Research Article | DOI: https://doi.org/10.31579/2835-2971/042
Assess the Risk Factors of Developing Hypoglycemia Among Term Infants Born to Diabetic Mothers
- Mona Eid Ahmed *
National Nutrition Institute, Cairo, Egypt.
*Corresponding Author: Mona Eid Ahmed, National Nutrition Institute, Cairo, Egypt.
Citation: Mona Eid Ahmed, (2024), Assess the risk factors of developing hypoglycemia among term infants born too diabetic mothers, J. Clinical Pediatrics and Mother Health, 3(6); DOI:10.31579/2835-2971/042
Copyright: © 2024, Mona Eid Ahmed. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 02 December 2024 | Accepted: 17 December 2024 | Published: 27 December 2024
Keywords: biology proficiency; biology performance; gender; Nigeria
Abstract
Objective: to assess the risk factors of developing hypoglycemia among term infants born to diabetic mothers and to characterize rates of glucose concentrations in the first 2 days of life.
Methods: A prospective study included all IDMs who were born at EL Kasr EL-Aini Hospital with exclusion of major congenital anomalies, polycythemia, respiratory distress, sepsis, asphyxia or other clinical manifestations not clearly attributed to hypoglycemia. Blood glucose level was measured immediately after delivery and over 48 hours, taking into consideration maternal data before and during pregnancy and neonatal data including gestational age, sex, body weight, apgar score, clinical manifestations of hypoglycemia and nutrition of the newborn.
Results: Hypoglycemia at 0 hour was more among those born to uncontrolled diabetic mothers, mothers who were on insulin therapy (either GDM-A2 or IDDM), severe hypoglycemia after birth and on the 1st day of life was more common in neonates that were born to hypertensive, uncontrolled diabetic mothers as well as to mothers on insulin therapy. The mean of glucose values on the 2nd day of life showed improvement for the majority of the neonates.
Conclusions: It seems that infants born to diabetic mothers tend to have very high rates of hypoglycemia on the first day of life when a higher cut-off point is used. When considering glucose values in newborn infants, it is necessary to distinguish between ‘common’ glucose values that can be low not only among high-risk infants and values of infants born to diabetic mothers. Then it must be decided whether these values should be accepted as ‘normal’ or, as suggested in a number of recent studies. Whether they indicate a correlation between hypoglycemia (even moderate and asymptomatic) and unfavorable outcome, leading to a recommendation to maintain higher glucose levels.
Introduction
The majority of fetal glucose is obtained from maternal circulation through facilitated diffusion, maintaining fetal glucose levels during the second and third trimesters (Lord and De León, 2024). Upon severance of the umbilical cord, a maternal cutoff occurs, necessitating the newborn's prompt engagement in glycogenolysis of hepatic reserves, gluconeogenesis, and the assimilation of exogenous nutrients (Rosenfeld and Paul Thornton, 2023). Hypoglycemia poses a significant issue, resulting in numerous severe short- and long-term complications, including convulsions, apnea, cyanosis, and cognitive impairment. Blood glucose levels in term neonates exhibit considerable variability, with values below 30 mg/dl commonly observed due to the underdevelopment of gluconeogenesis and ketogenesis (Adamkin, 2017; De Rose et al. 2024).
The reported incidence of hypoglycemia fluctuates according on its definition, with estimates indicating it occurs in around 25-50% of newborns born to diabetic mothers and 15-25% of infants born to mothers with gestational diabetes; however, only a minor fraction exhibit symptom (Suraiya et al. 2018). Insulin resistance is a typical occurrence that arises during the second trimester of pregnancy and subsequently escalates to levels comparable to those observed in non-pregnant individuals with type 2 diabetes; it is believed to ensure glucose availability for the developing fetus (Andrews et al. 2024). Women with gestational diabetes mellitus exhibit insulin resistance that cannot be mitigated by augmented production in the pancreatic β-cells (Nazarpour et al. 2024).
Placental hormones, together with a lower contribution from increased fat deposits, appear to facilitate insulin resistance during pregnancy. Cortisol and progesterone are the primary factors, but human placental lactogen, prolactin, and estradiol also play a role (Handwerger and Freekman, 2000; Schenk et al. 2024). Variable maternal hyperglycemia leads to fetal hyperglycemia, pancreatic B-cell hyperplasia, and hyperinsulinemia. Postnatally, hyperinsulinemia continues, as indicated by increased utilization of exogenous glucose and reduced endogenous glucose synthesis. Additionally, free fatty acids and ketones are diminished (Klaus and Fanaroff, 2001; Mittal et al. 2024).
The pathogenetic basis of neonatal hypoglycemia in infants of diabetic mothers (IDMs) is elucidated by maternal hyperglycemia as described by Pederson. The fetal hyperinsulinism hypothesis posits a correlation between fetal macrosomia, elevated HbA1c levels in maternal and cord blood, and neonatal hypoglycemia. Additionally, the relationship between increased cord blood C-peptide or immunoreactive insulin levels and hypoglycemia indicates that regulating maternal blood glucose during the final trimester may reduce the occurrence of neonatal hypoglycemia in infants of diabetic mothers (De Rose et al. 2024).
