Research Article | DOI: https://doi.org/10.31579/2835-835X/117
Cystadenoma of the Seminal Vesicle Review and Update
North Manchester General Hospital; Department of Urology, Manchester, M8 5RB. United Kingdom.
*Corresponding Author: Anthony Kodzo-Grey Venyo., North Manchester General Hospital; Department of Urology, Manchester, M8 5RB. United Kingdom.
Citation: Grey Venyo AK, (2025), Cystadenoma of the Seminal Vesicle Review and Update, Clinical Trials and Case Studies, 4(6); DOI:10.31579/2835-835X/117
Copyright: © 2025, Anthony Kodzo-Grey Venyo. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 24 November 2025 | Accepted: 08 December 2025 | Published: 19 December 2025
Keywords: cystadenoma of seminal vesicle; seminal vesicle cystadenoma; asymptomatic; incidental; lower urinary tract symptoms; histopathology; immunohistochemistry; benign tumour; surgical excision; good prognosis; rare; recurrence; alive.
Abstract
Cystadenomas of the seminal vesicles are benign cystic tumours, which had been classified into the group of mixed epithelial-stromal tumours (MEST). Primary tumours which afflict the seminal vesicles are quite rare, and benign tumours afflicting the seminal vesicles are rarer than malignant ones, with only a few cases reported in the English literature since 1944. Cystadenomas of the seminal vesicles do constitute a potential diagnostic pitfall, due to the fact that they could be clinically confused with malignant neoplasms and histologically with non-neoplastic inflammatory lesions or other cystic tumours, even malignant tumours. Cystadenoma of seminal vesicle is a very rare benign tumour which has been reported sporadically. Cystadenoma of seminal vesicle may be identified incidentally based upon radiology imaging of some asymptomatic individuals who have undergone radiology imaging for a different reason. Cystadenoma of seminal vesicle may manifest with non-specific symptoms including: lower urinary tract symptoms; urinary retention; haematuria; haematospermia; and infertility. In majority of cases of cystadenoma of seminal vesicle, the serum PSA level had tended to be low or normal; but on rare occasions serum PSA levels of some individuals afflicted by cystadenoma of seminal vesicle the serum PSA level had been reported as elevated. Cystadenoma of seminal vesicle has most often tended to be unilateral but bilateral cystadenoma of the seminal vesicle has been reported occasionally.
Effective treatment of cystadenoma of seminal vesicle could be either open seminal vesicle surgical excision or laparoscopic surgical excision of the seminal vesicle containing the tumour. Cystadenoma of seminal vesicle may prove difficult to differentiate from simulants of cystadenoma of the seminal vesicle that are more common lesions including: adenocarcinoma of seminal vesicle, seminal vesicle cyst and mixed epithelial and stromal tumours of the seminal vesicle.
Introduction
It has been iterated that cystadenomas of the seminal vesicles are benign cystic tumours, which currently has been classified into the group of mixed epithelial-stromal tumours (MEST). [1] It had also been documented that primary tumours that arise within the seminal vesicles are quite uncommon, benign tumours which are less common in comparison with malignant tumours of the seminal vesicles, with only a few cases reported in the English literature since 1944. [1] It has additionally been iterated that cystadenomas represent a potential diagnostic pitfall, as they could be clinically confused with malignant neoplasms and histologically with non-neoplastic inflammatory lesions or other cystic tumours, even malignant. In view of the aforementioned recent iterations, the ensuing article on cystadenoma of the seminal vesicles has been written and divided into two parts: (A) Overview of cystadenoma of seminal vesicles and (B) Miscellaneous Narrations and Discussions from some case reports, case series and studies related to cystadenoma of seminal vesicles.
Aim
To review and update the literature on cystadenoma of the seminal vesicles.
Methods
Internet data bases were searched including: Google; Google Scholar; Yahoo and PUBMED. The search words that were used included: cystadenoma of seminal vesicle; seminal vesicle cystadenoma. Twenty -seven (27) references were identified which were used to write the article which has been divided into two parts: (A) Overview of cystadenoma of seminal vesicles and (B) Miscellaneous Narrations and Discussions from some case reports, case series and studies related to cystadenoma of seminal vesicles.
