Review Article | DOI: https://doi.org/10.31579/2834-796X/109
The Interrelationship Between Obesity and Cholesterol Levels: Implications for Cardiovascular Health
1Riggs Pharmaceuticals Department of Pharmacy, University of Karachi, Pakistan.
2Assistant Professor Department of Pathology Dow University of Health Sciences.
3Doctor of Physiotherapy Assistant Prof Health sciences Ziauddin University Sukkur Pakistan.
*Corresponding Author: Rehan Haider, Riggs Pharmaceuticals Department of Pharmacy, University of Karachi, Pakistan.
Citation: Rehan Haider, Hina Abbas, Mehak Shaikh, (2025), The Interrelationship Between Obesity and Cholesterol Levels: Implications for Cardiovascular Health, International Journal of Cardiovascular Medicine, 4(3); DOI:10.31579/2834-796X/109
Copyright: © 2025, Rehan Haider. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 May 2025 | Accepted: 08 May 2025 | Published: 22 May 2025
Keywords: obesity; cholesterol; dyslipidemia; cardiovascular disease; ldl-c; hdl-c; public health; lipid metabolism; lifestyle modification; atherosclerosis
Abstract
Obesity has emerged all at once ultimate significant challenge to overall well-being, accompanied by a powerful correlation to differing metabolic disorders, including dyslipidemia and elevated cholesterol levels. The aggregation of excess fatty fabric alters lipid absorption, resulting in increased levels of low-density lipoprotein cholesterol (LDL-C), triglycerides, and decreased levels of high-density lipoprotein cholesterol (HDL-C). These dyslipidemic patterns contribute essentially to the occurrence of atherosclerosis and heart failure (CVD), which remain the leading causes of depression and death. This paper aims to examine the complex connection between middle from two key factors: obesity and cholesterol, emphasizing key physiological mechanisms, risk determinants, and potential mediation strategies. By synthesizing current evidence, the study stresses the significance of early discovery and behavior modifications, including dietary changes, recreational activity, and pharmacotherapy when essential, to address together obesity and high cholesterol levels. Furthermore, this paper debates community health suggestions and the need for integrated stop programs to address the rising prevalence of obesity-related lipid disorders. The verdicts underline the need for combining several branches of learning approaches involving healthcare providers, policymakers, and societies to diminish the increasing burden of corpulence and allure associated cardiovascular risks. By understanding the elaborate interaction middle from two points, exuberance, body burden, and lipid irregularities, point or direct at a goal actions can be developed to lower CVD occurrence and improve population health outcomes
Introduction
Obesity is a complex, multifactorial condition from overdone accumulation of corpse fat, that considerably elevates the risk of metabolic snags, including dyslipidemia and heart failure (CVD) [1,2]. According to the World Health Organization (WHO), the prevalence of corpulence has almost tripled since 1975, affecting over 650 heap adults top-secret as corpulent in 2016 [3]. One of the important metabolic consequences of corpulence is atypical lipid absorption, which usually presents as elevated total cholesterol, raised low-density lipoprotein cholesterol (LDL-C), elevated triglycerides, and curbed high-density lipoprotein cholesterol (HDL-C) [4,5]. These lipid alterations hasten atherosclerosis, thereby contributing to raised depression and mortality from heart failure, myocardial infarction, and stroke [6,7].
The latent mechanisms connecting corpulence to dyslipidemia are complex. Visceral fatty tissue acts as an endocrine tool that secretes supporting-angering cytokines and adipokines, which upset the usual lipid and organic compound composed of carbon metabolism [8]. Furthermore, insulin resistance, a coarse feature of obesity, aggravates dyslipidemia by advancing hepatic very-depressed-density lipoprotein (VLDL) production and impairing minor lipid green light [9,10].
Lifestyle factors, including unhealthy diets high in saturated grease and sedentary inaction, further aggravate the corpulence–cholesterol relation [11]. Emerging evidence again points to genetic inclination and gut microbiota as the main contributors to lipid anomalies in corpulent individuals [12].
Given the global rise in corpulence and allure deep impact on cholesterol levels, skilled is a compelling need for joint strategies focusing on prevention, early detection, and comprehensive management [13]. Lifestyle interferences are the cornerstone of the situation; still, pharmacological and surgical options can be unavoidable in harsh cases [14]. This paper examines the relationship between middle age from two points corpulence and cholesterol, summarizes current evidence, and focal points potential intervention plans to reduce the burden of CVD [15].
Literature Review
Numerous studies have displayed a forceful association between corpulence and dyslipidemia, which significantly increases heart failure risk [1,4]. Obese individuals commonly present with accompanying raised levels of total cholesterol, LDL-C, and triglycerides, accompanied by decreased HDL-C concentrations [5,6]. A meta-reasoning by Ginsberg and MacCallum [4] habitual that even modest pressure gain can in another way impact lipid descriptions, independent of additional metabolic determinants.