In typical circumstances, the adrenergic response occurring immediately post-birth inhibits insulin secretion and promotes glucagon release, thereby augmenting gluconeogenesis and ketogenesis. This results in a reversal of the insulin/glucagon ratio shortly after birth, constituting a normal physiological occurrence. Consequently, a post-delivery glucose nadir is attained within 30 to 90 minutes after birth, followed by an autonomous recovery before 3 to 4 hours of age (Giouleka et al. 2023). In infants born to diabetic mothers, the inversion of the ratio is delayed, resulting in more severe and prolonged hypoglycemia (Rennie and Roberton, 2002). The aim of this study is to evaluate the risk factors for hypoglycemia in term children born to diabetic mothers and to delineate glucose concentration levels over the first two days of life.
Patients And Methods
Study design
This is a prospective controlled non-randomized study conducted at Kasr El-Aini Hospital Cairo University. 100 full-term babies more than 37 weeks gestation born to diabetic mothers were enrolled in our study after written concern form the parents or their cavere.
Patient’s criteria
Inclusion Criteria:
Maternal data: included maternal age, delivery mode, presence of meconium in aminiotic fluid,maternal diseases: (Gestational diabetes (GDM-A0), (GDM-A1), (GDM-A2) and IDDM, The glycemic state of the mother and whether it is controlled or not during pregnancy, and maternal hypertension.
Neonatal Dat: included detailed history and full clinical examination of the newborn including:Gestational age and birth weight (AGA, SGA and LGA). Apgar score at 1 min, 5min. Estimate the perfusion of the infant by capillary refill time Neurological manifestations of hypoglycemia in the form of jitteriness, lethargy, convulsions or coma.
Exclusion Criteria:
Major congenital malformations that affect the neonate.
Polycythemia with hematocrite >70gm% and HB%>21gm%.
Respiratory distress that are not clearly attributed to hypoglycemia.
Asphyxia.
Sepsis. Whole blood glucometer (whole blood glucose monitoring system) is (in vitro diagnostic test) which is designed for self-test glucose monitoring using fresh capillary whole blood from fingertip. It is a rapid test and an easy test that gives a rapid idea about blood glucose level either within normal range, high or low that helps rapid intervention especially in neonates that are at risk of developing hypoglycemia.
The glucometer used in this study was called Optime-x-ceed made in china. Each glucometer had its test strips and its code which were specific for the device.Each test strip and lancet was used for a single measurement and reading to follow infection control rules.
Blood glucose level was measured using whole blood glucometer (Optime x-ceed) as it has the advantage of being bedside and helps rapid intervention than plasma glucose levels as there is time elapsed between withdrawing of the sample and the results. We measured blood glucose levels at 0, 2, 4, 6, 8 hrs and every 8 hours for 48 hours to find out the rates of hypoglycemia and the symptoms accompanying the corresponding blood glucose levels. Oral feeding was initiated during the first 2-4 h of life and thereafter every 2-3 has requested.Infants with glucose values lower than 30mg/dl and those with repeated values in the range of 30-39 mg/dl will be treated with continuous intravenous glucose after an intravenous bolus of 10% glucose 2 ml/Kg (Maayan-metzger et al. 2009).
Statistical analysis
All data were compiled and analyzed using SPSS version 25 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as means (± standard deviation [SD]), and categorical variables are presented using relative frequency distributions and percentages. Categorical data were analyzed using the chi-square (X2) test, Fishers exact test. Statistical significance was established at p ≤ 0.05.
Results
The patients were categorized into two groups, A and B, based on post-natal glucose levels assessed at 0 hours, utilizing a cut-off point of 47 mg/dl instead of 40 mg/dl to mitigate false-negative results due to elevated plasma glucose concentrations. Group (A) comprised infants with glucose levels below 47 mg/dl, while group (B) consisted of neonates with glucose levels equal to or beyond 47 mg/dl. The average mother age and standard deviation were 32.29 ± 6.01 years. Group (A) had a mean age of 32.32±5.88 years, while group (B) had a mean age of 32.16±6.51 years. Among 100 diabetic women, 36 had gestational diabetes (GDM-A0) without insulin therapy or dietary management (36.0%), 47 were receiving insulin therapy (GDM-A2) (47%), and 16 were diagnosed with insulin-dependent diabetes mellitus (IDDM) (16%). Only one case exhibited gestational diabetes managed with dietary intervention (GDM-A1).
