Review | DOI: https://doi.org/10.31579/2834-8745/024
Juvenile Diabetes
1Department of Chemistry, Sri J.N.M.PG College,Lucknow UP, India.
2Department of Chemistry,Dayanand Girls PG Kanpur, UP, India.
*Corresponding Author: D.K. Awasthi, Department of Chemistry, Sri J.N.M.PG College. Lucknow UP, India.
Citation: D.K. Awasthi, Dixit A. (2024). Juvenile Diabetes. Journal of Scientific Research and Biomedical Informatics 3(6); DOI:10.31579/2834-8745/024
Copyright: © 2024 D.K. Awasthi, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 17 October 2024 | Accepted: 24 October 2024 | Published: 31 October 2024
Keywords: juvenile diabetes; glucose; blood test; urine test
Abstract
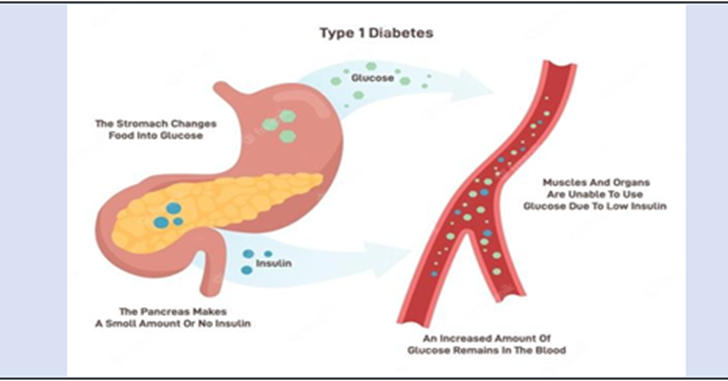
Diabetes is a condition in which the body can't make enoughinsulin, or can't use insulinnormally. Type 1 diabetes is an autoimmune disorder. The body's immune system damages the cells in the pancreas that make insulin. Insulin is a hormone.It helps sugar (glucose) in the blood get into cells of the body to be used as fuel. When glucose can’tenter the cells, it builds up in the blood. This is called high blood sugar (hyperglycaemia). High blood sugar can cause problems all over the body. It can damage blood vessels and nerves. It can harm the eyes, kidneys, and heart. It can also cause symptoms such as tiredness.
Introduction
Juvenile diabetes is mostly an autoimmune disorderand is also referredto as type 1 diabetesAs the name suggests, the disease is commonly diagnosedin childhood or adolescence (as opposed to type 2 or “adult-onset” diabetes, which occurs most often in middle age). In truth though, juvenile/type 1 diabetes doesn’t only happen in kids—it’s possible, though lesscommon, for adults to get it, too. Similarly, children can and sometimes do get type 2. Accordingto the most recent figure, about 283,000 kids and teens have diabetes; approximately 244,000 of those cases are juvenile diabetes. People with all types of diabetes share one thing in common:High amounts of sugar, or glucose, in their blood.
How Glucose Works
After you eat, your body breaks down the food into glucose (a.k.a. sugar) and other substances, which then enter the bloodstream. In response, your pancreas releases insulin,a type of hormone that helps muscleand fat cells suck up the glucose and use it for energy. But in kids with juvenile diabetes, the body’s immune system gets confused and starts attacking the beta cells in the pancreas that make insulin, shutting down production. Without insulin to help guide glucose into the body's cells, sugar starts to build up in the bloodstream, leading to a host of health issues.
Who Gets JuvenileDiabetes?
About 37.3 million people in the United States have been diagnosedwith diabetes, and 5% to 10% of those cases are juvenile (type1). That works out to about one in 250 people; of those, about three-quarters are diagnosedwith juvenile diabetes during childhood or young adulthood. The most common age for a juvenile diabetes diagnosis is between 10 and 16, possibly because pubertytriggers an increasein hormone production and these hormones, including oestrogen and testosterone can affect blood sugar levels.
Possible factors that play a role in the development ofthe disease:
Ethnicity and geography: Juvenile diabetes becomes more common the further away you live from the equator. For instance, childrenin Scandinavian countries have a much higher risk of beingdiagnosed with the disease. And Caucasians of Northern Europeanancestry have a higher risk than otherethnicities.
Genetics: Although there is no juvenilediabetes “gene,” there are several genes and mutations that have been identified as increasing your risk for it. In particular, mutations in the human leukocyte antigen(HLA) class of genes, which are related to the immune system, can raise the risk of autoimmune conditions like juvenilediabetes.
Family history: If autoimmune conditions run in your family, that means your child is at higherrisk of developing one, too. Some studiessuggest that if a sibling or parent has type 1 diabetes, kids have a 15 times higher risk of developing the condition than someonewithout any familyhistory.
