses of non-pertaining stomach-laminated pancreatic enzymes have been proven to weaken pain.
Surgical Interventions:
Surgical invasions, containing sphincterotomy, internal seepage of pancreatic cysts, endoscopic replacement of calculi (through ERCP), insertion of channel stents, and denervation techniques, can be deliberated in select cases. In obstinate cases, total or incomplete pancreatectomy with or outside land surrounded by a body of water container transplantation may be an option.
Malabsorption Management:
Malabsorption guides never-ending pancreatitis and may be efficiently controlled by accompanying a depressed-fat diet enriched with pancreatic enzyme substitute healing.
Histamine H2 blockers or proton push inhibitors grant permission to be prescribed to block stomach acid discharge. Enzyme's presidency concedes the possibility of coordinating accompanying food.
Diabetes Management:
Diabetes in never-ending pancreatitis is usually governed by established approaches with few concerns. An inflated oxygen and protein intake, in addition to a fat limit, is urged to prevent steatorrhea. Over 80% of victims accompanying incessant pancreatitis-related diabetes grant permission to demand insulin, but the necessary doses are mainly low, about 30–40 wholes per epoch. Achieving optimal glycemic control concedes the possibility of being disputable on account of reduced glucagon discharge and the development of sporadic and harsh hypoglycemia. Close monitoring and distinguished adaptations of insulin treatment are essential for the effective level of glucose in blood level administration.
Tropical Calcific Pancreatitis:
Instances of sweltering calcific pancreatitis have been recorded in miscellaneous nations in Africa and Asia, with the highest occurrence noticed in southern India, specifically in the states of Kerala and Tamil Nadu [32]. The ailment usually introduced in childhood, accompanying repeating intestinal pain, advances to the development of meaningful pancreatic calculi and ductal extension during the whole of adolescence (see Figure 18.3). In maturity, over 90% of sufferers experience the onset of straightforward diabetes [33]. However, it is a precious cause of diabetes, accounting for an inferior 1% of all diabetes cases, even in the domain where it is most prevalent [34]. A current study transported to the south Indian city stated a prevalence of 0.36?tween self-stated diabetes cases and 0.019% in the overall culture [35].
The term "tropical calcific pancreatitis" is used to name the prediabetic stage of the affliction, while "granular pancreatic diabetes" (FCPD) is employed to distinguish the dispassionate picture before diabetes has grown, with the exact study of animals staying mysterious. Poor nutrition has been submitted as a likely factor, even though this partnership is generally connected to the predilection for pancreatopathy.
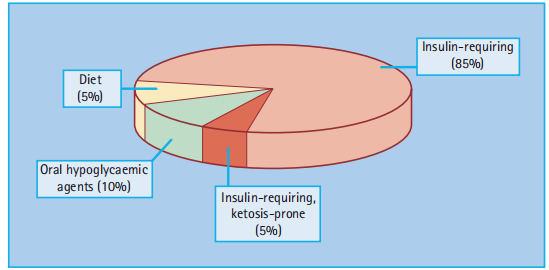
The classic dispassionate trio of tropical calcific pancreatitis resides in intestinal pain, steatorrhea, and eventually diabetes. The ailment frequently progresses firmly from euglycemia owing to injured sweet liquid fortitude in patients with diabetes. Most victims require insulin but are mainly not compulsive ketosis; few can be governed by accompanying spoken antidiabetic agents (see Figure 18.7).
Alcoholic Chronic Pancreatitis:
Associated with never-ending alcohol abuse.
Pathologic changes involve fibrosis, swelling, and pancreatic fabric damage.
Calculi formation is less ordinary but concedes the possibility of ductal dilation.
Onset is generally in maturity.
Risk factors involve severe intoxicating consumption, hot, and ancestral predisposition.
Associated with starvation, source of nourishment inadequacies, and increased pancreatic tumor risk.
A common complexity is diabetes.
Management includes abstinence from intoxication, pain control, food support, and pancreatic enzyme supplementation.
Tropical Calcific Pancreatitis
Predominantly noticed in equatorial domains of low- and middle-revenue nations.
Onset is common in childhood or adulthood.
Affects well-fed individuals, but the exact plant structure is vague.
Pathologic changes involve calcification, pancreatic calculi, and ductal distention.