In terms of Maternal Data, the incidence of gestational diabetes type GDM-A0 was higher in group (A) with 26 cases, compared to only 10 instances in group (B). Similarly, GDM-A2 was more prevalent in group (A) with 41 cases, in contrast to 6 cases in group (B). Group (A) had 9 cases of IDDM moms, whereas group (B) included 7 cases. GDM-A1 was identified in one instance within group (B). The difference was statistically significant, with a P value of 0.01. Group (A) had sixty-nine neonate cases with mothers suffering from uncontrolled diabetes, whereas group (B) had fifteen cases, resulting in a statistically significant difference of P=0.001. The comparison of maternal data between diabetic women in groups (A) and (B) concerning mode of delivery, meconium-stained amniotic fluid, hypertension, and insulin therapy yielded statistically negligible results (Table 1).
Maternal data | Group (A) N = 76 | Group(B) N = 24 | P value | |||
N | % | N | % | |||
Mode of Delivery | CS (N = 98) | 74 | 97.4 | 24 | 100.0 | 0.900 |
N.V.D (N = 2) | 2 | 2.6 | 0 | 0.0 | ||
Meconium-stained amniotic fluid | Present (N = 6) | 3 | 3.9 | 3 | 12.5 | 0.1400 |
Absent (N = 94) | 73 | 96.1 | 21 | 87.5 | ||
Hypertension | Present (N = 30) | 23 | 30.3 | 7 | 29.2 | 0.900 |
Absent (N = 70) | 53 | 69.7 | 17 | 70.8 | ||
DM type | GDM-A0 (N =36) | 26 | 34.2 | 10 | 41.6 | 0.010* |
GDM-A1 (N=1) | 0 | 0.0 | 1 | 4.2 | ||
GDM-A2 (N=47) | 41 | 53.9 | 6 | 25.0 | ||
IDDM (N = 16) | 9 | 11.8 | 7 | 29.2 | ||
Control of maternal diabetes | Controlled (N = 16) | 7 | 9.2 | 9 | 37.5 | 0.001* |
Uncontrolled (N = 84) | 69 | 90.8 | 15 | 62.5 | ||
Insulin Therapy during pregnancy | Yes (N =63) | 50 | 65.8 | 13 | 54.2 | 0.330 |
No (N = 37) | 26 | 34.2 | 11 | 45.8 | ||
Table (1): The maternal data in the 2 groups.
Regarding glucose measurements at 0 hours and maternal data, it was observed that 53.8% of severely hypoglycemic cases (<30>47 mg/dl), 85.7% of mildly hypoglycemic cases (40-46 mg/dl), and 96.7% of moderately hypoglycemic cases (30-39 mg/dl) were born to normotensive mothers. The difference was statistically significant with a P-value of 0.001. In the comparison of glucose measurements at 0 hours and the control of maternal diabetes, it was shown that 87.2% of severely hypoglycemia cases (<30>(Table 2).
Maternal data: |
| Glucose measurement at 0 hour |
P value | ||||||||
| ≥ 47 N = 24 | 40 - 46 N = 7 | 39 - 30 N = 30 | < 30> N = 39 | |||||||
| N | % | N | % | N | % | N | % | |||
Mode of Delivery | CS (N = 98) |
| 24 | 100.0 | 7 | 100.0 | 28 | 93.3 | 39 | 100.0 | 0.190 |
N.V.D (N = 2) |
| 0 | 0.0 | 0 | 0.0 | 2 | 6.7 | 0 | 0.0 | ||
Me conium-stained amniotic fluid | Present (N = 6) |
| 3 | 12.5 | 0 | 0.0 | 0 | 0.0 | 3 | 7.7 | 0.225 |
Absent (N = 94) |
| 21 | 87.5 | 7 | 100.0 | 30 | 100.0 | 36 | 92.3 | ||
Hypertension | Present (N = 30) |
| 7 | 29.2 | 1 | 14.3 | 1 | 3.3 | 21 | 53.8 | 0.001* |
Absent (N = 70) |
| 17 | 70.8 | 6 | 85.7 | 29 | 96.7 | 18 | 46.2 | ||
DM status | Controlled (N=16) |
| 9 | 37.5 | 2 | 28.6 | 0 | 0.0 | 5 | 12.8 | 0.002* |
Uncontrolled (N=84) |
| 15 | 62.5 | 5 | 71.4 | 6 | 100.0 | 34 | 87.2 | ||
Insulin Therapy | Yes (N=63) |
| 13 | 54.2 | 3 | 42.9 | 13 | 43.3 | 34 | 87.2 | 0.001* |
No (N=37) |
| 11 | 45.8 | 4 | 57.1 | 17 | 56.7 | 5 | 12.8 | ||
DM type | GDM-A0 (N =36) |
| 10 | 41.7 | 4 | 57.1 | 17 | 56.7 | 5 | 12.8 | 0.001* |
GDM-A1 (N=1) |
| 1 | 4.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
GDM-A2 (N=47) |
| 6 | 25.0 | 3 | 42.9 | 12 | 40.0 | 26 | 66.7 | ||
IDDM (N = 16) |
| 7 | 29.2 | 0 | 0.0 | 1 | 3.3 | 8 | 20.5 | ||
Table (2): Glucose measuremnt at 0 hour in relation to maternal data.