Toxins and infections: Doctors believe that in most cases, a toxin or virus triggers the start of juvenile diabetes. This “foreign invader” kicks the immune system into gear, causing it to mistakenly attack thepancreas and kill off insulin-producing beta cells.
Tests for Juvenile Diabetes: The first step in getting a diabetes diagnosis is a blood test to look for elevatedglucose levels. If your child is diagnosed with high blood sugar, then the doctor will want to perform additional tests to identify the specific type of diabetes. Correct diagnosisis very important since treatment is different for each type. Your child may need one or more of the below:
Blood Tests
A1C (or glycatedhemoglobin) test: Thistest measures what percentage of red blood cells have been coated with glucose over the past two to three months and is the most common test for diabetes. The higher a child’s blood sugar, the higher his score. An A1C result below 5.7 is considered normal; 5.7 to 6.4 is prediabetic; 6.5 or abovesuggests diabetes.
Fasting blood sugar test: Blood will be drawn firstthing in the morning before your child eats or drinks anythingother than water. A result under 100 milligrams per deciliter is normal; 100 to 125 mg/dL is prediabetic; 126 mg/dL indicates diabetes. The doctor will likely want to do the test twice before officially diagnosing your child.
Random blood sugar test: Blood is drawn at any time of day, whether your child has eaten recently or not. A resultof 200 mg/dL indicates diabetes.
Antibody test: To help differentiate between juvenile diabetes and other types, a doctor may also want to draw blood for an “autoantibody” test. This test will show if your child’s immune system is attacking thepancreas. Kids with juvenile diabetesoften test positive for several specific autoantibodies, while those with type 2 don’t.
Urine Test
Your child’s doctor may want to test his urine for ketones. The test can generally be done at home or in a doctor’s office by peeinginto a specimen cup. If you’re doingthe test at home, it will come with paper test stripsto dip into the urine. Extremely high levels of ketones are a sign of ketoacidosis, a potentially fatal complication of diabetes that requires immediatetreatment.
Treatment
Treatment for Juvenile Diabetes
All children with juvenile diabetes need to regularly check their blood glucose levels,take insulin daily, and be mindful of what they eat—not because diet can cure juvenilediabetes (it can’t), but because large meals or those high in carbohydrates rely on high doses of insulin to manage blood sugar levels, and your child’sbody isn't able to producethat insulin.
Checking GlucoseLevels
Kids with juvenile diabetesmay need to check (or have someone help check) their blood glucose four to 10 times a day in order to make decisions about insulin dosages,food, and exercise choices. This can be done with a home glucose meter. To use it, the child’s fingertip is pricked with a specialized lancet “pen,” then blood is droppedonto a test strip in the meter. In some cases, a doctor might suggest a continuous glucose monitor, a tiny sensor that is insertedunder the skin of the abdomen, arms, or thigh to check glucose levels regularly. The sensor will alert your child if levels fall too low.
Taking Insulin
Insulin, which people with juvenile diabetesneed daily, can’t be takenas a pill because it would be broken downand digestedbefore getting into your blood.
There are a couple of different ways insulin can be delivered to the body:
Injection: This is the most common way to take insulin. Your child (or someone helpinghim) will use a syringe or “pen” to inject the drug, usually in the belly, upper arm, thigh, or butt. Kids may need four or more injections a day.
Insulin Pump: Children who need multipleinjections per day or are high risk of ketoacidosis may prefer an insulin pump, which automatically delivers insulin throughout the day through a tiny catheter that’s worn on the body.
Insulin Types
The type of insulin your child take depends on several factors, including how long it takes the body to absorb insulin; your child’s diet and exercisehabits; and tolerance for injections. A pediatrician will help determine what’s best for your child. These are the common options:
Rapid-Acting Insulin: This medication starts to work within about 15 minutes of taking it (often just before a meal to prevent blood glucose from rising). It works for two to four hours. Examples include Humalog(lispro) and Novolog (aspart).
Short-Acting Insulin: Also called“regular” insulin, this med takesabout 30 minutesto kick in. It is taken beforea meal to help lower increased levels of bloodsugar while eating.It works for three to six hours.Examples include Humulin R and Novolin R. Intermediate-Acting Insulin: Often combined with rapid-acting insulin,this med startsworking about two to four hours after taking and balancesthe body’s glucose levels for 12 to 18 hours. Examplesinclude Humulin N and Novolin N (NPH).
Long-Acting Insulin: These meds can take up to six hoursto reach the bloodstream. They work to maintain lower blood sugar levels for up to 26 hours.Examples include Lantus (insulin glargine) and Levemir (insulin detemir).