Results
[A] Overview
Definition / general statement [2]
• It has been iterated that cystadenoma of seminal vesicle is a rare, benign epithelial tumour which is composed of variably sized cysts that are lined by bland cuboidal cells [2]
Essential features
The essential features of cystadenoma of the seminal vesicle, has been summated as follows: [2]
• Cystadenoma of the seminal vesicle, is differentiated from mixed epithelial and stromal tumour of the seminal vesicle by demonstration upon microscopy examination of the seminal vesicle lesion the absence of stromal hypercellularity
• Cystadenoma of the seminal vesicle, should be differentiated from prostatic stromal tumour of uncertain malignant potential entrapping glands
o Factors that favour seminal vesicle cystadenoma diagnosis had been documented to include the ensuing:
Cystic tumour that is centred within the seminal vesicle
Presence of no immunohistochemistry staining expression of prostatic differentiation markers
Terminology
• It has been iterated that with regard to terminology, some authors consider cystadenoma of the seminal vesicle, as the expression of lowest grade (benign) of mixed epithelial and stromal tumour of the seminal vesicle [2] [3]
Epidemiology [2]
• With regard to epidemiology, it has been iterated that cystadenoma of the seminal vesicle, is rare and that less than thirty (< 30>
• It has been documented that there has been a wide age distribution of cystadenoma of the seminal vesicle, and this has ranged from 23 years to 66 years of age.
Sites
• With regard to the site of cystadenoma of the seminal vesicle, it has been iterated that cystadenoma of the seminal vesicle has tended to be centred within the seminal vesicles [2]
Pathophysiology
• It has been iterated that the pathophysiology of cystadenoma of the seminal vesicle, is not known [2]
Aetiology
• It has been iterated that the aetiology of cystadenoma of the seminal vesicle, is not known [2]
Clinical features
It has been iterated that the clinical features of cystadenoma of the seminal vesicle, include the following: [2]
• Obstructive urinary tract symptoms
• Some patients had manifested with an asymptomatic mass or the masses were incidentally identified within radiology imaging studies
Diagnosis
• With regard to the diagnosis, it has been iterated that cystadenoma of the seminal vesicle, is visualised as cystic or solid and cystic masses that tend to be detected within undertaken radiology imaging studies. [2]
Radiology description
With regard to the radiology imaging description of cystadenoma of the seminal vesicles, it has been stated that radiology imaging studies do demonstrate the following: [2]
• Cystic or solid and cystic masses that are centred within the seminal vesicles
Prognostic factors
With regard to the factors of prognostication, it has been iterated that: [2]
• Cystadenoma of the seminal vesicle is a benign neoplasm and local resection of the seminal vesicle tumoral lesion is regarded as curative treatment.
Treatment
• Surgical resection has been stated to be the treatment for cystadenoma of seminal vesicle [2]
Microscopic (histologic) description
The microscopy pathology examination features of cystadenoma of the seminal vesicle had been summated as follows: [2]
• Microscopy pathology examination of specimens of the seminal vesicle lesion demonstrates glandular spaces of varying sizes that are lined by cuboidal cells without atypia [3]
• Microscopy pathology examination of specimens of the seminal vesicle lesion demonstrates lobular pattern, forming branching lumina and cysts that contain granular intraluminal secretions [2]
• Microscopy pathology examination of specimens of the seminal vesicle lesion demonstrates no hypercellularity or atypia within the stromal cells [2]
Immunohistochemistry staining studies
Positive stains
It has been iterated that immunohistochemistry staining studies of specimens of the seminal vesicle lesion demonstrates positive staining for the following features: [2]
• The epithelial lining stains positively for pancytokeratin and CK7
• Basal cells of cystadenoma of seminal vesicle exhibit positive expression for high molecular weight keratins.
• Stromal cells of cystadenoma of seminal vesicle may exhibit positive staining for smooth muscle actin.