Concerning maternal data, the kind of gestational diabetes: Among the LGA neonates, 31 (47%) were born to mothers with GDM-A2, 28 (42.4%) to those with GDM-A0, and 7 (10.6%) to mothers with IDDM, with no statistical significance seen (P=0.06).Upon comparing the relevance of gestational age and birth weight with maternal data (mode of delivery, meconium-stained amniotic fluid, hypertension, insulin therapy, diabetes type, and diabetes management), no statistical significance was observed among the various groups.In the comparison of maternal diabetes management, 55 (83.3%) LGA and 5 (83.3%) SGA neonates were delivered by moms with uncontrolled diabetes, which demonstrated no statistical significance. Furthermore, the comparison of gestational age and birth weight with neonatal data, including initial glucose level and subsequent glucose bolus followed by infusion, demonstrated statistical insignificance (Table 3).
Neonatal data | AGA N = 28 | LGA N = 66 | SGA N = 6 | P | ||||
N | % | N | % | N | % | |||
Sex | Male (N = 54) | 10 | 35.7 | 42 | 63.6 | 2 | 33.3 | 0.02* |
Female (N = 46) | 18 | 64.3 | 24 | 36.4 | 4 | 66.7 | ||
Breast feeding | Yes (N = 31) | 15 | 53.6 | 16 | 24.2 | 0 | 0.0 | 0.001* |
No (N = 69) | 13 | 46.4 | 50 | 75.8 | 6 | 100.0 | ||
Formula | Yes (N = 20) | 2 | 7.1 | 17 | 25.8 | 1 | 16.7 | 0.110 |
No (N = 80) | 26 | 92.9 | 49 | 74.2 | 5 | 83.3 | ||
Glucose followed by infusion | Yes (N = 72) | 16 | 57.1 | 51 | 77.3 | 5 | 83.3 | 0.110 |
No (N = 28) | 12 | 42.9 | 15 | 22.7 | 1 | 16.7 | ||
Serum glucose at 0 hr | <47 xss=removed> | 19 | 67.9 | 53 | 80.3 | 4 | 66.7 | 0.370 |
≥ 47 (N = 24) | 9 | 32.1 | 13 | 19.7 | 2 | 33.3 | ||
Table (3): Appropriateness of gestational age and birth weight in relation to neonatal data.
Also, mothers with GDM-A0, GDM-A2, IDDM had uncontrolled diabetes (97.2%), (80.9), (68.8%) respectively and that was statistically significant with P=0.001 (Table 4). When comparing the type of maternal diabetes and the maternal data (mode of delivery, me conium-stained amniotic fluid and hypertension all proved to be statistically insignificant (Table 5).
Maternal Data | GDM-A0 N = 36 | GDM-A1 N = 1 | GDM-A2 N = 47 | IDDM N = 16 |
| |||||
N | % | N | % | N | % | N | % | |||
Mode of Delivery | CS (N = 98) | 34 | 94.4 | 1 | 100.0 | 47 | 100.0 | 16 | 100.0 | 0.30 |
N.V.D (N = 2) | 2 | 5.6 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
Me conium-stained amniotic fluid | Present (N = 6) | 4 | 11.1 | 0 | 0.0 | 0 | 0.0 | 2 | 12.5 | 0.11 |
Absent (N = 94) | 32 | 88.9 | 1 | 100.0 | 47 | 100.0 | 14 | 87.5 | ||
Hypertension | Present (N = 30) | 10 | 27.8 | 0 | 0.0 | 17 | 36.2 | 3 | 18.7 | 0.50 |
Absent (N = 70) | 26 | 72.2 | 1 | 100.0 | 30 | 63.8 | 13 | 81.3 | ||
DM status | Controlled (N=16) | 1 | 2.8 | 1 | 100.0 | 9 | 19.1 | 5 | 31.2 | 0.001* |
Uncontrolled (N=84) | 35 | 97.2 | 0 | 0.0 | 38 | 80.9 | 11 | 68.8 | ||
Insulin Therapy | Yes (N=63) | 0 | 0.0 | 0 | 0.0 | 47 | 100.0 | 16 | 100.0 | 0.001* |
No (N=37) | 36 | 100.0 | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 | ||
Table (4): Type of maternal diabetes and neonatal data.
