Mini Review | DOI: https://doi.org/10.31579/2834-8761/015
Cardiac Tamponade the Debut of Systemic Lupus Erythematosus in a Young Man: Case Report
- Jessica Paola Jimenez Wilches *
- Mario A. Lora Andocilla
- Amilkar Jose Almanza Hurtado
- Miguel Aguilar Schotborgh
- Carmelo Duenas Castell
1 Internal Medicine, Metropolitan University.
2 Critical medicine and intensive care, health management clinic, Cartagena.
3 Fellows critical medicine and intensive care University of Cartagena.
4 Critical medicine and intensive care, University of Cartagena.
5 Research group in intensive care and obstetrics (GRICIO)
*Corresponding Author: Jessica Paola Jiménez-Wilches, Internal Medicine, Metropolitan University.
Citation: Jimenez Wilches JP, Mario A. Lora Andocilla, Almanza Hurtado AJ, Miguel A. Schotborgh, Carmelo D. Castell (2023), Cardiac Tamponade the Debut of Systemic Lupus Erythematosus in a Young Man: Case Report, Clinical Endocrinology and Metabolism, 2(2) DOI:10.31579/2834-8761/015
Copyright: © 2023, Jessica Paola Jiménez-Wilches. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 22 March 2023 | Accepted: 06 April 2023 | Published: 11 April 2023
Keywords: rabeprazole; proton pump inhibitor; unique
Abstract
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease that can affect any organ. The classic manifestations generally consist of arthralgia, myalgia, arthritis, photosensitivity, and renal failure. Almost half of the patients present cardiac alterations throughout the disease and cardiac tamponade is described as one of the late complications, becoming an infrequent form of initial presentation. We present the case of a 32-year-old man who consulted for precordial pain, dyspnea, and lower limb edema. Acute coronary syndrome is suspected, on admission an ultrasonographic examination was performed with evidence of cardiac tamponade that led to emergent interventions that saved the patient's life. The paraclinical tests ruled out infectious causes and a high titer of ANAS, anti-DNA associated with clinical variables led to the diagnosis of SLE. Immunomodulatory management was started and he was discharged on the 16th day of stay.
Introduction
A 32-year-old male patient, who consulted due to a clinical picture of 7 days of evolution consisting of progressive dyspnea until presenting dyspnea at rest associated with oppressive precordial pain of moderate intensity without irradiation, which is why he was admitted to the emergency department where they considered coronary syndrome. acute reason for which they refer to the intensive care unit.
As an important personal history, he manifested a recent diagnosis of arterial hypertension and deterioration of left ventricular function controlled with losartan, carvedilol and furosemide. She denies diabetes, asthma, dyslipidemia, fever, or trauma.
On admission, they found a hypertensive patient (171/105 mmHg) and tachypneic (24 rpm), with jugular engorgement and bibasal crepitus. Additionally, the dema that leaves pitting 2+ in the lower limbs and capillary refill of 4 seconds stands out. An ultrasound is performed at the patient's bedside, documenting signs of pulmonary congestion, bilateral pleural effusion predominantly on the left, ascites, and severe pericardial effusion that collapses the right cavities. Therefore, a patient with signs of cardiac tamponade is considered. (Image 1 – 2). It is valued by the general surgery service who perform pericardiocentesis under ultrasound guidance with little return of hemorrhagic fluid. During the procedure, the patient became unstable due to altered consciousness, arterial hypotension (TAM 56 mmHg) and desaturation (SpO2: 85%), for which an airway was secured and a pericardial window was performed emergently with 2000 drainage. ml of bloody fluid. A sample of pericardial fluid is taken and studies are requested to determine etiology.
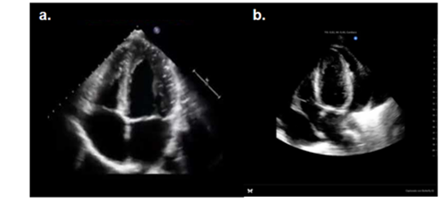
Image 1: Apical 4-chamber view. to. Normal heart chambers. b. Severe pericardial effusion with right atrial collapse in diastole.