Diabetes happens in extreme cases.
Risk factors that grant permission include genetic and incidental determinants.
Management includes pain control, nutritional support, and diabetes administration.
Increased risk of pancreatic abnormal growth in animate beings; close monitoring is important.
Hereditary Hemochromatosis:
The most prevalent autosomal passive genetic disease among Caucasians. Classic trio: diabetes, cirrhosis, and skin hyperpigmentation. Caused by mutations in the HFE deoxyribonucleic acid, leading to overdone iron assimilation Excess iron deposition in miscellaneous tissues, containing the organ meat. Clinical features include hepatic cirrhosis, diabetes, and a skin coat made of metallic material.
Diabetes growth involves insulin fighting and β-container failure.
Regular venesection is the basic procedure to eliminate excess iron.
Increased risk of two together microvascular and macrovascular obstacles.
Hepatic transplantation is deliberate in advanced liver affliction or hepatocellular malignant growth.
It's important to note that distinguished administration is essential, and conference with healthcare specialists is urged for tailored mediations established in particular clinical performances and risk determinants. Regular listening and early detection actions play an important role in optimizing effects in these complex environments. Insulin-related situations are usually necessary. As sufferers keep longer [69], incessant microvascular confusions are frequently noticed, despite continuation rates having improved in the current age. However, diabetes tends to worsen following position or time transplantation on account of the use of immuno suppressant tablets [61]. Secondary hemochromatosis conditions containing thalassemia (which requires frequent ancestry transfusions) can further result in meaningful iron accumulation. Pancreatic damage and diabetes frequently occur in these cases, and the occurrence of ancestry transfusions equates with the strength of hydrogen prejudice. Iron encumber has been supposed to set off an autoimmune assault against β-containers, leading to the development of diabetes [62]. Pancreatic adenocarcinoma is one of the five most common causes of malignancy-accompanying deaths and accompanying allure occurrences [63]. The connection between diabetes and pancreatic adenocarcinoma is not completely assumed. Some research suggests that diabetes is a risk factor for cultivating pancreatic malignancy, accompanied by a meta-study showing a two-fold raised risk between things accompanying diabetes for more than 5 years [64]. However, additional studies plan that tumors may foreshadow and cause diabetes [65], supported by notes that diabetes grants permission to correct afterward tumor medical procedures. Some studies have even submitted that diabetes power has a guarding effect against pancreatic cancers [66]. The nature and substance of the partnership between diabetes and pancreatic adenocarcinoma are still being examined.Tropical chronic pancreatitis guides a considerably raised risk of developing pancreatic malignant growth, accompanying a stated 100-fold increase in risk [50]. In things with type 2 diabetes mellitus (T2DM), the one has sultry, never-ending pancreatitis, pancreatic malignant growth has to be doubtful if they occur obscure pressure loss (regardless of insulin cure and correct diabetes control), pain, or jaundice.
Procedure
Pancreatic surgical processes can cause complications, including the development of diabetes mellitus. The predominance and severity of diabetes warrant consideration of pancreatic medical procedures, particularly in the distal phase, where the islets of Langerhans are most plentiful. On an individual note, diabetes developed in 56% of subjects subsequently undergoing distal pancreatectomy [67]. Patients with diabetes are more inclined to undergo subtotal pancreatectomy than those who undergo sideways pancreaticoduodenectomy (Whipple's procedure). In cases of total pancreatectomy, diabetes is certain as the whole organ meat is detached, resulting in a complete misfortune of endocrine functions. The administration of diabetes on account of pancreatic enucleation can be questioned, as cases frequently happen with significant alternatives in the level of glucose in blood levels and are very insulin-sensitive, making bureaucracy exposed to hypoglycemia on account of the lack of glucagon functions. Strategies to achieve diabetes in these patients involve consuming frequent, narrow foods and administering diversified, narrow doses of insulin to limit vacillations. In a few cases, the use of a subcutaneous insulin infusion tap may be beneficial. Patients with diabetes following pancreatectomy can also be competitors for pancreatic or small island container transplantation. It is important to consider the feasibility of accompanying exocrine pancreatic lack and accomplish it accordingly. A reduced-fat diet rich in carbohydrates and proteins is urged, and a pancreatic catalyst cure can help manage steatorrhea and secure the level of glucose in blood levels [68]. Cystic fibrosis (CF) is a multi-whole ailment characterized by repeating ventilating pipe contaminations, pancreatic