Maternal Data | GDM Type with gestational age and birth weight |
P value | ||||||||
GDM-A0 N = 36 | GDM-A1 N = 1 | GDM-A2 N = 47 | IDDM N = 16 | |||||||
N | % | N | % | N | % | N | % | |||
Sex | Male (N=54) | 24 | 66.7 | 0 | 0.0 | 21 | 44.7 | 9 | 56.3 | 0.15 |
Female (N=46) | 12 | 33.3 | 1 | 100.0 | 26 | 55.3 | 7 | 43.8 | ||
Glucose followed by infusion | Yes (N=72) | 22 | 61.1 | 0 | 0.0 | 38 | 80.9 | 12 | 75.0 | 0.08 |
No (N=28) | 14 | 38.9 | 1 | 100.0 | 9 | 19.1 | 4 | 25.0 | ||
Glucose level at 0 hr | Group A (N=76) | 26 | 72.2 | 0 | 0.0 | 41 | 87.2 | 9 | 56.2 | 0.01* |
Group B (N=24) | 10 | 27.8 | 1 | 100.0 | 6 | 12.8 | 7 | 43.8 | ||
Gestational Age | AGA (N=28) | 8 | 22.2 | 1 | 100.0 | 13 | 27.6 | 6 | 37.5 | 0.06 |
LGA (N=66) | 28 | 77.8 | 0 | 0.0 | 31 | 66.0 | 7 | 43.7 | ||
SGA (N=6) | 0 | 0.0 | 0 | 0.0 | 3 | 6.4 | 3 | 18.8 | ||
Table (5): Type of maternal diabetes with the neonatal data:
Moreover, a comparison of maternal diabetes management with neonatal outcomes revealed that neonates receiving a glucose bolus followed by infusion were predominantly those born to mothers with uncontrolled diabetes (79.8%), whereas a lesser proportion were born to mothers with controlled diabetes (31.2%). This demonstrated statistical significance with a P value of 0.001. Upon comparing maternal diabetes management with glucose levels at baseline, it was observed that 82.1% of neonates in group A were born to mothers with uncontrolled diabetes, whereas 56.2% in group B were born to moms with controlled diabetes. This was statistically significant with P=0.001. (Table 6).
Neonatal data | DM status |
P value | ||||
Controlled N=16 | Uncontrolled N=84 | |||||
N | % | N | % | |||
Gestational age/weeks | AGA (N=28) | 4 | 25.0 | 24 | 28.5 | 0.950 |
LGA (N=66) | 11 | 68.8 | 55 | 65.5 | ||
SGA (N=6) | 1 | 6.2 | 5 | 6.0 | ||
Glucose followed by infusion | Yes (N=72) | 5 | 31.2 | 67 | 79.8 | 0.001* |
No (N=28) | 11 | 68.8 | 17 | 20.2 | ||
Glucose level at 0 hr | <47 N=76)> | 7 | 43..8 | 69 | 82.1 | 0.001* |
Table (6): Neonatal data in controlled and uncontrolled diabetes.
In our study, the comparison of glucose measurements on day 1 with maternal data revealed that 76.7% of hypertensive mothers delivered hypoglycemic neonates (glucose <30 P=0.001. P=0.001.>(Table 7).
Maternal data | Glucose measurement on day 1 |
P value | ||||||||
≥ 47 N = 19 | 40 - 46 N = 8 | 39 - 30 N = 31 | < 30> N = 42 | |||||||
N | % | N | % | N | % | N | % |
| ||
Mode of Delivery | CS (N = 98) | 19 | 19.4 | 8 | 8.2 | 29 | 29.6 | 42 | 42.8 | 0.200 |
N.V.D (N = 2) | 0 | 0.0 | 0 | 0.0 | 2 | 100.0 | 0 | 0.0 | ||
Me conium-stained amniotic fluid | Present (N = 6) | 2 | 33.3 | 0 | 0.0 | 0 | 0.0 | 4 | 66.7 | 0.250 |
Absent (N = 94) | 17 | 18.1 | 8 | 8.5 | 31 | 33.0 | 38 | 40.4 | ||
Hypertension | Present (N = 30) | 4 | 13.3 | 1 | 3.3 | 2 | 6.6 | 23 | 76.7 | 0.001* |
Absent (N = 70) | 15 | 21.4 | 7 | 10.0 | 29 | 41.4 | 19 | 27.14 | ||
DM status | Controlled (N=16) | 9 | 56.25 | 2 | 12.5 | 0 | 0.0 | 5 | 31.2 | 0.001* |
Uncontrolled (N=84) | 10 | 11.9 | 6 | 7.1 | 31 | 37.0 | 37 | 44.0 | ||
Insulin Therapy | Yes (N=63) | 11 | 17.5 | 3 | 4.8 | 13 | 20.6 | 36 | 57.1 | 0.001* |
No (N=37) | 8 | 21.6 | 5 | 13.5 | 18 | 48.6 | 6 | 16.2 | ||
Dm type | GDM-A0 (N =36) | 7 | 19.4 | 5 | 13.9 | 18 | 50.0 | 6 | 16.7 | 0.001* |
GDM-A1 (N=1) | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||
GDM-A2 (N=47) | 6 | 12.7 | 3 | 6.3 | 12 | 38.7 | 26 | 61.9 | ||
IDDM (N = 16) | 5 | 31.25 | 0 | 0.0 | 1 | 6.25 | 10 | 62.5 | ||
Table (7): Glucose measurement on day 1 in relation to maternal data.
