Research Article | DOI: https://doi.org/10.31579/2834-5118/064
Role of Matriderm in Wound Bed Preparation in Thermal Burns
1Department of Plastic Surgery JIPMER Puducherry, India – 605006.
2Senior Professor and Associate Dean (Academic), Head of IT Wing and Telemedicine, Department of Plastic Surgery and Telemedicine JIPMER Puducherry, India – 605006.
*Corresponding Author: Ravi Kumar Chittoria, Senior Professor and Associate Dean (Academic), Head of IT Wing and Telemedicine, Department of Plastic Surgery and Telemedicine JIPMER Puducherry, India
Citation: Kanav Gupta, Ravi K. Chittoria, (2025), Role of Matriderm in Wound Bed Preparation in Thermal Burns, International Journal of Clinical Surgery, 4(4); DOI:10.31579/2834-5118/064
Copyright: © 2025, Ravi Kumar Chittoria. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 04 August 2025 | Accepted: 15 August 2025 | Published: 29 August 2025
Keywords: matriderm; gluteal burns; thermal burns; dermal substitute
Abstract
Dermal substitutes have been a breakthrough in plastic surgery. They are being increasingly used in the partial and full thickness deep burns for better pliability and elasticity. Matriderm is one such dermal substitute – porous, single layered collagen matrix which promotes dermal formation and preserves native collagen fiber bundles and fibril structures.[1] In this study, matriderm was used in case of full thickness thermal burns over the gluteal region which was later grafted easily.
Introduction
Burn injuries remain a serious global epidemiologic concern. The majority of burn injuries in adults tend to be thermal injuries, making up over 65% of cases. Burn wound management is the focus once the patients with burn injuries have had their critical care difficulties stabilized. The ultimate goals of burn restoration techniques are to conceal injuries, reestablish function, and maintain appearance. The three main surgical procedures for managing a wound are excision, grafting, and reconstruction [3]. Early excision and skin grafting minimize necrotic and diseased tissue while simultaneously enabling the first acute covering of burns. Regenerative treatments such as matriderm aid in the improvement of scar formation and the repair of second-degree superficial burns. Matriderm serves as scaffolding for the growth of a neodermis. Blood vessels and other cells migrate into the matrix and begin to lay down a new layer of dermis earlier as compared to other dermal substitutes as it has non-cross-linked collagen which helps easier angiogenesis.
Materials and Methods
This study was conducted in Tertiary Care Centre in Department of Plastic Surgery after getting the department ethical committee approval. Informed consent was obtained. The subject was a 37-year- old male who had accidental thermal burn injury sustaining 15 percentage burns to the bilateral gluteal region with deep burns (Figure 1). He was admitted in burns care ICU. He underwent wound debridement of the burns and split thickness skin grafting under general anaesthesia (Figure2). But due to unhealthy bed and exposed fat, graft did not take post which matriderm 1 mm thickness 5x5 cm was cut in small bits and applied to the raw area over which negative pressure wound therapy (NPWT) was applied (Figure 3). The burn wound improved and healthy granulation was present as seen on 7th day post which grafting was done. Matriderm was used in the patient to achieve the adequate granulation over fat in gluteal region. (Figure4).
Results
Intra-operative and post-operative periods were uneventful for the patient. The raw area took up the matriderm and burn wounds granulated well. Split skin grafting was done to the raw area (figure 4). The wounds healed well after 2 weeks with minimal scarring (Figure5). No complications and side effects were noted.

Figure 1: Full thickness burn wound over left gluteal region on presentation

Figure 2: Post eschar excision and debridement


Figure 3a, b: Matriderm 1mm thickness placement
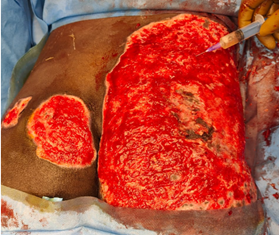
Figure 4: Healthy wound bed for future grafting