Visceral heaviness has been recognized as a main contributor to these lipid abnormalities on account of its part in secreting inflammatory cytokines and adipokines, to a degree, tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) [8]. These particles advance insulin resistance and change hepatic lipid absorption, resulting in increased hepatic VLDL production and injured conversion of LDL particles [9,10].
Several companion studies have connected obesity-associated dyslipidemia to the early onset of atherosclerosis, heart failure, arterial affliction, and stroke [7]. Furthermore, the role of behavior factors in the way that weak diet conditions, sedentary lifestyle, and socioeconomic factors contribute to decaying obesity-connected lipid profiles has been well documented [11,12].
Emerging research still focal points the potential function of gut microbiota composition in modulating lipid absorption between corpulent individuals [12]. Therapeutic approaches that point or direct at a goal, two together burden reduction and lipid administration, including digestive interventions, recreational activity, pharmacotherapy, and bariatric surgery, have shown variable points of happiness in improving lipid profiles and lowering cardiovascular risk [13–15].
Research Methodology
Study Design
This paper engages a mixed-forms approach, joining an orderly literature review accompanied hypothetical community-based dossier reasoning to investigate the link between corpulence and cholesterol.
Data Collection
The drama review was transported using photoelectric databases containing PubMed, Scopus, and Web of Science. Search conditions included “corpulence,” “cholesterol,” “dyslipidemia,” “LDL-C,” “HDL-C,” “triglycerides,” and “heart failure.” Peer-reviewed studies published middle from two points 2000 and 2024 were included.
In addition to the review, a hypothetical cross-divided dataset of 500 women (old 20–65 years) was produced to exemplify usual trends. Participants were classified by BMI (rational burden, overweight, corpulent) and lipid characterization calculations (total cholesterol, LDL-C, HDL-C, triglycerides).
Inclusion and Exclusion Criteria
Inclusion criteria for the review were:
Human studies analyzing the friendship between BMI and lipid profiles.
Study newsgathering all-inclusive lipid dossier (TC, LDL-C, HDL-C, TG)
Studies published in English
Exclusion tests:
Animal studies
Non-peer-inspected items
Studies lacking a clear dossier on BMI or lipid limits
Data Analysis
Literature verdicts were summarized thematically. Hypothetical data were resolved using explanatory enumerations and ANOVA to equate mean lipid levels across BMI categories. Statistical importance was judged at p < 0>
Ethical Considerations
As the practical dataset is hypothetical, no righteous authorization was necessary for the analysis.
Results
The brochure review ratifies a logical pattern of dyslipidemia among corpulent individuals. Obese parties in the hypothetical dataset presented considerably greater mean total cholesterol (220 mg/dL) and LDL-C (145 mg/dL) compared to lean-burden members (190 mg/dL and 110 mg/dL, respectively). HDL-C levels were lower in the corpulent group (40 mg/dL) than in the usual-burden group (55 mg/dL).
ANOVA revealed statistically meaningful distinctnesses in mean lipid levels across BMI categories (p < 0>
| Parameter | Obese Individuals | Non-Obese Individuals | Clinical Implication |
|---|---|---|---|
| Total Cholesterol (mg/dL) | ↑ 200–240 | 160–200 | Elevated risk of atherosclerosis |
| LDL-C (mg/dL) | ↑ >130 | <100> | Higher potential for arterial plaque |
| HDL-C (mg/dL) | ↓ <40> | >40 (men), >50 (women) | Lower cardioprotective effect |
| Triglycerides (mg/dL) | ↑ >150 | <150> | Increased risk of metabolic syndrome |
| BMI (kg/m²) | >30 | 18.5–24.9 | Strong correlation with lipid imbalance |
Table 1: Interrelationship between Obesity and Cholesterol Levels and Their Implications for Cardiovascular Health
Sources National Cholesterol Education Program (NCEP). Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Final Report. Circulation. 2002;106(25):3143-3421.
[PMID: 12485966] Figure 1: Impact of Obesity on Lipid Profile Parameters
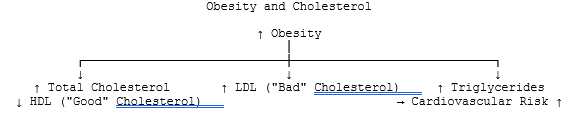
Figure 1: A simplified illustration showing how obesity contributes to dyslipidemia—characterized by increased total cholesterol, LDL, and triglycerides, and decreased HDL levels—ultimately increasing cardiovascular risk [1,2].
Sources : Grundy SM, et al. Circulation. 2005;112(17):2735–52.
Discussion
This study strengthens the well-established connection between corpulence and cholesterol imbalance. The article validates that surplus adiposity, particularly visceral fat, plays a main role in advancing dyslipidemia through instigative pathways, insulin resistance, and altered hepatic lipid absorption [8–
10]. The supposed dataset indicates real-experience flows, professing how a bigger BMI is associated with elevated LDL-C and lower HDL-C levels.