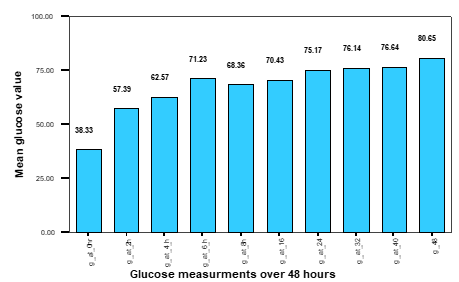
Figure (1): The mean glucose values at 0,2,4,6,8,16,24,32,40 and 48 hrs in 100 full-term neonates born to diabetic mothers and their improvement over 48 hours. The mean glucose value at 0 hour was 38.330 ± 21.33. When comparing the glucose measurement on day 1 and gestational age and birth-weight, it was found that (84.9%) of LGA neonates and (100%) of SGA had shown hypoglycemia on the first day of life.
Discussion
Historically, infants born to diabetes mothers have been seen as having an elevated risk for symptomatic hypoglycemia compared to other newborns. The impact of intensified evaluation of pregnant women for glucose intolerance, together with rigorous glucose monitoring and therapy during gestation, on the infant's risk of hypoglycemia remains ambiguous (Van Howke and Storms, 2006). Currently, 3-10% of pregnancies are impacted by gestational diabetes, with the majority of these instances associated with impaired glucose management throughout pregnancy. Approximately 3% to 5% of patients with gestational diabetes mellitus (GDM) possess pre-existing type 1 or type 2 diabetes, with pregnancy serving as the initial occasion for diagnostic testing (Parritz and Cloherty, 2008). Infants of diabetes mothers are often healthy and benefit from contemporary obstetrical and neonatal care; yet, they remain susceptible to problems.The risk is correlated with the duration, severity, and management of the mother's diabetes (Rudolph et al. 2003).In evaluating glucose levels in neonates, it is essential to differentiate between 'normal' glucose values, which may be low in both high-risk infants and those born to diabetes moms. It must be determined whether these levels should be regarded as 'normal' or, as indicated in several recent research. The findings suggest a link between hypoglycemia, including moderate and asymptomatic cases, and adverse outcomes, prompting a suggestion to sustain elevated glucose levels (Maayan-Metzger et al. 2009).
In this study, a cut-off points of ≥47 mg/dl was employed, as the glucometer does not adjust for the established discrepancy between whole blood and plasma glucose concentrations (with plasma glucose exhibiting higher levels). Consequently, the 47 mg/dl threshold was selected instead of the more frequently utilized 40 mg/dl for defining hypoglycemia, to mitigate the risk of false-negative results that could pose safety concerns. At this stage, we discovered that over 75% of neonates born to diabetic moms exhibited hypoglycemia (defined as <47>
In contrast to our findings, Maayan-Metzger et al. (2009), in their study involving retrospective analysis of 576 infants born to diabetes mothers, calculated that around half of the neonates had comparable rates of hypoglycemia when applying the same threshold. Van Howe and Storms (2006) reported reduced hypoglycemia rates in infants of diabetic mothers when employing a lower threshold (<40>Agrawal et al. (2000) observed that 47% of the thirty-eight term newborns investigated exhibited hypoglycemia, utilizing a cut-off point of less than 40 mg/dl.Using a comparable cutoff criterion to our study (≥47 mg/dl), the incidence was 71%. In contrast to our findings, Van Howe and Storms (2006) reported reduced rates of hypoglycemia in infants of diabetic mothers (IDMs) when employing a lower cut-off point (<40>Van Howke and Storms (2006) reported a reduced incidence of severe hypoglycemia, noting that 16.6% of the 66 examined infants of diabetic mothers (IDMs) experienced severe hypoglycemia soon after birth. Maayan-Metzger et al. (2009) revealed that the incidence of severe hypoglycemia was under 4% among the neonates tested on their first day of life.
In the present study, 80.3% of hypoglycemic newborns were asymptomatic, with no cases of convulsions or coma reported. Likewise, Maayan-Metzger et al. (2009) noted that no infants had significant coma or convulsions. Van Howke and Storms (2006) observed that none of the 66 infants who underwent blood glucose assessments developed symptomatic hypoglycemia.Numerous investigations have been conducted to elucidate the neurodevelopmental outcomes of neonatal hypoglycemia. McKinlay et al. (2018) demonstrated that asymptomatic hypoglycemia was formerly deemed clinically insignificant; nevertheless, the presence of aberrant electroencephalograms and sensory evoked potentials in asymptomatic hypoglycemic babies has called this assumption into question. Furthermore, Stenninger et al. (2008) revealed that school-age children of diabetes mothers who experienced recurrent neonatal asymptomatic hypoglycemia (BGL < 27>Singh et al. (1991) discovered that 94% of the 107 asymptomatic and symptomatic infants with hypoglycemia exhibited normal developmental outcomes at follow-up.