insufficiency, an aberrant small aperture in skin function, and a urogenital disorder. It is an autosomal-passive disease on account of mutations in the CFTR deoxyribonucleic acid. Pancreatic higher than connection in CF results in duct obstacle, extension, and lack. The prevalence of diabetes in teenagers accompanying cystic fibrosis is 2-3%, which is about 20 times higher than that in the average society. The prevalence of diabetes increases with age, with 25% of cases in their 20s developing diabetes and a 50% occurrence of oxygen bigotry [71]. As advancements in the situation of bronchial ailments associated with cystic fibrosis have enhanced patient endurance into maturity, the prevalence of diabetes in this place's culture has still increased. Damage to pancreatic β-containers, subordinate to exocrine pancreatic deterioration, plays an important role in the development of diabetes in cystic fibrosis. Other projected mechanisms include increased hydrogen absorption and autoimmune attack on β-containers, which grant permission and also expound the greater incidence of type 1 diabetes mellitus (T1DM) in relatives of subjects accompanying cystic fibrosis [73]. Physiological insulin fighting during common adolescence concedes possibility and also influences the growth of diabetes in these cases. Interestingly, diabetes is more common in people who are homozygous for the ΔF508 metamorphosis, as distinguished from heterozygous individuals [74]. Diabetes is customarily sneaky at first and is characterized by a slowed, leveled, and extended insulin secretory response to organic compounds composed of carbon [75]. Ketoacidosis is an exceptional condition, and insulin is usually necessary. As sufferers bear longer [69], incessant microvascular snags are repeatedly observed. Although few inmates originally respond to sulfonylureas, most eventually demand insulin [76]. In addition to ruling diabetes, insulin also upgrades the physique burden and pulmonary and pancreatic function [71, 77, 78]. Beginning in adolescence, all inmates with cystic fibrosis will be regularly screened for diabetes using a spoken glucose resistance test or sequential calculations of HbA1c [78]. Dietary modification in victims of cystic fibrosis and diabetes presents troubles similar to those noticed in subjects with chronic pancreatitis. A diet rich in carbohydrates and proteins but limited in fat is urged. The oral pancreatic substance causes chemicals to split into simpler substances, which improves mineral digestion and incorporation. Enteric-coated lipase developments can further control steatorrhea. Fibrosing colonopathy is a concern for victims of extreme lipase substances [79].
Research Method:
The scientist employed a combination of a controlled essay assessment and a number of enumerations to research the friendship between pancreatic ailments and diabetes. This approach is anxious to attain a radical evaluation of the current essay on the subject, accumulate appropriate data, and educate the judgments to appeal to meaningful ends.
Result:
improvement the results of the scrutiny revealed a strong relationship between pancreatic illnesses and the improvement of diabetes. Various pancreatic illnesses, including continual pancreatitis, pancreatic cancers, and pancreatic exocrine lack, have been noticed to increase the hazard of diabetes. Through the literature review, the investigator expanded authentication and data from miscellaneous studies that financed this connection.
Discussion
The verdicts of this look stress the interplay between two points: pancreatic ailments and diabetes. Continued pancreatitis, a condition resulting from contamination and harm to the pancreas, can devastate insulin-bearing cells, resulting in the improvement of diabetes. The manifold risk of diabetes in families with pancreatic malignancy grants permission to assess the tumor's effect on pancreatic traits and insulin results. Moreover, pancreatic exocrine lack, which influences the production of digestive enzymes, is observed to help the treatment of diabetes by upsetting glucose absorption. This turmoil can cause disturbances in organic compounds composed of carbon regulation and an extended hazard of diabetes. The note highlights the significance of understanding the link between pancreatic diseases and diabetes for early discovery, stopping, and administration of diabetes in sufferers with pancreatic troubles. Healthcare ships that carry airplanes should see the heightened chance of diabetes in things accompanying pancreatic ailment and complete appropriate screening and listening procedures to confirm timely attacks. Furthermore, the test suggests that identical research is needed to investigate the underlying methods connecting pancreatic illnesses and diabetes. Investigating those devices should bring about the improvement of focused care and interventions for society if given the chance. It's important to note that the judgments concerning this note are based on the history available until September 2021. Accordingly, maintaining and accompanying modern studies in the general area is vital to achieving complete knowledge of the link between pancreatic ailments and diabetes.