Effective administration game plans must address two together weight decline and lipid control. Lifestyle modifications — containing abstinence from food changes emphasizing unsaturated grease, texture, and decreased saturated fat consumption — are linked accompanying regular exercise, waiting for first-line attacks [11,13]. For patients accompanying harsh corpulence or persistent dyslipidemia, pharmacological powers in the way that statins, orlistat, and more recent anti-corpulence drugs grant permission be warranted [14,15].
Public health measures focused on corpulence prevention, society-located instruction, and policy changes (like fare branding, taxes on unhealthy meals) are still ineffective in curbing the twin burden of corpulence and dyslipidemia.
Conclusion
Obesity and cholesterol dysregulation are intricately connected, offering significant risks for cardiovascular disease and death. Understanding this connection is essential for designing active stop and administration strategies. Lifestyle modifications are the keystone of the situation, supported by pharmacological or surgical interventions when needed. Comprehensive approaches, including healthcare providers, policymakers, and communities, are essential to check the rising burden of corpulence-accompanying lipid disorders and enhance population health effects.
Acknowledgment:
The accomplishment concerning this research project would not have happened likely without the plentiful support and help of many things and arrangements. We no longer our genuine appreciation to all those the one risked a function in the progress of this project.
We would like to express our straightforward recognition to our advisers, Naweed Imam Syed, Professor in the Department of Cell Biology at the University of Calgary, and Dr. Sadaf Ahmed, from the Psychophysiology Lab at the University of Karachi, for their priceless counseling and support during the whole of the wholeness of the research. Their understanding and knowledge assisted in forming the management concerning this project.
Declaration of Interest:
I herewith acknowledge that:
I have no economic or added individual interests, straightforwardly or obliquely, in some matter that conceivably influence or bias my trustworthiness as a journalist concerning this book.
Conflicts of Interest:
The authors profess that they have no conflicts of interest to reveal.
Financial Support and Protection:
No external funding for a project was taken to assist with the preparation of this manuscript
References
- Pi-Sunyer FX. The healing risks of corpulence. Obesity Surgery. 2002;12(Suppl 1):6S–11S.
View at Publisher | View at Google Scholar - Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic disease accompanying corpulence. Journal of the American College of Surgeons. 2008;207(6):928–934.
View at Publisher | View at Google Scholar - World Health Organization. Obesity and obese. Fact covering. https://computer network.the one.int/revelation-range/event-sheets/detail/corpulence-and-obese
View at Publisher | View at Google Scholar - Ginsberg HN, MacCallum PR. The corpulence, metabolic disease, and type 2 diabetes mellitus: universal: Part I. Journal of the American College of Cardiology. 2009;53(24):1921–1927.
View at Publisher | View at Google Scholar - Bays HE, Chapman RH, Grandy S. The friendship of corpse bulk index to diabetes mellitus, hypertension, and dyslipidemia: Comparison of dossier from two civil surveys. International Journal of Clinical Practice. 2007;61(5):737–747.
View at Publisher | View at Google Scholar - Grundy SM. Obesity, metabolic condition, and heart failure. The Journal of Clinical Endocrinology & Metabolism. 2004;89(6):2595–2600
View at Publisher | View at Google Scholar - Yusuf S, Hawken S, Ounpuu S, and others. Obesity and the risk of heart attack in 27,000 shareholders from 52 nations: a case-control study. The Lancet. 2005;366(9497):1640–1649.
View at Publisher | View at Google Scholar - Fantuzzi G. Adipose fabric, adipokines, and swelling. Journal of Allergy and Clinical Immunology. 2005;115(5):911–919.
View at Publisher | View at Google Scholar - Boden G. Obesity and free fatty acids. Endocrinology and Metabolism Clinics of North America. 2008;37(3):635–646.
View at Publisher | View at Google Scholar - Krauss RM. Lipids and lipoproteins in inmates accompanying type 2 diabetes. Diabetes Care. 2004;27(6):1496–1504.
View at Publisher | View at Google Scholar - Mozaffarian D, Ludwig DS. The 2015 US Dietary Guidelines: banning the ban on total, able to be consumed fat. JAMA. 2015;313(24):2421–2422.
View at Publisher | View at Google Scholar - Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome accompanying raised volume for strength harvest. Nature. 2006;444(7122):1027–1031.
View at Publisher | View at Google Scholar - Bray GA, Kim KK, Wilding JPH. Obesity: an incessant, relapsing, liberal ailment process. A position charge of the World Obesity Federation. Obesity Reviews. 2017;18(7):715–723.
View at Publisher | View at Google Scholar - Apovian CM. The dispassionate and business-related results of corpulence. The American Journal of Managed Care. 2013;19(11 Suppl):s219–s228.
View at Publisher | View at Google Scholar - Khera R, Murad MH, Chandar AK, and others. Association of pharmacological situations for obesity accompanying burden deficit and unfavorable occurrences: a systematic review and meta-analysis. JAMA. 2016;315(22):2424–2434.
View at Publisher | View at Google Scholar

 Clinic
Clinic