The majority of hypoglycemia neonates, 90.8%, were born to women with uncontrolled diabetes, in contrast to 62.5% in group (B), with this difference being statistically significant (P value = 0.00). This resulted from variable maternal hyperglycemia caused by insulin resistance in uncontrolled diabetic pregnancies, leading to fetal hyperglycemia, pancreatic B-cell hyperplasia, and hyperinsulinism. Following birth, the maternal impact diminished, resulting in persistent hyperinsulinemia, which subsequently caused neonatal hypoglycemia (Klaus and Fanar off, 2001). Consistent with our findings, Van Howke and Storms (2006) conducted research at Marquette General Hospital in Michigan, aimed at identifying characteristics that contribute to neonatal hypoglycemia in infants born to diabetes mothers. The study of 66 neonates revealed that the incidence of symptomatic hypoglycemia seems reduced with stricter management of gestational diabetes. Conversely, Mayan – Metzger et al. (2009) conducted a comparable trial and discovered that even well-managed maternal diabetes did not avert newborn hypoglycemia. Agrawal et al. (2000) underscored that effective clinical and potentially laboratory glycemic management during pregnancy and delivery did not avert hypoglycemia in the neonate. The comparison of glucose levels at 0 hours with gestational age, birth weight, and sex was statistically insignificant. The research conducted by Sarkar et al. in 2003, which determined that birth weight, gestational age, sex, and maternal HbA1c did not forecast low glucose levels during initial screening, corroborated our findings.
Nonetheless, a comparison of glucose measurements on day one with gestational age and birth weight revealed that 84.8% of LGA neonates and all SGA neonates had hypoglycemia on their first day of life. This aligns with the findings of Maayan-Metzger et al., 2009, which indicated that hypoglycemia is more prevalent in LGA and SGA newborns. The heightened risk associated with larger infants and younger moms may indicate inadequate management of diabetes during pregnancy (Van Howke and Storms, 2006). Large for gestational age (LGA) newborns indicate inadequate management of gestational diabetes throughout pregnancy, leading to fetal hyperinsulinemia and macrosomia; hence, upon cessation of maternal insulin, hyperinsulinemia causes hypoglycemia. SGA newborns exemplify inadequate management of pre-diabetes, leading to vasculopathy and reduced glycogen and lipid reserves, which culminates in hypoglycemia within the initial 12 to 24 hours of life (Rennine and Roberton, 2002).
In our study, only 1 case was born to controlled GDM-A1 mother and did not experience hypoglycemia.In the study done by Sarkar et al., 2003, they proved that infants of gestational diabetes mellitus (GDM)-A1 women are unlikely to experience the marked excursion in maternal glucose levels that may characterize insulin-requiring GDM (class-A2) or insulin-dependent diabetes (IDDM).
Our study revealed that 65.8% of hypoglycemic neonates (<47>Maayan-Metzger et al. (2009) calculated that severe hypoglycemia was more prevalent in the same cohort. A notable correlation between maternal hypertension and severe hypoglycemia incidents, which accounted for 76.7% of hypertensive mothers, was observed on the first day of life.It was determined that 55.3% of GDM-A2 moms and 62.5% of IDDM women delivered severely hypoglycemia neonates on the first day of life. Sarkar et al. (2003) and Maayan-Metzger (2009) found that maternal hypertension substantially linked with newborn hypoglycemia, in addition to the type and control of maternal diabetes, which aligns with our findings.Numerous research have disclosed alarming findings concerning the consequences of newborn hypoglycemia. Prolonged or severe hypoglycemia (glucose < 18>(Auer, 2004). Less severe hypoglycemia has been demonstrated to induce sensor-evoked potential anomalies in children (Maayan Metzger, 2009).
Conclusions
It seems that infants born to diabetic mothers tend to have very high rates of hypoglycemia on the first day of life when a higher cut-off point is used. When considering glucose values in newborn infants, it is necessary to distinguish between ‘common’ glucose values that can be low not only among high-risk infants and values of infants born to diabetic mothers. Then it must be decided whether these values should be accepted as ‘normal’ or, as suggested in a number of recent studies. Whether they indicate a correlation between hypoglycemia (even moderate and asymptomatic) and unfavorable outcome, leading to a recommendation to maintain higher glucose levels.
References
- Adamkin DH. Neonatal hypoglycemia. Semin Fetal Neonatal Med. 2001;22(1):36-4 .
View at Publisher | View at Google Scholar - Andrews C, Maya J, Schulte CC, Hsu S, Thaweethai T, James KE, Halperin J, Powe CE, Sen S. Risk of Neonatal Hypoglycemia in Infants of Mothers with Gestational Glucose Intolerance. Diabetes Care. 2024 Jul 1;47(7):1194-201.
View at Publisher | View at Google Scholar - Auer RN. Hypoglycemic brain damage. Meta Brain Dis 2004; 19: 169–175.