Image 2: Subxiphoid 4-chamber view, severe pericardial effusion with right ventricular collapse in diastole.
Paraclinical tests on admission (Table 1) show normocytic anemia, indirect hyperbilirubinemia, elevated acute phase reactants, azotemia, metabolic acidosis, and hyperkalemia with negative serology and urinalysis with red blood cell casts. Patient becomes anuric so hemodialysis is started. Twenty-four hours later, successful intubation is achieved. Pericardial fluid cytochemical was received with inflammatory characteristics, without bacteria in the Gram, ADA and negative cultures. In addition to paraclinical tests in blood with ANAS (positive), ANTI-DNA: reactive, ANTI-SM (positive), ANTI-RO (positive), ANTI-LA (positive), consumption of C3 complement, lupus anticoagulant > 20% of the control, AC ANTI-CITRULLINE (positive).
Biopsy of tissue pericardium with non-specific moderate chronic inflammation, negative for granulomas, specific microorganisms and for malignancy. For all of the above, we consider the diagnosis of SLE with diagnostic criteria according to The American College of Rheumathology (ACR): 5/11 (arthritis, polyserositis, renal failure, immunological disorder, positive antinuclear antibodies), SLICC (2012) :8/17 positive criteria, including 1 Clinical Criteria AND 1 Immunological Criteria and SLE EULAR/ACR 2019 > 10 points.
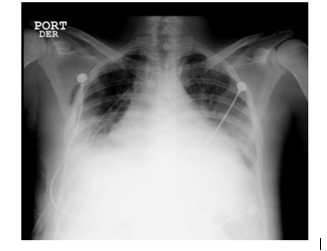
Image 3: Post-pericardial window control chest X-ray. Expired projection. Increased cardiac silhouette suggestive of cardiomegaly and/or pericardial effusion. Alveolar opacities in lung bases due to atelectasis and/or pleural effusion. Right chest tube.
Steroid pulses (methylprednisolone) are started with adequate response and initiation of disease-modifying drugs. Sixteen days later, the patient is discharged from the unit with control echocardiogram showing LVEF of 55% and no evidence of pericardial effusion. Outpatient follow-up was ordered by nephrology, rheumatology and internal medicine.
Table 1. Admission paraclinical report. | |
Laboratory | Result |
Leukocytes (mm3) | 4800 |
Neutrophils (%) | 65 |
Lymphocytes (%) | 30.9 |
Hemoglobin (g/dl) | 8.3 |
Hematocrit (%) | 25.1 |
Platelets (mm3) | 150,000 |
C Reactive Protein (mg/dl) | 48 |
Erythrocyte Sedimentation Rate (mm/hour) | 60 |
Thromboplastin Time (sec) (11Sec) | 14.3 |
INR | 1.18 |
Partial thromboplastin time (sec) (29 sec) | Four. Five |
Total bilirubins (mg/dl) | 4.27 |
Indirect Bilirubin (mg/dl) | 3.37 |
Albumin (g/dl) | 3.6 |
Lactate dehydrogenase (U/L) | 937 |
Ureic Nitrogen (mg/dl) | 71.7 |
Creatinine (mg/dl) | 4.41 |
Sodium (mEq/L) | 144.3 |
Potassium (mEq/L) | 5.83 |
Chlorine (mEq/L) | 111.6 |
ultrasensitive troponin I | 0.3 |
Natriuretic Peptide ( pg /ml) | 210 |
Immunological profile | |
Lupus anticoagulant (sec)* | 51 |
Extractable Antinuclear Antibodies (Sm, Sss , Rnp ) | 162.47 (Positive) |
IFI antinuclear antibodies | 1/2560 (Reagents) |
IFI Anticytoplasmic Antibodies | 1/20 (Reagents) |
Anti-citrulline IgG antibodies | 21.6 (Positive) |
anti- dsDNA | 1/320 (Reactive) |
Total ENAS (UI) | 155.26 (Positive) |
Anti SM (EU/ml) | 161.12 (Positive) |
Anti Ro (EU/ml) | 24.81 (Positive) |
Anti La (EU/ml) | 21.75 (Positive) |
Complement C3*** | 56.66 |
Complement C4**** | 13.34 |