Figure 5: Post grafting and take of graft
Discussion
The utilization of appropriate scaffold matrices is ultimately what drives skin tissue regeneration. Scaffolds can be porous, fibrous, microsphere-shaped, hydrogel-based, composite, or a cellular. Ulcers that don't heal well, post-burn ulcers, larger area wounds that need to be covered require skin grafting or flap covering, depending on the situation. The greatest biological substance to cover a wound is skin. Certain situations prevent a patient from receiving skin grafting, such as major burns when additional skin is needed to cover a wound because sufficient skin is not present or in case of deep burns where graft does not take adequately. We require biological material that is both efficient and economical to cover the wound and act as a barrier against wound infection. Matriderm is thought to be a significant prospective source of scaffolding material.
Four distinct phases of dermal regeneration have been observed—imbibition, fibroblast migration, neovascularization, and remodeling and maturation. Imbibition occurs within minutes and the initial take of the matrix is enhanced via fibrin in the wound exudate. Swelling of the matrix during this period is expected. Around day seven, fibroblasts begin migration into the matrix. In the third week, myofibroblasts arrive and begin depositing native collagen within the matrix. By week four, host collagen is dominant and replaces the matrix collagen. During this stage, the neo dermis is thicker than host dermis, but through maturation, the neodermis thins and gains pliability. By the end of week four, the neo dermis is fully vascularized. This can be appreciated clinically by the color progression from pink to pale yellow to peach. Other groups have found vascularization to be complete after two weeks; however, these studies were in patients with acute burns and the earlier vascularization may be attributed to increased metabolism and systemic inflammatory response. [3] It is important to note that once the neo dermis has formed, no adnexa, nerve endings, or elastic fibers will be present. After the neo dermis is fully vascularized, it is ready to receive a graft. Once the graft is placed, the dermal–epidermal junction will develop rete ridges. [4]
Both Integra and Matriderm matrices demonstrated progressive cellular infiltration and vascularization; however, Matriderm showed a faster rate of neovascularization. [4] Endothelial cell infiltration, marked by CD31 expression, was evident by the second week, with lumen formation and vessel maturation by the third week. In contrast, Integra typically shows substantial neovascular development by the fourth week, aligning with its recommended delayed grafting approach.
Matriderm is composed of non-crosslinked collagen and shows early degradation, with substantial thinning by the second week and near-complete resorption by two months. The early inflammatory response seen with Matriderm- characterized by neutrophil and macrophage infiltration- helps facilitate early readiness for graft take. [5]
Dickson et al demonstrated that despite concerns regarding scaffold thickness and imbibition, the 1 mm Matriderm matrix facilitated successful one-stage grafting, especially when supplemented with occlusive dressings to preserve graft hydration. However, clinical outcomes were less favorable with 2 mm Matriderm, where excessive thickness impaired graft take. This highlights the importance of matrix architecture in facilitating graft survival and vascular integration. [2,6]
Overall, this study supports the clinical utility of 1 mm Matriderm in promotion of wound bed preparation offering accelerated integration and early vascular support. However, its rapid degradation, inflammatory response, and variable elastin incorporation suggest a need for further refinement.[7] Comparative long-term studies examining functional, histological and aesthetic outcomes will be critical to determine optimal matrix selection in burn and reconstructive surgery.
Conclusion
Matriderm plays a role in burn wound healing. It helps in promoting the wound healing process and wound bed preparation. It helps in better healing of second-degree partial thickness burns and wound bed preparation for deep burn wounds for further intervention.
Conflict of Interest
None declared.
References
- Ryssel H, Gazyakan E, Germann G, Ohlbauer M. (2008). The use of MatriDerm in early excision and simultaneous autologous skin grafting in burns--a pilot study. Burns. Feb;34(1):93-97.
View at Publisher | View at Google Scholar - Dickson K, Lee KC, Abdulsalam A, Amirize E, Kankam HKN, et al., (2023). A Histological and Clinical Study of MatriDerm® Use in Burn Reconstruction. J Burn Care Res. Sep 7;44(5):1100-1109.
View at Publisher | View at Google Scholar - Moiemen NS, Staiano JJ, Ojeh NO, Thway Y, Frame JD. (2001). Reconstructive surgery with a dermal regeneration template: clinical and histologic study. Plast Reconstr Surg; 108:93–103.
View at Publisher | View at Google Scholar - Zuijlen PP, van Trier AJ, Vloemans JF, Groenevelt F, Kreis RW, Middelkoop E. (2000). Graft survival and effectiveness of dermal substitution in burns and reconstructive surgery in a one-stage grafting model. Plast Reconstr Surg; 106:615–623.
View at Publisher | View at Google Scholar - Moiemen NS, Vlachou E, Staiano JJ, Thawy Y, Frame JD. (2006). Reconstructive surgery with Integra dermal regeneration template: histologic study, clinical evaluation, and current practice. Plast Reconstr Surg;117(7 Suppl):160S–174S
View at Publisher | View at Google Scholar - Böttcher-Haberzeth S, Biedermann T, Schiestl C et al. (2012). Matriderm® 1 mm versus Integra® Single Layer 1.3 mm for one-step closure of full thickness skin defects: a comparative experimental study in rats. Pediatr Surg Int; 28:171–177
View at Publisher | View at Google Scholar - Ryssel H, Germann G, O hlbauer M. (2008). The use of Matriderm in early necrectomy and onestep autologous skingrafting Burns; 34:93–97.
View at Publisher | View at Google Scholar

 Clinic
Clinic