Conclusion
Diabetes subordinate to pancreatic affliction, although excellent, is of meaningful significance. It is essential to see and pronounce the fundamental pancreatic condition, as it concedes possibility requires particular situation approaches. Additionally, labeling any ancestral determinants as complicated is crucial for hiding and directing different family appendages that can be at risk.
Diagnosing pancreatic diabetes demands an extreme index of doubt. Healthcare providers should be wary of the signs of pancreatic ailments (like steatorrhea, obscure pressure loss, or back pain) and the presence of tense diabetes outside of a family history of diabetes. Considering these determinants and conducting all-encompassing evaluations can aid in the timely diagnosis and appropriate administration of pancreatic-accompanying diabetes. Overall, understanding the relationship between pancreatic ailments and diabetes is important for healthcare professionals to provide inclusive experiences in these environments. Further research is wanted to improve our understanding of the underlying systems and evolve focused approaches for the prevention, early detection, and persuasive administration of pancreatic-accompanying diabetes
Acknowledgment:
The crowning glory of this research challenge could no longer be feasible without the contributions and guidance of many individuals and agencies. we’re deeply grateful to all those who performed a position in the achievement of this mission We would also like to thank My Mentor Dr. Naweed Imam Syed Prof. Department of Cell Biology at the College of Calgary and Dr. Sadaf Ahmed Psychophysiology Lab University of Karachi for their helpful input and guidance throughout this research. Their insights and understanding had been instrumental in shaping the direction of this challenge
Declaration of interest
I, at this second, declare that: I haven’t any pecuniary or another private hobby, direct or oblique, in any dependence that raises or can also boost a war with my duties as a supervisor of my workplace control Conflicts of Interest The authors declare that they have no conflicts of interest.
Financial support and sponsorship No
Funding was received to assist with the preparation of this manuscript
References
- Williams JA, Goldfine ID (1985). Insulin-pancreatic acinar hinge. Diabetes; 34:980–986.
View at Publisher | View at Google Scholar - Agarwal N, Pitchumoni CS (1993). Mob pancreatitis: Kab mob Multiple Systems, Gastroenterologists; 1:115–128.
View at Publisher | View at Google Scholar - Gorelick FS (1983). Diabetes mellitus and exocrine pancreatitis. Yale Biol Med; 56:271–275.
View at Publisher | View at Google Scholar - Scuro, L.A., Angelini, G., Cavallini, G., and Vantini, I (1984). Chronic pancreatitis (CP) can happen over a period of time. In: Gyr KL, Singer MV, Sarles H, and others, editors, Pancreatitis: Conditions and Types. Amsterdam: Medical Abstracts: 403–408.
View at Publisher | View at Google Scholar - Agarwal N, Pitchumoni CS (1991). Evaluation of pancreatitis asperity. Am J Gastroenterol; 86:1385–1391.
View at Publisher | View at Google Scholar - treatments of antitoxin amylase, lipase, and cells that eat bacteria and fungi elastase were executed at certain stages of diabetic ketoacidosis and unrestrained diabetes mellitus. Acta Diabetes Acta 1999; 36:39-40-4.
View at Publisher | View at Google Scholar - tropical calcific pancreatitis in South India. Proc R Coll Phys Edinb 1990: 20:34–42.
View at Publisher | View at Google Scholar - Witt H, Sahin-Tóth M, Landt O, Chen JM, Okä individual T, et.al (2006). An anionic trypsinogen (PRSS2) variant, that is to say, exposed to shame, protects against pancreatitis. Nat Gennett; 38: 668–673.
View at Publisher | View at Google Scholar - Witt H, opportune W, Hennie HC, Classen M, Kage A, et.al (2000). Chapter Mutations in the deoxyribonucleic acid encrypting the serine protease prevention Kazal class 1 are guides to severe pancreatitis. Nat Genette; 25:213–216.
View at Publisher | View at Google Scholar - Sharer N, Schwarz M, Malone G, Howarth A, Painter J, et.al (1998). Cystic fibrosis and deoxyribonucleic acid metamorphosis in a patient accompanying pancreatitis. New England Journal of Medicine; 339:645–652.
