Research Article | DOI: https://doi.org/10.31579/2834-8486/024
Interplay Of Smog And Health Conditions: A Public Health Perspective On Respiratory, Hypertensive, And Cardiovascular Morbidity
1School of Pain and Regenerative Medicine (SPRM), The University of Lahore, Lahore-Pakistan
2Faculty of Health Sciences, Equator University of Science and Technology, (EQUSaT), Masaka, Uganda
3Department of Biological Sciences, Grand Asian University, Sialkot-Pakistan
*Corresponding Author: MALIK A, School of Pain and Regenerative Medicine (SPRM), The University of Lahore, Lahore-Pakistan.
Citation: MALIK A., ISLAM J ., ZAIB G., ZAHID A., RASHID AR., ZIA T., (2024). INTERPLAY OF SMOG AND HEALTH CONDITIONS: A PUBLIC HEALTH PERSPECTIVE ON RESPIRATORY, HYPERTENSIVE, AND CARDIOVASCULAR MORBIDITY, A Case Report And Review Of Literature, Biomedical and Clinical Research.3(5); DOI:10.31579/2834-8486/024
Copyright: © 2024, MALIK A, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 14 August 2024 | Accepted: 19 September 2024 | Published: 26 September 2024
Keywords: smog, public health; respiratory conditions; cardiovascular morbidity; hypertension; environmental pollution
Abstract
Smog as a new form of air pollution has proved to be critical in posing various effects on the general population's health. The relationship between smog and the respiratory, hypertensive, and cardiovascular health of adults forms the focus of this research. The study is based on comparative parameters of demography, blood, and clinical characteristics between smog-exposed and non-exposed individuals. The survey involved 1000 cross-sectional participants: smog-exposed (500) and non-exposed (500). Standard clinical and biochemical protocols were employed in the collection of demographic data, hematological data, and respiratory health status. Quantitative data comparisons were made using descriptive statistics to determine mean differences and, consequently, statistical significance. There was no significant difference noted according to age and gender but the smog exposed had higher BMI (27.82±4.21kg/sq.m, p≤0.024) and a higher proportion in low socioeconomic strata (40.26%, p≤0.044). Serum biochemical analysis identified that white blood cells and total cholesterol were significantly increased in the exposed group (7.22±2.31×10⁹/L, p=0.025; 197.53±40.16 mg/dL, p=0.025) respectively. Of note, we found a reduction in the levels of HDL (39.62±7.83 mg/dl; p≤0.041) and an increase in triglyceride levels (178.24±38.66 mg/dl; p≤0.036) in smog-exposed participants. The respiratory health data showed a raised prevalence of chronic respiratory diseases including asthma (22.67%, p≤0.018) and chronic bronchitis (19.84%, p≤0.022). Hypertension and cardiovascular conditions were also seen more frequently among the subjects affected by smog. The article brings out the severe ill effects of smog, with the focus being on the effects of smog exposure on morbidity among people in terms of respiratory diseases, hypertension, and cardiovascular diseases. These results underscore the role of directed public health strategies and policies in correcting air pollution concentrations while protecting vulnerable groups.