Ultra-long-acting Insulin: Reaches the blood stream in 6 hours,does not peak,and lasts about 36 hoursor longer. Examplesinclude Degludec (Tresiba), Glargine u-300 (Toujeo).
Living With
Type 1 diabetes, also called juvenilediabetes, occurs when the body’s immune systemdestroys cells in the pancreasthat create insulin.Insulin is a hormone that takes sugar (known as glucose) from your bloodstream and delivers it into your cells to be used for energy. Without insulin,your blood sugarlevels remain high which can lead to serious health complications overtime. Because their bodies don’t make insulin,children with Type 1 diabetes must get insulin from multiple daily injections or an insulin pump. They also must test their blood sugar levels throughout the day and pay specialattention to eating,drinking, and exercising. Managing your child’s Type 1 diabetes can sometimes seem overwhelming. The Duke Children’s diabetes care team can help you overcome these challenges. We offer expert medical guidance and give you and your child information, support,and encouragement to manage and live well with diabetes.
Type 1 diabetes is a life-threatening, life-long disease that is characterized by the lack of insulin, causingexcessively elevated glucosein a person's blood (called hyperglycemia). Type 1 diabetesis the most common form of diabetes in childhood. About 1 in every 350 children in the United States has type 1diabetes. It can appear in children as young as 6 months of age, although the most common age is around 12. Type 1 diabetesis becoming more frequent than before, particularly among children younger than 5 years ofage. Adults can also developtype 1 diabetes.
Around 95% of cases of type 1 diabetes are caused by autoimmunity, that is, the body's defensesystem (called immune system) attacking its own cells, in this case, the insulin-producing cells in the pancreas (beta- cells). The ultimatereason for this attack is unknown.However, we know that there are inherited (genetic) and environmental factors. Relatives of a patient with type 1 diabetes have increased risk of developing the disease:about 70% for identical twins, 6% of siblings and non-identical twins, 6% for children of a father with type 1 diabetesand 4% for a motherwith type 1 diabetes. Certain genes (HLA types) make type 1 diabetes more likely. additionto genes and family history. Research studiesare ongoing with the ultimategoal of findingsafe and effective treatments to preventto type 1 diabetes in individuals at risk. Type 1 diabetes mellitus is a long-term (chronic)condition. It may start at any age. Insulin from the pancreas must be replaced with insulin injections or an insulinpump.
There are two forms of type 1 diabetes:
Immune-mediated diabetes. This is an autoimmune disorder in which the body's immune system damages thecells in the pancreas that make insulin.This is the most commonkind of type 1 diabetes.
Idiopathic type 1. This refers to rare forms of the disease with no known cause.
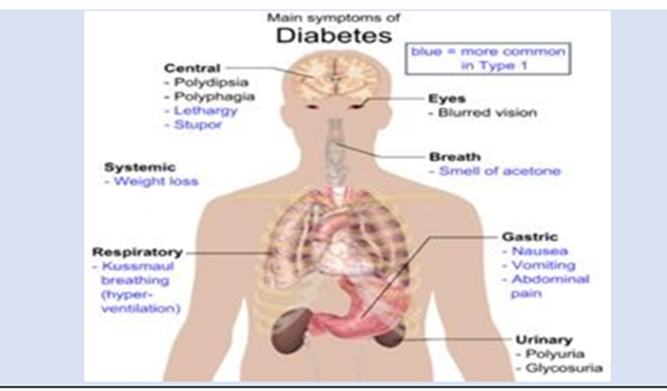
Symptoms & Types
Symptoms of diabetes include increased urination (caused by the kidneysflushing excessive bloodglucose), increased thirst (the body's compensatory mechanismof the fluid loss throughurine) and weight loss (caused by the loss of glucose through the kidneys, among other factors). Other symptoms includetiredness and mood changes, bedwetting (consequence of increased urination), blurry vision and infections (skin,urine, vaginal). If left untreated, increased glucose levels lead to additional complications, such as diabetic ketoacidosis (DKA),
which is lifethreatening. At this stage, patients have nausea, vomiting,abdominal pain and abnormal breathingfollowed by loss of consciousness and potentially death.
Early diagnosis of type 1 diabetes is critical to prevent development of this fatal complication.
Type1 diabetes often appears suddenly.In children, type 1 diabetessymptoms may be like flu symptoms. Symptoms can occur a bit differently in each child.They can include:
High levels of glucose in the blood and urine when tested.
Unusual thirst.
Dehydration.
Frequent urination (a baby may need more diaper changes, or a toilet-trained child may start wetting his or her pants).