• Normal epithelial lining of a seminal vesicle usually strongly expresses GATA3; nevertheless, this tumour marker is also positive within the prostate gland and should be interpreted with caution [4]
• Normal and neoplastic seminal vesicle epithelium tends to be strongly positive for PAX8 [5] [6]
Negative stains
It has been iterated that immunohistochemistry staining studies of specimens of the seminal vesicle lesion demonstrates negative staining the following features: [2]
• Epithelial cells usually do not express PSA, prostein / P501S or calretinin
• Stromal cells are negative for S100
Differential diagnoses
The differential diagnoses of cystadenoma of seminal vesicle had been summated to include the ensuing: [2]
• Mixed epithelial and stromal tumour of the seminal vesicle:
o Stromal hypercellularity
• Prostatic stromal tumour of uncertain malignant potential entrapping glands:
o Centred in the prostate, entrapped prostatic glands express PSA and other markers of prostatic differentiation
• Adenomatoid tumour of seminal vesicle:
o Expresses mesothelial markers such as calretinin
• Mesothelial cysts:
o Express mesothelial markers such as calretinin
• Cystic ductal adenocarcinoma of the prostate gland:
o Pseudostratified and atypical epithelial neoplastic cells
• Primary seminal vesicle carcinoma:
o Atypical cells
o The tumour centred within the seminal vesicle
o Adenocarcinomas usually show papillary glandular and trabecular growth patterns
• Exclusion of other primary sites and immunophenotype excluding primary prostate adenocarcinoma [7]
[B] Miscellaneous Narrations and Discussions from some case reports, case series and studies related to cystadenoma of seminal vesicle:
Argun et al. [8] stated the following:
• Cystadenoma is an extremely rare benign tumour of the seminal vesicle.
• Diagnosis of these cystadenoma tumours of the seminal vesicle and the differential diagnosis from malignant ones may be challenging in view of the fact that most of the time symptoms do not occur.
• Management of these cystadenoma of seminal vesicle tumours has remained debatable in view of the limited data in the literature.
• They had presented the first robot-assisted laparoscopic excision of a cystadenoma of the seminal vesicle.
Argun et al. [8] reported a-48-year-old man, who had manifested with diminished ejaculate volume and a 3.5 cm right seminal vesicle mass, which had increased its size at 6 cm after the 3-month period. He underwent trans-rectal ultrasound scan-guided biopsy of the lesion and pathology examination of the biopsy specimen revealed no malignancy. Robot-assisted laparoscopic excision of the tumour was undertaken. Port placement was the same as robot-assisted radical prostatectomy. The operative time and estimated blood loss were 240 minutes and 200 mL, respectively. The patient was discharged on post-operative day 3 without any complications. Final histopathologic examination of the excised lesion demonstrated. cystadenoma of the seminal vesicle. Argun et al. [8] made the ensuing conclusions:
• Surgical intervention might be considered when a cystadenoma of the seminal vesicle is diagnosed and symptoms or tumour growth does occur.
• Robot-assisted laparoscopic excision is an alternative treatment option in the management of these rare tumours.