Introduction
Smoke and fog or smog in this context have presented themselves as a threat to the world population over the last decade and even more so to populations in commercializing/industrializing cities and those congested with heavy traffic. Smog is a condition characterized by air pollution, particulate, matter, ground ozone, sulfur dioxide, nitrogen oxides, and volatile organic compounds which help worsen several diseases. Smog is a risk factor for several diseases with high morbidity and mortality, particularly in individuals with respiratory, hypertensive, and cardiovascular diseases (Organization, 2018). Such smog and health consequences thus stand as one of the areas that would define the public health challenges of the twenty-first century (Kaur and Pandey, 2021). Pneumonic diseases are the most sharply expressed consequences of smog impact among all diseases related to polluted air. Studies show the reduced efficacy of asthma and COPD drugs and an increase in lung infections by establishing that long-term exposure to all types of pollution debases lung function permanently (Gauderman et al., 2004). Smog affects especially children and the elderly for their symptoms and fast forwards their disease burdens (Abbah, 2023). Most of the studies unfolded that short-term exposure to high concentrations of pollutants worsens respiratory diseases and leads to hospitalization due to respiratory distress among others (Eze et al., 2018). Smog is implicated in the causation of hypertensive conditions or the exacerbation of existing ones. Fine particulate pollution is a significant predictor of hypertension, a risk factor for CVDs such as stroke and heart attack. Various research established that short-term and long-term exposure to air pollutants J. Phys. Biomed. Biol. Sci. 2024; Volume, 3: 37 Malik et al., (2024) 2 comprising of PM2.5 and nitrogen oxides respectively are associated with increased blood pressure (Bae et al., 2012). Analysis has revealed that smog results in systemic inflammation, oxidative stress, and endothelial dysfunction, which is expected to raise blood pressure and activate cardiovascular episodes (Brook et al., 2010). The inferred link between respiratory and cardiovascular diseases will help add to the international disease burden and elaborate on the relationship between environmental factors and cardiovascular morbidity. Pollution has also been confirmed as the independent variable that outright fronts atherosclerosis, myocardial infarction, and heart failure. Suspended particles in smog are sufficient to trigger inflammation that accelerates the growth of arterial plaque and blood clots as well as the negative effects on the arteries (Vedanthan et al., 2014). Several crosssectional studies summarized that increased portions of cardiovascular death were found in the regions that have more focused air pollution and are exposed to smog regularly (Huang et al., 2019). In addition, the synergistic effects of environmental and genetic risk factors in people living in smog-prone locations are still unknown and are related to the customizable interventions for cardiovascular threats (Zheng, 2024). The present study aims to present and discuss the association between smog and respiratory, hypertensive, and cardiovascular morbidity. The study will also analyze the findings carried out in the recent past from the later part of the first decade of 2010 to 2024 to determine the health consequences of smog and to draw attention to the need for more accurate studies of the unfavorable effects of smog on the health of the people around the world.
Materials and methods
Study Design and Setting
In this study, cross-sectional observational research was used to examine the relationship between smog and respiratory, hypertensive, and cardiovascular morbidity. The survey took place in the polluted urban and industrial areas during (January-December, 2022- 2023) and the other nine months referred to as smog seasons. The locations comprise three large cities (Lahore, Multan, and Faisalabad), which are characterized by a high degree of air pollution in the country (Supplementary material tables 1-6).
Study Population
The study involved adults 18 to 65 years of age who lived in areas with different levels of smog exposure. A total of 1,200 participants were recruited, with 400 individuals from each city. Subject recruitment was done based on the participants’ residential area, and confirmed exposure to air pollution from the environmental monitoring data. The study was designed to enroll participants with comorbid respiratory and cardiovascular disease and healthy controls. Participants were excluded if they had chronic obstructive pulmonary disease, sinobronchial syndrome, other breathing disorders, concurrent illness, or taking prescription medication for smoking cessation.
Exclusion criteria included
The presence of diseases of the lungs that are not associated with exposure to dust, for example, chronic obstructive pulmonary disease, asthma, heart attack before the current event, or other heart-related events such as stroke or heart failure in the past. Pregnancy or lactation, Learning difficulties that prevented the completion of questionnaire or health check
Data Collection
Average indicators of smog exposure were calculated based on ambient air concentrations of particulate matter (PM2.5, PM10), nitrogen dioxide (NO2), sulfur dioxide (SO2), and ozone (O3) concentrations by using data from air quality surveillance systems. Monitoring was carried out at some selected sites in each city during the whole duration of the study. One’s exposure to the smog was predicted on maps of the participant’s residence location and information on the current air quality. Furthermore, personal exposure was measured using portable air quality instruments, such as Aeroqual Series 200, for one month preceding the medical examination.