View at Publisher | View at Google Scholar - De Rose DU, Perri A, Maggio L, Salvatori G, Dotta A, Vento G, Gallini F. Neonatal hypoglycemia and neurodevelopmental outcomes: Yesterday, today, tomorrow. European Journal of Pediatrics. 2024 Mar;183(3):1113-9.
View at Publisher | View at Google Scholar - De Rose DU, Perri A, Maggio L, Salvatori G, Dotta A, Vento G, Gallini F. Neonatal hypoglycemia and neurodevelopmental outcomes: Yesterday, today, tomorrow. European Journal of Pediatrics. 2024 Mar;183(3):1113-9.
View at Publisher | View at Google Scholar - Giouleka S, Gkiouleka M, Tsakiridis I, Daniilidou A, Mamopoulos A, Athanasiadis A, Dagklis T. Diagnosis and management of neonatal hypoglycemia: a comprehensive review of guidelines. Children. 2023 Jul 14;10(7):1220.
View at Publisher | View at Google Scholar - Handwerger S. and Freemark M. The roles of placental growth hormone and placental lactogen in the regulation of human fetal growth and development. J Pediatr Endocrinol Metab; 2000, 13:343–356.
View at Publisher | View at Google Scholar - Klaus M. and Fanaroff A. Problems in Metabolic Adaptation. Glucose, Calcium and Magnesium. Care of the High-Risk Neonate, 1st edition; 2001, 11: 301-309.
View at Publisher | View at Google Scholar - Lord K, De León DD. Approach to the Neonate with Hypoglycemia. The Journal of Clinical Endocrinology & Metabolism. 2024 Sep;109(9): e1787-95.
View at Publisher | View at Google Scholar - Maayan -Metzger A., Lubin D. and Kuint J. Hypoglycemia rates among term infants born to diabetic mothers, Neonatology; 2009, 96:80-85.
View at Publisher | View at Google Scholar - McKinlay CJ, Alsweiler JM, Ansell JM, Anstice NS, Chase JG, Gamble GD, et al. CHYLD Study Group. Neonatal Glycemia and Neurodevelopmental Outcomes at 2 Years. N Engl J Med 2015; 373: 1507-18
View at Publisher | View at Google Scholar - Mittal M, Gupta AK, Kapoor S. Molecular mechanisms underlying congenital hyperinsulinemia of infancy and its relevance to management–A review. Journal of Pediatric Endocrinology and Diabetes. 2024 Aug 10;4(1):9-20.
View at Publisher | View at Google Scholar - Nazarpour S, Simbar M, Kiani Z, Khalaji N, Khorrami Khargh M, Naeiji Z. The relationship between quality of life and some mental problems in women with gestational diabetes mellitus (GDM): a cross-sectional study. BMC psychiatry. 2024 Dec;24(1):1-2.
View at Publisher | View at Google Scholar - Parritz A. and Cloherty J. Diabetes Mellitus. Manual of neonatology; 2008, 2A:9-19.
View at Publisher | View at Google Scholar - Rennie J. and Roberton NRC. Disorders of Glucose Homeostasis. A manual of Neonatal Intensive Care; 2002, (17): 283- 295.
View at Publisher | View at Google Scholar - Rosenfeld Elizabeth and Thornton S. Hypoglycdmia in neonates, infants 7 children. Endotext NIH, National Library of medicine, 2023.
View at Publisher | View at Google Scholar - Rudolph CD et al. What are the potential complications infants of Diabetic mothers may have? Rudolph’s pediatrics, 21st edition: 2003, 124-127.
View at Publisher | View at Google Scholar - Schenk S, Ravussin Y, Lacroix A, Quansah DY, Puder JJ. Weight Categories, Trajectories, Eating Behavior, and Metabolic Consequences during Pregnancy and Postpartum in Women with GDM. Nutrients. 2024 Feb 18;16(4):560.
View at Publisher | View at Google Scholar - Singh M. et al. Neur-developmental outcome of asymptomatic and symptomatic babies with neonatal hypoglycemia. Indian J Med Res; 1991, 94:6-10.
View at Publisher | View at Google Scholar - SPSS (Statistical Package for Social Science, Computer Software (Version 15, USA) on an IBM, PC Computer (1994).
View at Publisher | View at Google Scholar - Stenninger, R Flink, B Eriksson, C Sahlèn. Long term neurological dysfunction and neonatal hypoglycaemia after diabetic pregnancy E. Arch Dis Child Fetal Neonatal Ed 1998; 79:174–179
View at Publisher | View at Google Scholar - Suraiya Begum, Sanjoy K. Dey,1 and Kanij Fatema. Neonatal Glycemic Status of Infants of Diabetic Mothers in a Tertiary Care Hospital.Indian J Endocrinol Metab. 2018; 22(5): 621–626.
View at Publisher | View at Google Scholar - Van Howe RS and Storms MR. Hypoglycemia in infants of diabetic mothers: experience in a rural hospital. Am J Perinatol 2006, 23: 105–110.
View at Publisher | View at Google Scholar

 Clinic
Clinic