Ameli and Yousefzadeh [9] reported a-49 years old man, who presented with complain of urinary frequency over the preceding 5 months. He also stated that he had dysuria, mild obstructive urinary symptoms and constipation, which had a gradual onset, initiating 6 months preceding his attendance at the clinic. He did not have any other urinary symptoms, haematuria, flank pain or weight loss. He did not have any significant past medical and surgical history. During his clinical examination, all his organ systems were noted to be normal except for the finding of a huge prostate gland, that was palpable during his digital rectal examination which was rubbery and symmetrical. The results of his renal function tests, serum prostate specific antigen (PSA) level and ultrasound scan of his kidneys and prostate were within normal ranges except for his serum PSA which was 11.2. Furthermore, upon ultrasound scanning of his prostate gland it was reported that the prostate gland was enlarged prostate with volume of 560ml with multiple cystic area inside it. His post void residual urine volume was zero. He had a computed tomography (CT) scan and abdomen and pelvic magnetic resonance imaging (MRI) scan with and without gadolinium and huge (120 * 100 * 100mm) heterogeneous mass in anatomic site of prostate gland was reported (see figure 1). The mass visualised with solid and cystic component, it was well-circumscribed and had contained partially thick peripheral capsular. There was no adjacent structure involvement. Patient underwent pelvic mass resection by retro vesical abdominal approach. The mass was noted to have elongation beside prostatic urethra. Frozen section examination of the specimen of the mass had demonstrated that the mass was benign in nature, 70% of the mass was freed from the adjacent structures. In view of its extension near the prostatic urethra and risk of external sphincter injury or neurovascular bundle injury, the capsule of the mass which was elongated near prostatic urethra, was spared but enucleated within its inside aspect (see figure 2). Following his recovery from surgery patient was noted to be symptom free and totally continent with preserved erectile function. The final pathology examination of the mass was reported to have demonstrated features that had been adjudged to be consistent with cystadenoma/epithelial stromal tumour of the seminal vesicle with no features suggestive of malignancy.
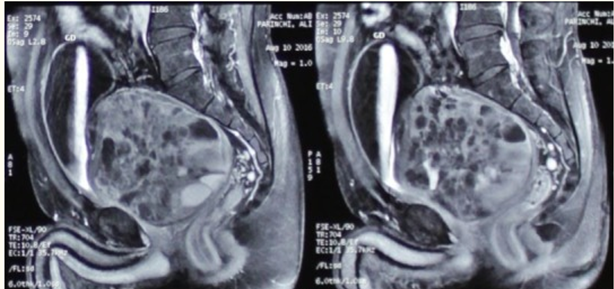
Figure 1: MRI of abdominopelvic. Reproduced from: [9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5847134/ Under the Creative Commons Attribution License. Under Copyright: under copyright: Droit d'auteur © Mojtaba Ameli et al. The Pan African Medical Journal - ISSN 1937-8688. This is an Open Access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Figure 2: An overview of the mass. - Reproduced from: [9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5847134/ Under the Creative Commons Attribution License. Under Copyright: under copyright: Droit d'auteur © Mojtaba Ameli et al. The Pan African Medical Journal - ISSN 1937-8688. This is an Open Access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Ameli and Yousefzadeh [9] made the ensuing discussions:
• Primary diseases of the Seminal Vesicles are very rare.
• Benign tumours could appear as complex, solid cystic retro vesical masses and had often tended to be totally asymptomatic.
• Nevertheless, they could also lead to the development of lower urinary tract symptoms (LUTS) and non-specific signs, such as visible haematuria, haematospermia, perineal or postcoital discomfort and painful defecation.
• On rare occasions, infertility would be the main manifestation [10]
• It had been iterated that cystadenoma of the seminal vesicle is an extremely rare benign tumour with only 15 cases reported by the time of the report of their article in the English literature. [8].
• Cystadenomas of the Seminal vesicle typically occurs in middle-aged man and had almost all the time never been bilateral and its diagnosis had typically been made upon final pathology examination of the specimen pursuant to surgical resection.
• Surgical approach to the Seminal vesicles does depend mainly on the expertise and comfort of the surgeon, even though the characteristics of the lesion might have an impact upon the decision regarding the approach.
• The anterior surgical approach had been well established and is a good open approach for patients who have large benign masses or cysts.
• It had been iterated that trans vesical, per vesical or retro vesical approach could be considered. [11]
• In other reports of cystadenoma of the seminal vesicle, serum PSA levels were normal [10] [12], but in their reported case the patient’s serum PSA level was 11 and hence the diagnosis was very difficult because the huge mass was at the prostatic anatomic and prostatic cancer was in differential diagnosis.
• But after the surgery the serum PSA level was normal and had not risen again.