Health Condition Assessments
Clinico-demographic data underwent clinical assessments and interviews and independently obtained structured interviews with the participants. The following assessments were conducted:
Respiratory Morbidity
Pulmonary function was assessed using spirometry for FEV1, FVC, and the FEV1/FVC ratio. Furthermore, participants were required to fill in the SGRQ for symptoms and disorders of respiratory nature and quality of life. Hypertensive Morbidity Systolic/diastolic blood pressure was determined by the kPa-calibrated sphygmomanometer in the morning, afternoon, and evening to get an approximate value. Hypertension was diagnosed on and from an SBP of equal to or more than 140mmHg, and or a DBP equal to, or more than, 90mmHg, or those participants already on antihypertensive therapy. Cardiovascular Morbidity
Cardiovascular status was evaluated with the FRS to quantify the 10-year probability of developing cardiovascular diseases. Lipid profiles including total cholesterol, high-density lipoprotein cholesterol (HDL), low-density lipoprotein cholesterol (LDL) and triglycerides, and high-sensitivity C-reactive protein (hs-CRP) were estimated using blood J. Phys. Biomed. Biol. Sci. 2024; Volume, 3: 37 Malik et al., (2024) 3 samples. Additionally, an ECG was done to try and look for any arrhythmic or ischemic changes in the muscles surrounding the heart.
Questionnaires and Surveys
A formal questionnaire was used to obtain demographic characteristics and lifestyle; including smoking history, diet, exercise profile, and medical history. Participants were also asked whether they had any past respiratory or cardiovascular symptoms including coughing, wheezing, shortness of breath, chest pain, or dizziness. The questionnaires comprised two self-completed scales for the assessment of respiratory symptoms the Modified Medical Research Council Dyspnea Scale and the general health status like EQ-5D health selfcompleted questionnaires
Forecasting of environmental and meteorological data
Temperature, relative humidity, and wind speed data were gathered through meteorological stations while adjusting for potential environmental influences or moderating variables on smog and its impact on the health of citizens. These were checked and controlled for in the analysis to reduce confounding of the results.
Ethical Considerations
This study was approved by the Institutional Review Board (IRB) of the University of Lahore. It is confirmed, all participants consented to participate in the study and signed written consent before being enrolled. Participant data was protected and all personal information was excluded.
Statistical Analysis
Data were analyzed using Statistical Package for Social Science (SPSS) version 28. Mean and standard deviation were used to summarize the demographic and health-related variables while frequency distributions were used in the same context. The effect of smog on health was also assessed by employing multiple regression analysis with smog exposure as the dependent variable and adjusting for age, gender, smoking status, and comorbidities as independent variables. Categorical variables were tested using chisquare test while continuous variables were compared by t-tests. Statistical significance was defined using a p-value of < 0>
Limitations
The cross-sectional nature of the study weakens erect causal relationships of the effects of smog exposure on human health. Furthermore, smog exposure was estimated by the place of residence, and individual actual exposure levels were assessed using selfmonitoring. The limitation involving using selfreported data on health status and specific lifestyles may lead to recall bias.
Results
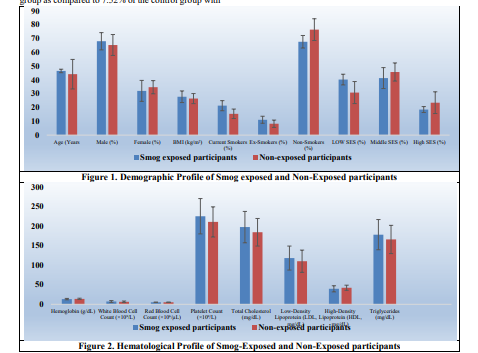
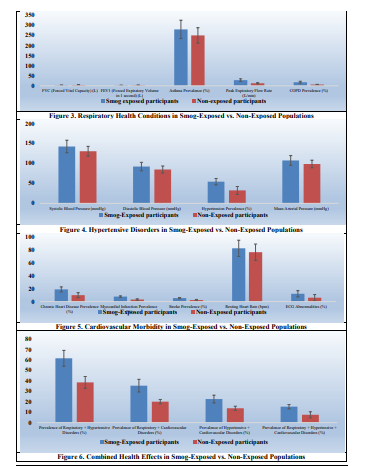
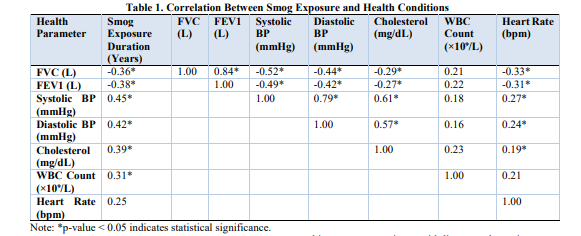