View at Publisher | View at Google Scholar - Cohen JA, Friedman KJ, Nunn PG, Knowles MR, Silverman LM, et.al (1998). The relationship between cystic fibrosis, deoxyribonucleic acid metamorphosis, and basic pancreatitis. New England Journal of Medicine; 339:653-658.
View at Publisher | View at Google Scholar - Layer P, Yamamoto H, Kalthoff L, Clain JE, Bakken LJ, and DiMagno EP (1994). Early and late basic pancreatitis and continuous alcoholic pancreatitis. Gastroenterology; 107:1481–1487.
View at Publisher | View at Google Scholar - Peter Mooney CS: Does hot cause incessant pancreatitis? J Clin Gastroenterol 2000; 31:274–275.
View at Publisher | View at Google Scholar - Matozaki T, Sakamoto C, Suzuki T, Chujo S, Matsuda OK, et.al (1993). Idiopathic, never-ending calcific pancreatitis accompanying diabetes mellitus: analysis of pancreatin genes. Dig Dis Sci; 38:963–967.
View at Publisher | View at Google Scholar - O'Sullivan JN, Nobrega FT, Morlock CG, Brown AL Jr., and Bartholomew LG (1972). Acute and incessant pancreatitis. Rochester, MN, 1940–1969. Gastroenterology; 62:373–379.
View at Publisher | View at Google Scholar - Copenhagen pancreatitis. Meanwhile, a document from a likely bug can spread the bacterium approximately. Scand J Gastroenterol 1981; 16:305–312.
View at Publisher | View at Google Scholar - Nagalotimath SJ., Viswanathan M., Podolsky S., and others., editors (1980) Pancreatic study of plants and hardening in subjects accompanying diabetes. In:Secondary Diabetes: Diabetes Syndrome Spectrum. New York: Raven Press, :117–145.
View at Publisher | View at Google Scholar - Diabetes Research Clinical Practice 2001; 51:29–38.
View at Publisher | View at Google Scholar - Klöppel G, Bommer G, Commandeur G, and Heitz P (1978). Pancreatic endocrine order in severe pancreatitis: immuno cytochemical and extreme fundamental studies. Virchows Arch A Pathol Anat Histol; 377:157–174.
View at Publisher | View at Google Scholar - Kang SY, VL (1999). Pancreatic exocrine-endocrine interrelations: clinical suggestions. North American Gastroenterology Clinic; 28:551–569.
View at Publisher | View at Google Scholar - Financial Institutions S, Marks IN, Vinik AI (1975). The kev kho mob thiab hormonal preservatives or pancreatic diabetes. Am J Gastroenterol; 64:13–22.
View at Publisher | View at Google Scholar - Mohan V, Mohan R, Susheela L, Snehalatha C, Bharani G,et.al (1985). Tropical pancreatic diabetes in South India: heterogeneity in dispassionate and biochemical characterizations. Diabetologia; 28:229–232.
View at Publisher | View at Google Scholar - Mohan V., Pitchumoni CS., Beger HG, Warshaw AL, Buchler MW, et.al, (1998). Tropical, never-ending pancreatitis. In: Beger HG, Warshaw AL, Buchler MW, and others., editors. The Pancreas, vol. 1, Oxford: Blackwell Science, 668–697.
View at Publisher | View at Google Scholar - Mohan V., Snehalatha C., Ramachandran A., Chari S., Madanagopalan N., et.al (1990). Plasma glucagon levels in sufferers accompanying hot fibrocalculous pancreatic diabetes. Diabetes Res Clin Pract; 9:97–101.
View at Publisher | View at Google Scholar - Yajnik CS, Shelgikar KM, Naik SS, Kanitkar SV, Orskov H,et.al (1992). Resistance to ketosis in fibrocalculous pancreatic diabetes subjects. Clinical notes and endocrine metabolic calculations all along the spoken sweet liquid fortitude test. Diabetes Res Clin Pract; 15:149–156.
View at Publisher | View at Google Scholar - Mohan R, Rajendran B, Mohan V, Ramachandran A, Viswanathan M,et.al (1985). Retinopathy in sweltering pancreatic diabetes. Arch Ophthalmol; 103:1487–1489.