• In this respect their reported case was absolutely unique. The tumour was resected utilising an open trans vesical approach which enabled full exposure of the seminal vesicle without damaging the nerves and blood supply of the urinary bladder which is also routinely undertaken by another surgeon [13] [14]
• In view of the rarity of cystadenomas of the seminal vesicles, no standard surgical approach could be concluded but in the literature this surgery had been undertaken done with laparoscopy and robot assisted laparoscopy [8] [10]
Ameli and Yousefzadeh [9] concluded that:
Surgical intervention might be considered when a cystadenoma of the seminal vesicle is diagnosed and the symptoms or tumour growth occurs trans-vesical removal of seminal vesicle mass is an effective surgical procedure for seminal vesicle disease.
Baschinsky et al. [15] stated the following:
• Primary tumours of the seminal vesicle are rare; and most of the reported cases of primary tumours of the seminal vesicle are carcinomas, with occasional reports of primary seminal vesicle sarcoma and an uncommon group of mixed epithelial-stromal tumours.
• The latter had been variably reported in the literature as cystadenoma, phyllodes tumour, and mullerian adenosarcoma-like tumour.
Baschinsky et al. [15] reported a 37-year-old man, who had manifested with symptoms of urinary bladder outlet obstruction and who was found to have a pelvic mass. Resection of the mass had yielded a biphasic tumour which was typified by cystically dilated glandular spaces admixed with spindle-shaped stromal cells. There was no significant cytologic atypia or mitotic activity. The histological features of the specimen were adjudged to be most consistent with the reported cases of cystadenoma. The patient was alive, with no evidence of disease, 6 months after undergoing his surgery.
Baschinsky et al. [15] concluded that:
• Their reported case had added to the gradually growing body of literature on mixed epithelial-stromal tumours of the seminal vesicle.
Santos et al. [16] stated the following:
• Cystadenomas of the seminal vesicles are extremely rare benign tumours.
• They had not been able to find more than 10 cases in the literature.
Santos et al. [16] reported a benign cystadenoma of the seminal vesicle in a 49-year-old man.
Lee et al. [17] stated the following:
• Primary tumours of the seminal vesicle are quite rare with most reported cases being carcinomas.
• Nevertheless’ benign tumours of the seminal vesicle are extremely rare.
Lee et al. [17] reported a case of a cystadenomas of the seminal vesicles in a 46-year-old asymptomatic man, that was identified incidentally by computed tomography scan
Chen et al. [18] evaluated the clinical presentation pathological characteristics, diagnosis and treatment of cystadenoma of the seminal vesicle. Chen et al. [18] analysed one case of cystadenoma of the seminal vesicle as well as reviewed the relevant literature of cystadenoma of seminal vesicle. Chen et al. [18] summated the results as follows:
• The patient had undergone surgical removal of the right seminal vesicle together with the tumour, that was pathologically confirmed to be cystadenoma of the seminal vesicle.
• He had ultrasound scan as well as CT scan which demonstrated no recurrence 3 months subsequently.
Chen et al. [18] made the ensuing conclusions:
• Cystadenoma of the seminal vesicle is extremely rare and it is easily missed in diagnosis.
• Routine digital rectal examination (DRE) is necessary and ultrasound scan and CT scan are helpful for the diagnosis of cystadenoma of seminal vesicle.
• Seminal vesiculectomy with tumour removal is an ideal option which is associated with good prognosis.
Rodrigo Aliaga et al. [19] stated the following:
• Cysstadenoma of the seminal vesicles is an extremely rare pathology.
• To their knowledge only eight cases had been reported in the literature by 1997.
Rodrigo Aliaga et al. [19] reported a new case of this benign tumour, which was bilaterally located and incidentally found during surgery.
Debansu and Vaibhav Kant [20] stated the following:
• Benign cystadenomas are the rarest tumours of the seminal vesicles (SVs).
• Only 22 cases of cystadenoma of the SVs had been noted up to 2023.
• Clinical findings and radiology imaging studies are nonspecific for the identification of cystadenoma of seminal vesicle, so the diagnosis is made based upon the final pathology examination features of the tumoral mass.
• The only curative treatment for cystadenoma of seminal vesicle is surgical resection of the lesion.