Beta 2 Glycoprotein I – Anticardiolipin- Phosphatydyl serine, Phosphatidyl inositol – Phosphatidic Acid | Normal |
Coombs Indirect | Negative |
infectious profile | |
HIV 1 and 2 | Negative |
Hepatitis B surface antigen | not reactive |
Anti-Hepatitis C | not reactive |
VDRL | not reactive |
tuberculin test | Negative |
Anyplex Mycobacterium tuberculosis (nasopharyngeal lavage) | Not detectable |
Pericardial fluid analysis | |
color: reddish, appearance: cloudy, after centrifugation: transparent with blood bud, glucose: 89.5 mg/dl, proteins: 4.72gr, LDH 602.7, erythrocytes: full fields, crenates: 100% intact, leukocytes: not observed. Gram: no bacteria observed. | |
Adenosine D- Aminase ( U/L ) | 13.5 |
Reference Value: 37.3 sec. ** ADA Reference Value: 90 UL* ** Reference Value: 90 – 180. **** Reference Value: 10 - 40
Discussion
Systemic lupus erythematosus (SLE) is an autoimmune disorder with a variable presentation that affects multiple organs and systems. It is common in women of childbearing age [1] and is considered an independent risk factor for cardiovascular complications. Cardiac manifestations, present in up to 50% of cases, include conduction disorders, ischemia, cardiomyopathy, valve disease, and pericarditis [2]. The rapid progression of these entities to shock is rare [3] and potentially fatal, even in the initial stages of the disease.
Cardiac tamponade may be the initial manifestation of SLE in a small group of patients, as identified by Goswami RP et al., 2018, in their study where they only identified this entity in 2.5% of the initial cases. [4 -5].
Despite the low prevalence of SLE in men, compared to women, these patients tend to be more predisposed to developing serositis. [6] as evidenced in the ultrasound examination of the patient in question (ascites, pericardial effusion and pleural effusion) increasing the risk of possible secondary cardiac tamponade. In addition, the marked elevation of the erythrocyte sedimentation volume (ESR) together with the increase in C-reactive protein (CRP), complement consumption, normocytic anemia, concurrent renal disease and pleural effusion, predominantly on the left side, are considered risk factors. risk for massive pericardial effusion [5,7-8].
The presumed negative influence of ASA diuretics is striking, as a possible factor of progression to hemodynamic instability due to cardiac tamponade by reducing ventricular filling pressures, as described in the case of Cheng W et al, 2013, in a woman of 45 years [9] . On the other hand, we highlight the presentation with hypertensive crisis without changes in cardiac auscultation, so that the typical Beck triad [10]. was not met, ruling out the CT as a possible cause of precordial pain in the initial clinical approach. This finding was consistent with several cases of cardiac tamponade due to SLE in men, presumably explained by the initial compensatory adrenergic response. [9]. When comparing the age of our patient with other reported cases, this was consistent with what has been reported in the literature in patients who debut with CT [2, 7,9-11]. Additionally, in the review of the cases published in the last 10 years of CT as the initial presentation of SLE, the volume of fluid drained in our patient is the highest amount reported to date. (Table 2.)