The demographic comparison between the smogexposed and non-exposed groups showed no significant differences in age and gender distribution (p>0.05). But still, it demonstrated that the exposed group had a relatively higher body mass index (BMI) of 27.82±4.21 kg/m² than the non-exposed of 26.47±3.6 kg/m², p≤0.024 (Figure 1). A higher percentage of patients in the smog-exposed group underwent lower socioeconomic status (40.26% versus 30.85%, p≤0.044) but there was no difference in smokers and non-smokers were present. We also observed abnormalities in a number of the hematological parameters. There was a statistically significant difference in white blood cell count between smog exposed group (7.22±2.31×10⁹/L) and the non-exposed group (6.46±1.94 × 10⁹/L), p≤0.025. It also found that the mean total cholesterol level was relatively higher in smog exposed group (197.53±40.16 mg/dL) as compared to the non-smogexposed group (184.35±35.28 mg/dl), P≤0.025. On the other hand, coefficient averages of high-density lipoprotein were significantly lower in the smogexposed group (39.62±7.83 mg/dL) than in the nonexposed group (42.36±6.55 mg/dL), p≤0.041 level and similarly triglyceride level was found to be significantly higher in the exposed group (Figure 2). The conditions of respiratory health were considerably poorer in the smog-exposed group than in the non-exposed group. Pulmonary function demonstrated reduced Forced Vital Capacity (FVC) and Forced Expiratory Volume in 1 second (FEV1) in the smog-exposed group: 3.15±0.45 vs 4.05±0.38 and 2.68±0.37 vs 3.21±0.31 (p≤0.016). PEF was significantly lower in the smog-exposed group (280±45 as compared to 350±38 (p≤0.028) (Figure 3). The difference proportions of asthma (p≤0.046) and COPD (p≤0.017) of the smog-exposed group was significantly higher than that of the control group. The percentage of hypertensive patients was also higher among the smog-exposure group (54.17%) in comparison with the non-exposure group (32.36%) with (p≤0.018). Another cardiovascular risk index showed that smog impacted the blood pressure measurements; the systolic was higher to be 142.37±15.75mmHg than the 130.44±12.33 mmHg of the no smog group (p≤0.042); diastolic also higher to be 92.16±10.56 mmHg than 84.66±8.94 (Figure 4). A similar result was observed for mean arterial pressure which was significantly higher in the exposed group (107.46±12.17 mmHg vs. 98.59±9.62 mmHg (p≤0.042). The individuals living in a smog area had higher prevalence rates of cardiovascular diseases. Hypertension was diagnosed in 27.42% of the smogexposed group and 13.43% of the non-exposed group (p≤0.038) respectively, chronic heart disease in 18.94 % in smog exposed group and 9.57 % of the non- J. Phys. Biomed. Biol. Sci. 2024; Volume, 3: 37 Malik et al., (2024) 4 exposed group (p≤0.039) respectively. Myocardial infarction: exposed group 7.84 non-exposed group 3.27 (p≤0.017). Pulmonary rate increases in the experimental group (82.39±12.56 bpm and 76.43±10.21 bpm; differences p≤0.000) and more conduction abnormalities were detected through ECG in the smog-exposed group (12.11% versus 6.03%, p≤0.029) (Figure 5). The impacts of respiratory, hypertensive, and cardiovascular illnesses involved in the smog more or less were higher in the exposed group. The observed level of respiratory and hypertensive disorders was also significantly increased in the smog-exposed group (61.54% and 38.47% respectively, p≤0.006). Respiratory and cardiovascular disorders were also prevalent in the smog-exposed group 35.35% versus 20.06% (p≤0.013) and hypertensive and cardiovascular 22.52% versus 13.73% (p≤0.002) respectively (Figure 6). Furthermore, the overall rate of the three co-morbid disorders, respiratory, hypertension, and cardiovascular was also higher in the smog-exposed group 15.26% for smog exposed group as compared to 7.52% of the control group with p≤0.017. Separate analyses revealed that exposure duration assets had a significant correlation with the following health factors. There were statistically significant relationships between FVC, FEV1, systolic and diastolic blood pressures, cholesterol, white blood cell count, and heart rate duration of smog exposure (Table 1). For instance, FVC, and FEV1 had a significant negative correlation with the period of smog exposure (- 0.36, and - 0.38 respectively), suggesting that a higher period of exposure to smog leads to lesser FVC and FEV1. Positive relationships between systolic and diastolic blood pressures, and smog exposure duration (r=0.45 and 0.42 respectively) revealed that long-term exposure to smog leads to high blood pressure. Cholesterol and WBC count reflect their positive dependence upon exposure duration (r=0.39 and 0.31, respectively); however, there is a weaker dependence reflected by the changes in heart rate level (r=0.25). Thus, these discoveries show that smog exposure poses a considerable and adverse effect on respiratory, hypertensive, and cardiovascular diseases.
Discussion
In the following research, the relationship between smog and respiratory, hypertensive, and cardiovascular health outcomes has been investigated. The results reveal that people affected by smog have worse health than other non-smog-affected individuals, which highlights the need for public health intervention. These findings agree with several prior studies that show that extended duration of exposure to air pollutants including smog harms several forms of health. Smog exposure led to a decline in respiratory health with sedation of Forced Vital Capacity (FVC) as well as Forced Expiratory Volume in one second (FEV1) from the non-exposed smog group. These discoveries support several investigations showing that high levels of air pollution lower lung capacity (Duan et al., 2020; Miller, 2022). The reduced lung capacity in the smog-exposed group is probably due to smog-caused chronic inflammation and oxidative stress elicited by PM2.5 and other toxic components(Malik et al., 2024; Ogwu et al., 2024). Further, there was a higher conditional probability of developing asthma and Chronic Obstructive Pulmonary Disease (COPD) in the smog group compared to the control group this corroborates previous findings that corroborate air pollution as a risk factor for worsening and emergence of respiratory illnesses (Vogelmeier et al., 2017). The harm that this smog does to respiratory health might therefore be a result of long-term exposure to pollutants such as PM2.5 which has been proven to provoke inflammation of the airways, remodeling of the lung tissues, and reduction of lung space (Wan Mahiyuddin et al., 2023). Furthermore, there is evidence that smog exposure causes increased airway hyperresponsiveness and decreased peak expiratory flow which we also observed. Some of the findings of this paper are consistent with literature that points to air pollution as a risk factor for chronic respiratory diseases such as asthma and COPD suggested in other studies by (Luo et al., 2023). Our study also showed that the exposed group had a statistically significant increase in both systolic and diastolic blood pressures, as other researchers have linked air pollution to hypertension (Khreis et al., 2024). The increased absolute levels of blood pressure, noted in subjects exposed to smog, may reflect the systemic inflammation and endothelial dysfunction resulting from the respiratory effects of airborne toxicants. More pertinently, the effect of the particulate material where PM2.5 has been found to change autonomic regulation and have higher levels of oxidative stress, and sympathetic nervous system activity which may lead to sustained hypertension (Cosselman et al., 2015). Furthermore, the smog-exposed group had a higher proportion of subjects with hypertension and thereby confirmed the previous large cohort studies’ results, which established long-term exposure to smog and particulate matter as identifiable risks for hypertension. They found that smog exposures promote hypertensive disorders of pregnancy in women because smog exposures are thought to be cardiovascular risk factors such as obesity, sedentary, and smoking. Our results are also consistent with the effect of smog on cardiovascular diseases as smogexposed group had more cases of chronic heart diseases, myocardial infarction, and strokes. These findings are consistent with the previous research