Debansu and Vaibhav Kant [20] reported the case of a cystadenoma of seminal vesicle in a 65-year-old man, who had manifested with lower urinary tract symptoms, and who was seen on radiology-imaging to have a cystic mass within his rectovesical space. He underwent surgical excision of the mass and pathology examination of the excised mass had confirmed the nature of a benign cystadenoma of the seminal vesicle. During his 6-month post-operative assessment he was doing well. Debansu and Vaibhav Kant [20] made the ensuing conclusions:
• They had reported a case of cystadenoma of seminal vesicle in a 65-year-old patient.
• Benign primary tumours including cystadenomas are the rarest ones.
• The diagnosis of cystadenoma of seminal vesicle is typically made upon the final pathology examination of the excised lesion.
• The only curative treatment is surgical resection, either by means of open or laparoscopic surgery.
Feger made the ensuing summations related to various aspects of cystadenoma of seminal vesicles: [21]
• Cystadenomas of the seminal vesicle, are a benign sub-group of mixed epithelial and stromal tumours of the seminal vesicles.
• It has been documented that benign tumours of the seminal vesicles are very rare and so are cystadenomas [22]
• Voiding difficulties or haematuria had been reported as clinical manifestations of cystadenomas of seminal vesicles. [22] [23].
• The diagnosis of cystadenomas of seminal vesicle is established based upon the typical pathological or rather histological features.
• Upon macroscopy examination, the tumours had been described as well-circumscribed tumours with a glistening or smooth surface and a multilocular cystic cut surface [24]
• Microscopically cystadenomas of the seminal vesicles are typified by columnar or cuboid epithelial cells that are encompassed by a fibrous stroma [22]. [24].
• In cases of cystadenomas of seminal vesicles, immunohistochemistry might express CA125; however, it but should be negative for prostate specific antigen (PSA) carcinoembryonic antigen (CEA), CK20 [24]
• Computed tomography (CT) scan may depict a cystic or soft tissue mass that is located between the urinary bladder and the rectum arising from one of the seminal vesicles [22] [23] [24] [25] [26]
• It had been iterated that upon prostate or pelvic MRI seminal vesicle, cystadenomas had been typified as multi-septate and well-delineated cystic masses with a well-defined capsule [22] [24] [26]
• MRI scan signal characteristics of cystadenoma of seminal vesicle had been summated as follows:
T1: mixed hyper and hypointense
T2: hyperintense with hypointense capsule
DWI: lack of diffusion restriction
DCE (Gd): delayed enhancement of the tumour capsule
• Radiology report: - It had been recommended that the radiological report should include a description of the following:
The location form and extent of the tumour should be documented
invasive features should be documented
The relation to of the seminal vesicle lesion to the prostate gland, urinary bladder and sigmoid colon should be documented or reported
• Treatment and prognosis
It has been documented that the treatment of cystadenoma of seminal vesicle includes laparoscopic or open surgical approaches, [22] and the first having the advantage of decreased rates in the development of postoperative morbidity, shorter hospitalisation and faster recovery than the latter. [22]
It has been iterated that recurrences of cystadenoma of seminal vesicle might occur on incomplete excision of the cystadenoma of seminal vesicle lesion. [24]
• History and etymology -
It had been stated that the first case of cystadenoma of seminal vesicle was probably described by R Guiteras in 1894. [25]
• Differential diagnoses.
It has been iterated that conditions which might simulate the clinical manifestation or radiology imaging features of cystadenoma of seminal vesicle include the ensuing: [22] [27]
o Seminal vesicle cyst.
o Adenocarcinoma of the seminal vesicle.
o Mixed epithelial and stromal tumours.
Conclusions
Cystadenoma of seminal vesicle is a very rare benign tumour which has been reported sporadically.
• Cystadenoma of seminal vesicle may be identified incidentally based upon radiology imaging of some asymptomatic individuals who have undergone radiology imaging for a different reason.
• Cystadenoma of seminal vesicle may manifest with non-specific symptoms including: lower urinary tract symptoms; urinary retention; haematuria; haematospermia; and infertility.