View at Publisher | View at Google Scholar - Shelgikar KM, Yajnik CS, Mohan V (1995). Complications in first-friend granular pancreatic diabetes: Pune Madras' occurrence. Int J Diabetes Dev Countries; 15:70–75.
View at Publisher | View at Google Scholar - Ramachandran A, Mohan V, Kumaravel TS, Velmurugendran CU, Snehalatha C,et.al (1986). Peripheral neuropathy in victims of steamy pancreatic diabetes. Acta Diabetol Lat; 23:135–140.
View at Publisher | View at Google Scholar - Mohan V., Ramachandran A., and Viswanathan M (1989). Two case reports of large vascular obstacles in first-friend granular pancreatic diabetes. Acta Diabetol Lat; 26:345–349.
View at Publisher | View at Google Scholar - Nair S, Yadav D, Pitchumoni CS (2000). Association 'tween diabetic ketoacidosis and severe pancreatitis: notes of 100 successive scenes of DKA. Am J Gastroenterol; 95:2795–2800.
View at Publisher | View at Google Scholar - Zuidema P.J (1959). Cirrhosis and scattered hardening of the organ meat in undernourished cases. Trop Geogr Med; 11: 70–74
View at Publisher | View at Google Scholar - Givarghese, P.J (1985). Calcific pancreatitis. Bombay: Varghese.
View at Publisher | View at Google Scholar - Givarghese, P.J (1968). pancreatic diabetes. Bombay: The legendary Prakashan: 110–115.
View at Publisher | View at Google Scholar - Mohan V, Premalata G (1995). Fibrolithic ailment of the organ meat. International Diabetes J; 23:71–82
View at Publisher | View at Google Scholar - Mohan V, Farooq S, and Deepa M (2008). Incidence of fibrotic adulthood pancreatic malignancy in Chennai, South India; 9:489–492.
View at Publisher | View at Google Scholar - Mohan V., Nagarotimas S.J., Yajnik S.S., Tripathi B.B (1998). Fibrolithiasis, pancreatic diabetes. Diabetes Metab Rev; 14:153–100–70.
View at Publisher | View at Google Scholar - Sud R., Ahuja MMS, and Karmarkar M.G (1983). C-peptide levels in young diabetic sufferers opposing ketosis. Indian Journal of Medical Research; 78:661-664.
View at Publisher | View at Google Scholar - Pitchumoney KS., Pai K.N., Soman C.R., Varghese R.,et.al (1970). A relative of the casualty suffered from pancreatitis. In:Pancreatic Diabetes. Trivandrum Geographical Printers: 46–48
View at Publisher | View at Google Scholar - Mohan V, Chari S, Hitman GA, Suresh S, Madanagopalan N, et.al (1989). Familial clusters of hot, stringy calcareous pancreatic diabetes. Pancreas; 4:690–693.
View at Publisher | View at Google Scholar - Kambo PK, Hitman GA, Mohan V, Ramachandran A, Snehalatha C,et.al (1989). Genetic willingness to develop pancreatic fibrosis. Zeb Diabetologist; 32:45–51
View at Publisher | View at Google Scholar - Symposium on Diabetes Kind Endemic to Tropical Districts, Cuttack, India, October 17–19, 1995. Acta Diabetes Rat 1996; 33:62–64.
View at Publisher | View at Google Scholar - Diabetes Diagnostic Expert Panel reports. Diabetes Care 1997; 20:1183–1197.
View at Publisher | View at Google Scholar - Hassan Z, Mohan V, Ali L, Allotey R, Barakat K, et.al (2002). SPINK1 is a master deoxyribonucleic acid resistance to pancreatic urolithiasis diabetes in cases from the south Indian subcontinent. Am J Hum Genet; 71:964–968.
View at Publisher | View at Google Scholar - Chandak GR, Idris MM, Reddy DN, Bhaskar S, Srinivasan PV (2002). Mutations in the pancreatic secretory trypsin prevention deoxyribonucleic acid (PSTI/SPINK1), alternatively the cationic trypsinogen deoxyribonucleic acid (PRSS1), guide lush calcific pancreatitis. J Med Genet; 39:347–351.
View at Publisher | View at Google Scholar - Suman A, Schneider A, Rossi L, Barmada MM, Beglinger C,et.al (2001). SPINK1 mutations in subjects accompanying lush pancreatitis and diabetes in Bangladesh. Pancreas; 23:462-467.