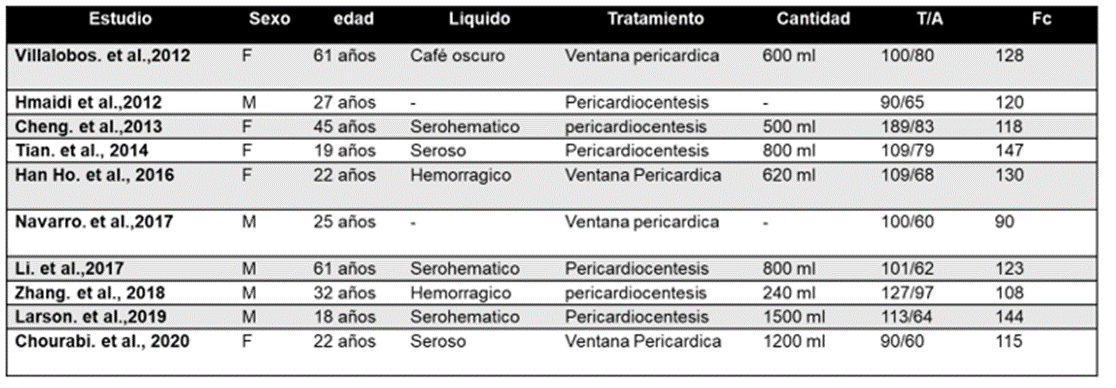
Table 2: Comparative analysis of the last 10 years of reported cases of cardiac tamponade as an initial symptom of systemic lupus erythematosus.
SLE-related pericardial effusions are mostly inflammatory exudates, with a serohematic (58%), serous (25%), and less frequently hemorrhagic (17%) appearance [6]. Failed pericardiocentesis, due to possible accumulation of posterior fluid and its density, added to the imminence of hemodynamic collapse, led to the emerging pericardial window in the ICU cubicle, an intervention that is necessary in less than 40% of patients with initial CT in SLE. [5, 12] The fluid obtained in our case was hemorrhagic, once other causes of pericarditis were ruled out, mainly infectious in our environment, with negative ADA and negative cultures, pulses of corticosteroids, antimalarials, and mycophenolate were started due to presumed concomitant lupus nephritis that conditioned the start of hemodialysis. [5]
The diagnosis of SLE was established based on positive clinical and immunological findings. According to the 2019 classification criteria of the European League Against Rheumatism (EULAR) [13] and the American College of Rheumatology (ACR), where ANA are a mandatory entry criterion, we obtained a value > 10 supporting supporting the diagnostic possibility. [14]
We highlight the importance of performing ultrasound at the patient's bedside, which is an important complement to the physical examination. In this case, it supported early diagnosis, changing the course of interventions performed on this patient by identifying potentially fatal entities.
Within the limitations of our case, we did not have a renal biopsy, but the finding of the urinalysis sediment, added to the patient's context, suggests that lupus nephritis was the cause of renal failure in our patient.
Conclusion
SLE affects any organ or system and its onset ranges from non-specific symptoms or infrequent potentially fatal conditions such as cardiac tamponade, which can lead to admission to the emergency department. High clinical suspicion and timely exploration with ultrasound are crucial for decision making and patient outcome. The causes of precordial pain in young men should not be underestimated, nor should SLE be ruled out as a cause of this entity.
References
- Larson NP, Frawley TC, Long B. Cardiac Tamponade in an 18-Year-Old Male with Undiagnosed Systemic Lupus Erythematosus. Cureus. 2019 Jul 21;11(7): e5186.doi :10.7759/cureus.5186. PMID: 31572632; PMCID: PMC6760573.
View at Publisher | View at Google Scholar - Zhang, Xuan MD *; Wu, Wenbin MD Cardiac plugging as an initial symptom due to systemic lupus erythematosus in a young man, Medicine: December 2018 - Volume 97 - Issue 51 - p e13708 doi: 10.1097/MD.0000000000013708
View at Publisher | View at Google Scholar - Raval, Jaydeep J et al. (2021). “SLE strikes the heart! A rare presentation of SLE myocarditis presenting as cardiogenic shock.” BMC cardiovascular disorders vol. 21,1 294. doi:10.1186/s12872-021-02102-6
View at Publisher | View at Google Scholar - Rosenbaum E, Krebs E, Cohen M, Tiliakos A, Derk CT. (2009) .The spectrum of clinical manifestations, outcome and treatment of pericardial tamponade in patients with systemic lupus erythematosus: a retrospective study and literature review. Lupus. 18(7):608-12. doi: 10.1177/0961203308100659. PMID: 19433460.