• In majority of cases of cystadenoma of seminal vesicle, the serum PSA level had tended to be low or normal; but on rare occasions serum PSA levels of some individuals afflicted by cystadenoma of seminal vesicle the serum PSA level had been reported as elevated.
• Cystadenoma of seminal vesicle has most often be unilateral but bilateral cystadenoma of the seminal vesicle has been reported occasionally.
• Effective treatment of cystadenoma of seminal vesicle could be either open seminal vesicle surgical excision or laparoscopic surgical excision of the seminal vesicle containing the tumour.
• Cystadenoma of seminal vesicle may prove difficult to differentiate from simulants of cystadenoma of the seminal vesicle that are more common lesions including: adenocarcinoma of seminal vesicle, seminal vesicle cyst and mixed epithelial and stromal tumours of the seminal vesicle.
Conflict Of Interest
Nil
Acknowledgements
Acknowledgements to The Pan African Medical Journal for granting permission for reproduction of figures and contents of their Journal article under copyright: Droit d'auteur © Mojtaba Ameli et al. The Pan African Medical Journal - ISSN 1937-8688. This is an Open Access article distributed under the terms of the Creative Commons Attribution License which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- Franca RA, Crocetto F, Pandolfo SD, et al. Cystadenoma of the seminal vesicle – Potential diagnostic pitfall: A case report and literature review. Journal of Clinical Urology. 2023;16(6):631-642.
View at Publisher | View at Google Scholar - Athanazio D. Cystadenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/prostatecystadenoma.html. Accessed February 25th, 2024.
View at Publisher | View at Google Scholar - Reikie BA, Yilmaz A, Medlicott S, Trpkov K. Mixed epithelial-stromal tumor (MEST) of seminal vesicle: a proposal for unified nomenclature. Adv Anat Pathol. 2015 Mar;22(2):113-120.
View at Publisher | View at Google Scholar - Ortiz-Rey JA, Chantada-de la Fuente D, Peteiro-Cancelo MÁ, Gómez-de María C, San Miguel-Fraile MP. Usefulness of GATA-3 as a marker of seminal epithelium in prostate biopsies. Actas Urol Esp. 2017 Nov;41(9):577-583. English, Spanish.
View at Publisher | View at Google Scholar - Ozcan A, Liles N, Coffey D, Shen SS, Truong LD. PAX2 and PAX8 expression in primary and metastatic müllerian epithelial tumors: a comprehensive comparison. Am J Surg Pathol. 2011 Dec;35(12):1837-47.
View at Publisher | View at Google Scholar - Posenato I, Caliò A, Segala D, Sgroi S, Polara A, Brunelli M, Martignoni G. Primary seminal vesicle carcinoma. The usefulness of PAX8 immunohistochemical expression for the differential diagnosis. Hum Pathol. 2017 Nov;69:123-128..
View at Publisher | View at Google Scholar - [WHO Classification of Tumours Editorial Board: Urinary and Male Genital Tumours, 5th Edition, 2022
View at Publisher | View at Google Scholar - Argun OB, Mourmouris P, Tufek İ, Saglican Y, Obek C, Kural AR. Robot-Assisted Laparoscopic Seminal Vesicle Cystadenoma Excision. J Endourol Case Rep. 2015 Dec 1;1(1):62-4.
View at Publisher | View at Google Scholar - Ameli M, Yousefzadeh N. Transvesical removal of huge seminal vesicle cystadenoma. Pan Afr Med J. 2017 Oct 17;28:149. French.
View at Publisher | View at Google Scholar - Campi R, Serni S, Raspollini MR, Tuccio A, Siena G, Carini M, Minervini A. Robot-Assisted Laparoscopic Vesiculectomy for Large Seminal Vesicle Cystadenoma: A Case Report and Review of the Literature. Clin Genitourin Cancer. 2015 Oct;13(5):e369-73.