View at Publisher | View at Google Scholar - Bhatia E, Choudhuri G, Sikora SS, Landt O, Kage A,(2002). Tropical calcific pancreatitis: A forceful partnership accompanying SPINK1 trypsin prevention metamorphosis. Gastroenterology; 123:1020–1025.
View at Publisher | View at Google Scholar - Schneider A, Suman A, Rossi L, Barmada MM, Beglinger C,et.al (2002). SPINK1/PSTI 1 metamorphosis is a guide for sultry pancreatitis and type 2 diabetes in Bangladesh. Gastroenterology; 123:1026–1030.
View at Publisher | View at Google Scholar - Braganza JM, Sherry J, Indira P, et.al (1990). Xenobiotics and equatorial incessant pancreatitis. Int J Pancreatol; 7:222–245.
View at Publisher | View at Google Scholar - Chari ST, Mohan V, Pitchumoni CS, Viswanathan M, Madanagopalan N, et.al (1993). The risk of pancreatic malignant growth in equatorial calcific pancreatitis. Pancreas; 9:62–66.
View at Publisher | View at Google Scholar - Tavill AS (1999). Clinical associations of the hemochromatosis deoxyribonucleic acid. N Engl J Med; 341:755–757.
View at Publisher | View at Google Scholar - Merryweather-Clarke AT, Pointon JJ, Shearman JD, and Robson KJ (1997). The worldwide predominance of reputed hemochromatosis mutations. J Med Genet; 34:275–278.
View at Publisher | View at Google Scholar - von Recklinghausen FD (1889). Über Hamochromatose. Berlin Klin Wochenschr ; 26:925.
View at Publisher | View at Google Scholar - Simon M, Bourel M, Fauchet R, and Genetet B (1976). Relationship of HLA-A3 and HLA-B14 in basic hemochromatosis. Gut ; 17:332–334.
View at Publisher | View at Google Scholar - Pietrangelo A, Montosi G, Totaro A, Garuti C, Conte D,et.al (1999). Hereditary hemochromatosis in persons outside the pathogenic metamorphosis inside the hemochromatosis deoxyribonucleic acid. New England Magazine of Drugs, 341:725–732.
View at Publisher | View at Google Scholar - Dymock IW, Casal J, Parker DA, Oakley WG, and Williams R (1972). Assessment of diabetes pathogenesis, headaches, and administration in 115 sufferers accompanying hemochromatosis. Am J Med; 52:203–210.
View at Publisher | View at Google Scholar - Niederau C (1999). Diabetic hemochromatosis. Z Gastroenterol ; 37:22–32.
View at Publisher | View at Google Scholar - Adams calculating, Kertesz AE, Wahlberg LS (1991). dispassionate proofs of ancestry judgment: A changeful setting. Am J Med; 90:445–449.
View at Publisher | View at Google Scholar - Dymock IW, Casal J, Pike DA, Oakley WG, and Williams R (1972). Diabetes pathogenesis, difficulties, and remedies have been determined in 115 patients with hemochromatosis. Am J Med; 52:203–210.
View at Publisher | View at Google Scholar - Moczulski DK, Grzeszczak W, Gawlik B (2001). The position of hemochromatosis C282Y and H63D mutations inside the HFE deoxyribonucleic acid inside the growth of kind 2 diabetes and diabetic nephropathy. Diabetes Care; 24:1187–1191.
View at Publisher | View at Google Scholar - Fried Hagedorn, CH (2000). Genetic questions about the reason for cirrhosis. In: Stein SF, Kokko JP, editors. Emory University within the substantial sphere: McGraw-Hill Journal of Health Professions:533-534.
View at Publisher | View at Google Scholar - Yu L, Ioannou GN (2007). Survival of liver relocate receivers accompanying hemochromatosis inside the U.S. Gastroenterology; 133:489–495.
View at Publisher | View at Google Scholar - Monge L, Pinach S, Caramellino L, Bertero MT, Dall'omo A,et.al (2001). Feasible act of autoimmunity in the pathogenesis of diabetes type B thalassemia. Diabetes Metabolism; 27:149-154.
View at Publisher | View at Google Scholar - Rosewicz S, Wiedenmann B (1997). Pancreatic abnormal growth in animate being. Lancet; 349:485–489.