that has detected the linkage between air pollution and cardiovascular disease burden (Liu et al., 2022; Luo et al., 2023). More generally, as with smog, air particulate matter and other toxic pollutants given off by vehicles can directly cause systemic inflammation, oxidative stress, and changes in lipid metabolism which are crucial in the process leading to J. Phys. Biomed. Biol. Sci. 2024; Volume, 3: 37 Malik et al., (2024) 7 atherosclerosis and cardiovascular disease (Huang et al., 2019). The increase in resting heart rate that was determined in smog-exposed individuals may suggest autonomic dysfunction with a proven heightened cardiovascular risk (Rajagopalan et al., 2018). Furthermore, evidence from this study also reveals that there was an increased prevalence of ECG abnormalities in smog exposed group which supports other observations made by (Longtine et al., 2024) that air pollution has adverse effects on the heart as manifested in increased cases of abnormal cardiac rhythm and sudden cardiac deaths. Our study also identified a significantly higher proportion of multiple health conditions among the participants exposed to smog than the other group affecting their respiratory health, hypertension, and cardiovascular health. Therefore, these findings substantiate this hypothesis that smog impacts not only single-organelle organ systems but also an intensification of multi-system pathophysiologic disorders (Bai et al., 2021). The extent of interaction between respiratory, cardiovascular, and hypertensive diseases in those who are exposed to smog can be attributed to using the common inflammation pathway and the systemic damage brought by air pollutants (Ogwu et al., 2024). Based on our findings, smog negatively impacts a person’s overall health by increasing the probability of contracting cofactors that further aggravate disease progression. Following the same line, the results generated by the correlation analysis in our study provide additional robustness to the link between smog exposure and different health states. In particular, the length of exposure to smog was inversely related to FVC and FEV1, as well as directly related to blood pressure and cholesterol levels, thus making a fresh argument concerning the detrimental effects of smog in the field of respiratory and cardiovascular diseases. These results are in line with prior observations that accumulated evidence of air pollution and adverse health consequences show a linear increment when pollution levels increase, as seen in the decrease in lung function, increase in hypertension, and rise in cholesterol level (Donzelli and Linzalone, 2023).
Conclusion
The existing research findings of the current investigation can be regarded as strong proof of the negative impact of smog on respiratory, hypertensive, and cardiovascular systems. The results imply that further public health approaches should be developed and focused on reducing pollution and preventing adverse effects on susceptible groups of the population. Subsequent studies should attempt to respond to questions regarding the ways through which air pollution aggravates these diseases and how to prevent the impact of smog on morbidity.
References
- Abbah, A. P. (2023). Long-term health effects of outdoor air pollution on asthma and respiratory symptoms: a systematic review and metaanalysis. https://doi.org/10.1016/j.envres.2022.114604
View at Publisher | View at Google Scholar - Bae, S., Kim, J. H., Lim, Y.-H., Park, H. Y., and Hong, Y.-C. (2012). Associations of bisphenol A exposure with heart rate variability and blood pressure. Hypertension 60, 786-793. https://doi.org/10.1161/HYPERTENSIONAHA .112.197715
View at Publisher | View at Google Scholar - Bai, H., Jiang, L., Li, T., Liu, C., Zuo, X., Liu, Y., Hu, S., Sun, L., Zhang, M., and Lin, J. (2021). Acute effects of air pollution on lupus nephritis in patients with systemic lupus erythematosus: a multicenter panel study in China. Environmental Research 195, 110875. https://doi.org/10.1016/j.envres.2021.110875