View at Publisher | View at Google Scholar - Alan J. Wein, Louis R. Kavoussi, Alan W. Partin, Craig A. Peters Campbell-Walsh Urology 4-Volume Set 11th Edition - October 13, 2015 Page 957. cambridgescholars.com
View at Publisher | View at Google Scholar - Kaminsky A, Kania U, Ortloff P, Sperling H. Zystadenom der Samenblase als Ursache einer retrovesikalen Raumforderung [Seminal vesicle cystadenoma as the cause of a retrovesical tumor]. Urologe A. 2014 Apr;53(4):542-4. German.
View at Publisher | View at Google Scholar - Takayasu K, Harada J, Kawa G, Ota S, Sakurai T. [Transvesical Removal of Seminal Vesicle Cystadenoma]. Hinyokika Kiyo. 2015 Jul;61(7):299-303. Japanese.
View at Publisher | View at Google Scholar - Xu LW, Cheng S, Zhang ZG, Li XD. [Transvesical removal of seminal vesicle mass: a report of 5 cases]. Zhonghua Nan Ke Xue. 2009 Apr;15(4):357-9. Chinese
View at Publisher | View at Google Scholar - Baschinsky DY, Niemann TH, Maximo CB, Bahnson RR. Seminal vesicle cystadenoma: a case report and literature review. Urology. 1998 May;51(5):840-5. Do
View at Publisher | View at Google Scholar - Santos LD, Wong CS, Killingsworth M. Cystadenoma of the seminal vesicle: report of a case with ultrastructural findings. Pathology. 2001 Aug;33(3):399-402.
View at Publisher | View at Google Scholar - Lee CB, Choi HJ, Cho DH, Ha US. Cystadenoma of the seminal vesicle. Int J Urol. 2006 Aug;13(8):1138-40.
View at Publisher | View at Google Scholar - Chen J, Meng HZ, Wang CJ, Wang ZM. [Cystadenoma of the seminal vesicle: 1 case report]. Zhonghua Nan Ke Xue. 2007 Apr;13(4):345-7. Chinese.
View at Publisher | View at Google Scholar - Rodrigo Aliaga M, López Alcina E, Alonso Gorrea M, Pontones Moreno JL, Paya Roma A, Jiménez Cruz JF. Cistadenoma de vesículas seminales [Cystadenoma of seminal vesicles]. Actas Urol Esp. 1997 Jun;21(6):628-30. Spanish.
View at Publisher | View at Google Scholar - Sarkar, Debansu; Baderiya, Vaibhav Kant. Cystadenoma of seminal vesicle. Annals of Medical Science & Research 2(1):p 53-55, Jan–Apr 2023.
View at Publisher | View at Google Scholar - Feger J, Knipe H, Seminal vesicle cystadenoma. Reference article, Radiopaedia.org (Accessed on 27 Feb 2024)
View at Publisher | View at Google Scholar - Tang QZ, Lin Z, Reddy RK, Zhang ZW. Laparoscopic excision of seminal vesicle cystadenoma. Urol Case Rep. 2019 May 7;27:100906.
View at Publisher | View at Google Scholar - Kim B, Kawashima A, Ryu JA, Takahashi N, Hartman RP, King BF Jr. Imaging of the seminal vesicle and vas deferens. Radiographics. 2009 Jul-Aug;29(4):1105-21.
View at Publisher | View at Google Scholar - Kuai XP, Ding QG, Wang SY, Wu PF, Qiu JM. Rare primary seminal vesicle cystadenoma: computed tomography and magnetic resonance imaging findings. Asian J Androl. 2017 May-Jun;19(3):384-385.
View at Publisher | View at Google Scholar - Bullock KN. Cystadenoma of the seminal vesicle. J R Soc Med. 1988 May;81(5):294-5.
View at Publisher | View at Google Scholar - Reddy MN, Verma S. Lesions of the Seminal Vesicles and their MRI Characteristics. J Clin Imaging Sci. 2014 Oct 31;4:61.
View at Publisher | View at Google Scholar - [Monica B, Larosa M, Facchini F, Pozzoli G, Franceschetti I, Piscioli I. Low grade epithelial stromal tumour of the seminal vesicle. World J Surg Oncol. 2008 Sep 23;6:101.
View at Publisher | View at Google Scholar

 Clinic
Clinic