View at Publisher | View at Google Scholar - R P Goswami, G Sircar, A Ghosh, P Ghosh, (2018). Cardiac tamponade in systemic lupus erythematosus, QJM: An International Journal of Medicine, Volume 111, Issue 2, Pages 83–87, https://doi.org/10.1093/qjmed/hcx195
View at Publisher | View at Google Scholar - Cauduro SA, Moder KG, Tsang TS, Seward JB. (2003). Clinical and echocardiographic characteristics of hemodynamically significant pericardial effusions in patients with systemic lupus erythematosus. Am J Cardiol. 1;92(11):1370-1372. doi: 10.1016/j.amjcard.2003.08.036. PMID: 14636928.
View at Publisher | View at Google Scholar - Navarro-Ulloa, OD, Bello-Espinosa, A., Borre-Orange, D., Ramirez Barranco, R., Sarmiento Agamez, O., &ET, ALL. (2017). Pericardial effusion and cardiac plugging. Colombian journal of cardiology , 24 (6), 622.e1–622.e5. https://doi.org/10.1016/j.rccar.2017.04.009
View at Publisher | View at Google Scholar - [PubMed] Maharaj SS, Chang SM. (2015). Cardiac tamponade as the initial presentation of systemic lupus erythematosus: a case report and review of the literature. Pediatr Rheumatol Online J. 13:9. doi: 10.1186/s12969-015-0005-0. PMID: 25802493; PMCID: PMC4369869.
View at Publisher | View at Google Scholar - Cheng, W., Balachandar, R., & Mistry, P. (2013). Cardiac tamponade: an initial presentation of SLE. BMJ Case Reports, bcr2013200011–bcr2013200011. https://doi.org/10.1136/bcr-2013-200011
View at Publisher | View at Google Scholar - Beck, C. S. (1935). Two cardiac compression triads. JAMA: the journal of the American Medical Association, 104(9), 714. https://doi.org/10.1001/jama.1935.02760090018005
View at Publisher | View at Google Scholar - Topaloglu S, Aras D, Ergun K, Altay H, Alyan O, et. All., (2006). Systemic lupus erythematosus: an unusual cause of cardiac tamponade in a young man. Eur J Echocardiogr. 7(6):460-2. doi: 10.1016/j.euje.2005.07.010. Epub PMID: 16154807.
View at Publisher | View at Google Scholar - Ronderos Botero, DM, Fernandez-Avila, DG, Diaz Jimenez, MC, & Gutierrez Dávila, JM (2015). Cardiac plugging due to lupic pericarditis: report of two cases. Colombian Journal of Reumatología, 22(1), 63–70. https://doi.org/10.1016/j.rcreu.2015.01.003
View at Publisher | View at Google Scholar - Oku K, Atsumi T, Akiyama Y, Amano H, Azuma N, et al. (2018). Evaluation of the alternative classification criteria established by the Systemic Lupus International Collaborating Clinics (SLICC). Rheumatol Mod. Jul;28(4):642-648. doi : 10.1080/14397595.2017.1385154. Epub. PMID:29120258.
View at Publisher | View at Google Scholar - Aringer M, Johnson SR. (2020). Classifying and diagnosing systemic lupus erythematosus in the 21st century. Rheumatology (Oxford). 59(Suppl5): v4-v11. doi: 10.1093/rheumatology/keaa379. PMID: 33280013; PMCID: PMC7719035.
View at Publisher | View at Google Scholar

 Clinic
Clinic