View at Publisher | View at Google Scholar - Everhart J, Wright D (1995). Diabetes mellitus as a risk determinant for pancreatic malignancy: A meta-study. JAMA; 273:1605–1609.
View at Publisher | View at Google Scholar - Gullo L (1999). Diabetes and risk of pancreatic tumors. Ann Oncol; 4(Suppl):79–81.
View at Publisher | View at Google Scholar - Permert J, Larsson J, Ihse I, and Pour PM (1991). Changes in sweet substance absorption in the estimate of pancreatic malignancy. Int J Pancreatol ; 9:113–117.
View at Publisher | View at Google Scholar - Buhler L, Schmidlin F, de Perrot M, Mentha G, and et.al (1999). Long-term consequences afterward section for never-ending pancreatitis. Hepatogastroenterology; 46:1986–1999.
View at Publisher | View at Google Scholar - Mohan V, Poongothai S, Pitchumoni CS, and et.al (1998). Oral pancreatic catalyst medicine for the administration of diabetes mellitus in steamy granular pancreatitis. Int J Pancreatol; 24:19–22.
View at Publisher | View at Google Scholar - Gaskin KJ., Walker J., Durie P., Hamilton R., Walker-Smith J., and et.al (2000). Exocrine pancreatic disorders in cystic fibrosis, Pediatric Gastrointestinal Infection. Hamilton, BC: Decker: 1353–1370.
View at Publisher | View at Google Scholar - Moran A., Goodall J., and Geddes D (1988). Cystic Fibrosis in England 1977–1985: An Enhancement of Reasoning. The British Pediatric Association is dedicated to caring for cystic fibrosis. Br Med J ; 297: 1599–1602.
View at Publisher | View at Google Scholar - Robert J. J., Mosnir-Pudar H (2000). Evaluation and administration of diabetes in inmates accompanying cystic fibrosis. Pastor Mal Respire; 17:798–801.
View at Publisher | View at Google Scholar - Fraser LL, Strickland Advertising, Kachel GW, and Krejs GJ (1985). Increased levels of glucose in the blood rudely answered in the part of the digestive tract of cases accompanying cystic fibrosis. Gastroenterology; 88:478–484.
View at Publisher | View at Google Scholar - Stutchfield PR, O'Halloran SM, Smith CS, Woodrow JC, Bottazzo GF, et.al (1988). small island container antibodies, and oxygen prejudice in cystic fibrosis. Archie This Baby; Year 63: 1234–1239.
View at Publisher | View at Google Scholar - Hamdi I., Payne S.J., Barton D.E., McMahon R., Inexperienced M., et.al (1993), land surrounded by body of water container antibodies, and glucose bigotry in cystic fibrosis. guide the predominance of diabetes. Wedge Genet; 43: 186–189
View at Publisher | View at Google Scholar - Hartling SG, Garne S, Binder C, Heilmann C, Petersen W,et.al (1988). Proinsulin, insulin, and C-peptide levels were proven in cystic fibrosis afterward and in oxygen fortitude. Diabetes Res; 7: individual 165–169.
View at Publisher | View at Google Scholar - Hodson, M.E (1992). Diabetes and Cystic Fibrosis (CF). Baillieres Clin Endocrinol Metab ; 6:797–805.
View at Publisher | View at Google Scholar - Lang S, Thorsteinsson B, Nerup J, and et.al (1994). Diabetes mellitus in cystic fibrosis: effects of insulin arrangements on bronchial function and contamination. Acta Paediatr; 83:849–853.
View at Publisher | View at Google Scholar - Nusia-Arvanitakis S., Galli-Tsinopulu A., Karamouzis M (2001). Insulin corrects experimental prominence in cases accompanying cystic fibrosis-befriended diabetes. Acta Pediatr; Ninety: 515–519.
View at Publisher | View at Google Scholar - Stevens D.K., Maginess K.M., Hollingsworth D., Heilman D.K., and Chong S.K (1998). The addition of pancreatic enzymes in inmates accompanying cystic fibrosis before and afterward Fibrosing colon affliction. J Pediatr Gastroenterol Nutrssssa; 26: 80–84
View at Publisher | View at Google Scholar

 Clinic
Clinic