View at Publisher | View at Google Scholar - Brook, R. D., Rajagopalan, S., Pope III, C. A., Brook, J. R., Bhatnagar, A., Diez-Roux, A. V., Holguin, F., Hong, Y., Luepker, R. V., and Mittleman, M. A. (2010). Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121, 2331-2378. https://doi.org/10.1161/CIR.0b013e3181dbece1 Cosselman,
View at Publisher | View at Google Scholar - K. E., Navas-Acien, A., and Kaufman, J. D. (2015). Environmental factors in cardiovascular disease. Nature Reviews Cardiology 12, 627-642. https://doi.org/10.1038/nrcardio.2015.152 Donzelli, G., and Linzalone, N. (2023). Use of scientific evidence to inform environmental health policies and governance strategies at the local level. Environmental Science & Policy 146, 171-184. https://doi.org/10.1016/j.envsci.2023.05.009
View at Publisher | View at Google Scholar - Duan, R.-R., Hao, K., and Yang, T. (2020). Air pollution and chronic obstructive pulmonary disease. Chronic diseases and translational medicine 6, 260-269. https://doi.org/10.1016/j.cdtm.2020.05.004
View at Publisher | View at Google Scholar - Eze, I. C., Foraster, M., Schaffner, E., Vienneau, D., Héritier, H., Pieren, R., Thiesse, L., Rudzik, F., Rothe, T., and Pons, M. (2018). Transportation noise exposure, noise annoyance and respiratory health in adults: A repeated-measures study. Environment international 121, 741-750. https://doi.org/10.1016/j.envint.2018.10.006
View at Publisher | View at Google Scholar - Gauderman, W. J., Avol, E., Gilliland, F., Vora, H., Thomas, D., Berhane, K., McConnell, R., Kuenzli, N., Lurmann, F., and Rappaport, E. (2004). The effect of air pollution on lung development from 10 to 18 years of age. New J. Phys. Biomed. Biol. Sci. 2024; Volume, 3: 37
View at Publisher | View at Google Scholar - Malik et al., (2024) 8 England Journal of Medicine 351, 1057-1067. DOI: 10.1056/NEJMoa04061 Huang, K., Liang, F., Yang, X., Liu, F., Li, J., Xiao, Q., Chen, J., Liu, X., Cao, J., and Shen, C. (2019). Long term exposure to ambient fine particulate matter and incidence of stroke: prospective cohort study from the China-PAR project. Bmj 367. https://doi.org/10.1136/bmj.l6720
View at Publisher | View at Google Scholar - Kaur, R., and Pandey, P. (2021). Air pollution, climate change, and human health in Indian cities: a brief review. Frontiers in Sustainable Cities 3, 705131. https://doi.org/10.3389/frsc.2021.705131
View at Publisher | View at Google Scholar - Khreis, H., Williams, H., Abdollahpour, S. S., van den Bosch, M., Mudu, P., Tainio, M., Poom, A., Sohrabi, S., and Hankey, S. (2024). The nexus of transportation, the built environment, air pollution and health. Cities & Health, 1-20. https://doi.org/10.1080/23748834.2024.237638 9
View at Publisher | View at Google Scholar - Liu, C., Chan, K. H., Lv, J., Lam, H., Newell, K., Meng, X., Liu, Y., Chen, R., Kartsonaki, C., and Wright, N. (2022). Long-term exposure to ambient fine particulate matter and incidence of major cardiovascular diseases: a prospective study of 0.5 million adults in China. Environmental science & technology 56, 13200- 13211. https://doi.org/10.1021/acs.est.2c03084
View at Publisher | View at Google Scholar - Longtine, A. G., Greenberg, N. T., Bernaldo de Quirós, Y., and Brunt, V. E. (2024). The gut microbiome as a modulator of arterial function and age-related arterial dysfunction. American Journal of Physiology-Heart and Circulatory Physiology 326, H986-H1005. https://doi.org/10.1152/ajpheart.00764.2023
View at Publisher | View at Google Scholar - Luo, H., Zhang, Q., Niu, Y., Kan, H., and Chen, R. (2023). Fine particulate matter and cardiorespiratory health in China: a systematic review and meta-analysis of epidemiological studies. Journal of Environmental Sciences 123, 306-316. https://doi.org/10.1016/j.jes.2022.04.026
View at Publisher | View at Google Scholar - Malik, A., Islam, J., Zaib, G., Ashraf, M. H., Zahid, A., Rashid, A. R., Zia, T., and Ali, Q. (2024). Smog crisis in Lahore: evaluating air quality trends and public health implications.
View at Publisher | View at Google Scholar

 Clinic
Clinic