Extreme hunger but weight loss.
Loss of appetite in younger children.
Blurred vision.
Nausea and vomiting.
Belly (abdominal) pain.
Irritability and mood changes.
Serious diaper rash that does get better with treatment.
Fruity breath and fast breathing. Yeast infection in girls.
Yeast infection in girls.
Diagnosis &Tests
Diagnosis of type 1 diabetes requires a test of blood glucose. Patients with clearly elevatedglucose in bloodwill also have glucose in their urine; however, glucose inurine can be normal at certain times of the day and therefore a normal urine test does not rule out diabetes. At the early stages of diabetes, blood glucosecan be normal at certain times ofthe day, and a special test called oral glucose tolerance test (OGTT), which is done by measuringblood glucose 2 hours after drinking a glucose load may be necessary to demonstrate that someone has diabetes. Once a patient is diagnosed with diabetes, several tests are conducted to diagnose the type of diabetes (for example, diabetes autoantibodies are typical of type 1 diabetes) and the presenceof complications (for example, DKA) and other conditions that are present more frequently (for example, thyroid abnormalities). To diagnose risk of type 1 diabetes,islet autoantibodies are measured in blood. Genetic tests and measurement of the ability to produce insulinhelp better estimatethe risk and establish the stage of the progression.
GlucoseTests
Fasting plasma glucose: The blood is tested after at least 8 hours of not eating.
Random plasma glucose: The blood is tested when there are symptoms of increased thirst,urination, and hunger.
Children with type 1 diabetes must have daily injections of insulin to keep the blood glucose level within normal ranges. Insulinis given either by injection or insulin pump. Your child’s healthcare provider will show you how to give your child insulin with either method.
Treatment will also include:
Eating the right foods to manageblood glucose levels. This includes timing meals and counting carbohydrates.
Exercise, to lower blood sugar.
Regular blood testing to check blood-glucose levels.Regular urinetesting to check ketone levels.
Type 1 diabetes can cause
Ketoacidosis: This is when blood sugar levels are very high and the body starts making ketones. This is a very serious condition that needs to be treated right away in the hospital, sometimes in the intensive care unit. If your child is not treatedright away, they are at risk for diabetic coma. A child with a diabetic coma loses consciousness because of brain swelling. The brain swells because of the veryhigh blood sugar levels.
Low blood sugar(hypoglycaemia): This isalso sometimes called an insulinreaction. This occurs whenblood glucose drops too low.
Your child’s healthcare provider will tell you how to avoid these problems.
Over time, high blood sugar levelscan damage bloodvessels. Balancing insulin,diet, and activitycan help keep blood sugar levels in the target range and help prevent complications such as:
Eye problems, Kidney disease, Nerve damage,Tooth and gum problems, Skin and foot problems, Heart and bloodvessel disease
Conclusion
Type 1 diabetes mellitus is a long-term (chronic) condition. It may start at any age. Only 5% of people with diabetes have type 1, Type 1 diabetes is a condition in which blood glucose levels are abnormally high. It is most frequently caused by an autoimmune disorder in which the body's immune system destroys the cells in the pancreasthat produce insulin. Children with type 1 diabetes must have dailyinjections of insulin to keep the blood glucose level within normal ranges. Without insulin,blood glucose levelscontinue to rise and death will occur.With the administration of insulin, and other management activities, childrenwith type 1 diabetes can lead active,healthy lives.
References
- Lucier J, Weinstock RS, Doerr C. (2021). Diabetes Mellitus Type 1 (Nursing).
View at Publisher | View at Google Scholar - Goodman CC, Snyder TEK. (2013). Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier, 425-432.
View at Publisher | View at Google Scholar - (2021). Diabetes SA Diabetes type 1.
View at Publisher | View at Google Scholar - (2016). American Diabetes Association. Type 1 Diabetes.
View at Publisher | View at Google Scholar - (2021). Diabetes aus.
View at Publisher | View at Google Scholar - Franc S, et al. I (2016). Insulin-based strategies to prevent hypoglycaemia during and after exercise in adult patients with type 1 diabetes on pump therapy: the DIABRASPORT randomized study. Diabetes, Obesity, and Metabolism.
View at Publisher | View at Google Scholar - Alarcón-Gómez J, Chulvi-Medrano I, Martin- Rivera F, Calatayud J. (2021). Effect of High- Intensity Interval Training on Quality of Life, Sleep Quality, Exercise Motivation and Enjoyment in Sedentary People with Type 1 Diabetes Mellitus. International Journal of Environmental Research and Public Health. Tips Tuesday and The Latest Physiopedia updates.
View at Publisher | View at Google Scholar

 Clinic
Clinic
